Guide to Are You Prepared Chronic Kidney Disease
Understand the risks, symptoms, and essential preparations for managing Chronic Kidney Disease (CKD). Learn about lifestyle changes, early detection, and treatment options to protect your kidney health.

_0.webp?tr=q-80,f-webp,w-350,dpr-2,c-at_max 700w)
Introduction
Chronic kidney disease is common, often silent, and importantly manageable when you’re prepared. Your kidneys filter blood, balance fluids and minerals, and help control blood pressure. But early kidney disease rarely causes obvious symptoms. That’s why knowing your risks, testing on time, and understanding your numbers can make a life-changing difference.
This guide shows you how to get prepared for kidney disease in practical, step-by-step ways. You’ll learn who should be screened and when, how CKD is diagnosed and staged, which daily habits protect your kidneys, and which medicines can slow progression. We’ll also cover red flags that deserve urgent attention, a simple preparedness checklist, and how to plan for emergencies so your kidney care stays on track. Wherever you are in the journey—preventing problems, managing early stages, or planning ahead—this prepared approach will help you protect kidney health today and for the long term.
If symptoms persist beyond two weeks or you’re worried about new swelling, breathlessness, or sudden changes in urination, consult a doctor online with Apollo 24|7 for further evaluation.
CKD in a Snapshot: What It Is and Why Preparedness Matters
Chronic kidney disease (CKD) means your kidneys are damaged or not filtering blood as well as they should for three months or longer. It’s common about 15% of US adults have CKD, and most don’t know it because early disease is often silent . Globally, CKD affects roughly 1 in 10 adults and is a growing cause of illness and early death, closely linked to diabetes and high blood pressure .
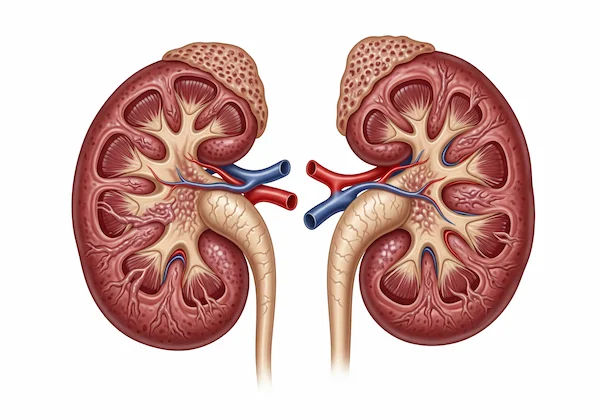
How your kidneys work (in plain language)
Each kidney is a dense network of tiny filters (nephrons) that remove waste, manage fluids, balance electrolytes (like sodium and potassium), and produce hormones that support blood pressure and bone health. When these filters are damaged, waste and fluids can build up, leading to swelling, fatigue, and complications over time.
Chronic vs acute kidney problems
Acute kidney injury (AKI) happens suddenly often due to dehydration, infection, medications, or contrast dyes and can sometimes be reversed. CKD, by contrast, is long term and progresses over years. Preparedness helps you prevent AKI on top of CKD (which can speed decline), and slows CKD progression through targeted daily habits.
Know Your Risk: Who Should Be Screened and When
Screening is simple and inexpensive: a blood test for creatinine (to estimate eGFR) and a urine albumin-to-creatinine ratio (ACR). These “know your numbers” tests catch kidney disease early, when it’s most treatable.
Top risk factors (diabetes, hypertension, family history)
- Diabetes: High blood sugar damages kidney filters over time. Adults with diabetes should have yearly eGFR and ACR checks .
- Hypertension: High blood pressure scars blood vessels in the kidneys. People with hypertension should be screened annually.
- Family history and known genetic conditions (e.g., polycystic kidney disease) increase risk and merit earlier monitoring.
Age, ancestry, and other contributors
Risk rises with age. People of African, South Asian, Indigenous, or Hispanic/Latino ancestry have higher rates of CKD due to a mix of genetic and social determinants of health . Additional risks: heart disease, obesity, autoimmune disease (e.g., lupus), recurrent urinary tract infections, kidney stones, or exposure to nephrotoxic medicines (like frequent NSAIDs).
Screening frequency and where to start
- If you have diabetes or hypertension: test every 6–12 months.
- If you have multiple risks (e.g., age >60 plus high blood pressure): discuss screening with your clinician.
- If you’re lower risk but curious: consider a baseline test and repeat as advised.
Apollo 24|7 offers a convenient home collection for tests like creatinine (eGFR), urine ACR, HbA1c, and lipid profile—handy if you’re managing diabetes and blood pressure together.
Long-tail keywords included: urine albumin-to-creatinine ratio test; home tests for kidney function.
Spot the Signals: Symptoms, Red Flags, and When to Seek Care
Early CKD has few or no symptoms. Consider this a friendly nudge: if you’re at risk, don’t wait for symptoms—get screened.
Early “silent” disease and subtle clues
- Subtle fatigue, reduced exercise tolerance
- Nocturia (urinating more at night), foamy urine (protein in urine)
- Mild ankle swelling, puffiness around the eyes
- These are nonspecific and can be missed. The safest step is testing if you’re at risk.
Red flags that need urgent attention
- Sudden shortness of breath, chest pain, or severe swelling
- Dramatic drop in urine output
- Persistent nausea/vomiting, confusion, severe drowsiness
- Severe flank pain with fever or blood in urine
These may indicate acute kidney injury, severe electrolyte imbalance, or infection. Seek urgent care.
When to speak to a doctor or book teleconsultation?
- If you notice new swelling, foamy urine, or rising blood pressure, speak to a clinician within a week..
- If you’re starting new over-the-counter pain relievers or supplements, ask whether they’re kidney-safe.
Long-tail keywords included: early signs of kidney disease in adults; what to ask your nephrologist.
Diagnosis Demystified: Tests, Stages, and Your Kidney Numbers
CKD is confirmed when reduced kidney function or damage persists for 3+ months. Diagnosis hinges on your numbers—and understanding them helps you stay prepared.
eGFR, creatinine, and ACR explained
- Creatinine: a waste product filtered by kidneys. Higher blood creatinine can indicate reduced kidney function.
- eGFR (estimated glomerular filtration rate): calculated from creatinine, age, sex. Roughly, eGFR ≥90 is normal; lower values suggest reduced kidney filtration.
- Urine ACR: measures albumin leakage. ACR ≥30 mg/g (A2 or A3) signals kidney damage even if eGFR is normal .
CKD stages (G1–G5) and albuminuria (A1–A3)
- G1: eGFR ≥90 with evidence of damage (e.g., ACR ≥30)
- G2: eGFR 60–89 with evidence of damage
- G3a: 45–59; G3b: 30–44
- G4: 15–29
- G5: <15 (kidney failure)
Albuminuria:
- A1: <30 mg/g (normal to mildly increased)
- A2: 30–300 (moderately increased)
- A3: >300 (severely increased)
- Risk is best gauged by combining G and A categories .
How often do you recheck and track your results?
- Mild CKD (G1–G2, A1–A2): typically every 6–12 months
- Moderate (G3a–G3b): every 3–6 months
- Advanced (G4–G5): monthly to every 3 months, often with nephrology
Keep a simple log of eGFR, ACR, blood pressure, and weight. If your condition does not improve or numbers worsen, book a physical visit to a doctor with Apollo 24|7. Long-tail keywords included: CKD stages explained eGFR and ACR; home tests for kidney function.
Citations: staging and risk per KDIGO 2024 , NIDDK .
Everyday Kidney Care: Diet, Activity, and Habits That Help
Prepared daily choices slow CKD and lower heart risks.
Sodium, protein, potassium, and phosphorus—finding your balance
- Sodium: Aim for under 2,000 mg/day to help blood pressure and swelling . Read labels; avoid processed foods.
- Protein: Moderate intake (about 0.8 g/kg/day) in early CKD is often recommended; too much can strain kidneys. In advanced CKD, dietitians may tailor lower-protein plans with careful monitoring .
- Potassium and phosphorus: If levels are high on blood tests or you’re in later stages, you may need to limit high-potassium foods (e.g., certain fruits) and high-phosphorus items (colas, processed cheeses). Don’t restrict blindly—ask for a renal dietitian referral to customize.
- Smart swaps: Use herbs and spices instead of salt; choose fresh over processed; soak and boil certain vegetables to reduce potassium.
Hydration and “sick-day” rules
Stay hydrated, but avoid “over-hydrating.” During vomiting/diarrhea or fever, call your clinician: you may need to pause certain medicines (e.g., ACEi/ARBs, diuretics, metformin) to prevent acute kidney injury—known as “sick-day rules” (local guidance varies; follow your clinician’s advice).
Exercise, sleep, and stopping smoking
- Activity: 150 minutes/week of moderate exercise supports blood pressure, glucose, and mood.
- Sleep: 7–8 hours improves cardiometabolic health.
- Smoking: Quitting reduces CKD progression and heart risk .
If you’re unsure where to start, a kidney-friendly meal plan and gentle walking program can be powerful first steps. Long-tail keywords included: best diet for kidney disease stages 1–3; kidney-friendly meal plan.
Consult a Top Nephrologist for Personalised Advice
Medicines That Protect Kidneys—and Ones to Use Cautiously
Medication choices are central to a prepared plan.
ACE inhibitors/ARBs, SGLT2 inhibitors, finerenone
- ACE inhibitors/ARBs: First-line for hypertension with CKD and albuminuria; reduce proteinuria and slow progression .
- SGLT2 inhibitors (e.g., dapagliflozin, empagliflozin): Recommended for many with CKD (with or without diabetes) to slow kidney decline and reduce cardiovascular events . Finerenone (non-steroidal MRA): For CKD in type 2 diabetes with albuminuria; reduces kidney and heart outcomes when added to ACEi/ARB in selected patients .
- Ask your clinician which medicines fit your stage, albuminuria level, and other conditions.
Diabetes meds and statins for cardiovascular protection
Good glucose control (HbA1c target individualized) and statins for lipid management reduce heart risk—a leading cause of death in CKD . GLP-1 receptor agonists can aid weight and glucose control in type 2 diabetes and may have kidney benefits. Apollo 24|7 offers convenient home collection for tests like HbA1c and lipid profile to support medication adjustments.
NSAIDs and contrast dyes—when to be careful
- NSAIDs (ibuprofen, naproxen): Frequent or high-dose use can reduce kidney blood flow and worsen CKD. Use cautiously and discuss alternatives, especially in dehydration or with ACEi/ARB/diuretics.
- Iodinated contrast: If imaging is necessary, inform the radiology team you have CKD to consider preventive steps or alternatives.
- Long-tail keywords included: medications safe for kidney disease; SGLT2 inhibitors for CKD. Citations: KDIGO 2024, NIDDK, NKF .
Your Kidney Preparedness Plan: Checklists, Disasters, and Self-Tracking
Preparedness is a habit. A simple system can keep you on track.
The Kidney Readiness Checklist (RAG: Red/Amber/Green)
- Green (doing well): Know your latest eGFR and ACR, home blood pressure <130/80 (as advised), salt <2 g/day, daily activity, meds reviewed, non-smoking.
- Amber (needs attention): Rising blood pressure, new swelling/foamy urine, missed labs, frequent NSAID use, inconsistent diabetes control.
- Red (urgent): Severe breathlessness, sharp drop in urine, chest pain, high potassium or creatinine spike on recent labs—seek urgent care.
- Unique insight: Use a color-coded phone note or fridge magnet to remind you which zone you’re in and what actions to take.
Home monitoring: blood pressure, weight, symptom diary
- Check BP 1–2 times/week (daily if advised). Record alongside weight and any swelling, cramps, or sleep issues.
- Share your log during telehealth visits. Many smart cuffs sync to apps.
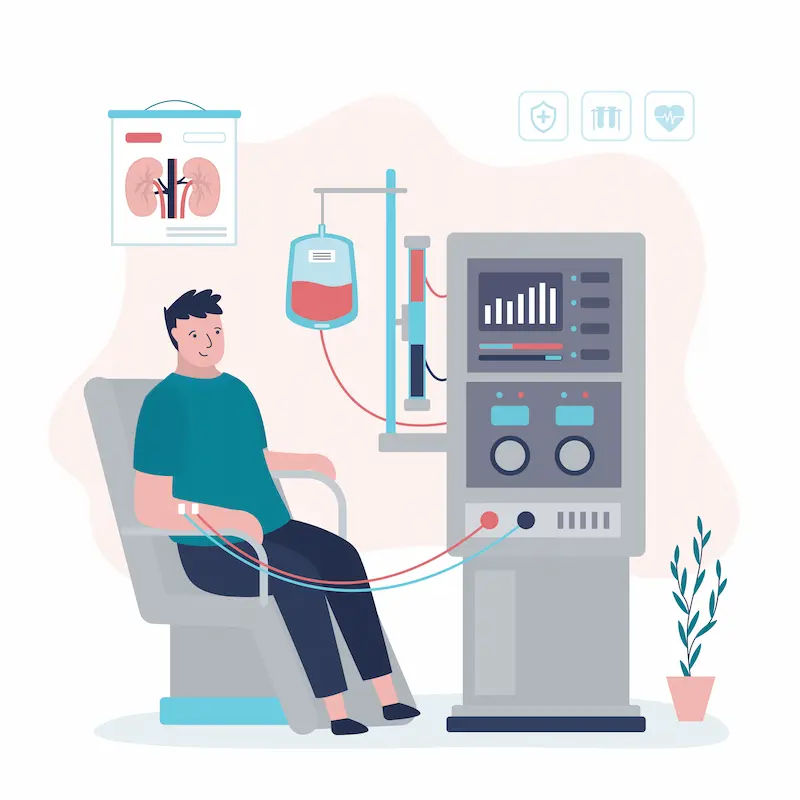
Disaster planning: dialysis continuity, medication list, go-bag
- Keep a two-week supply of essential meds, updated medication/allergy list, and copies of recent labs and insurance info.
- For dialysis: note your center’s disaster plan, alternate sites, and emergency contacts.
Include shelf-stable kidney-friendly foods and bottled water, a portable charger, and a list of your clinicians. This “kidney go-bag” is invaluable during storms, heatwaves, or power cuts. - Long-tail keywords included: emergency plan for dialysis patients; how to prepare for chronic kidney disease.
Looking Ahead: Complications, Advanced Care, and Thriving with CKD
Being prepared means anticipating and preventing complications, and planning for big life moments.
Anemia, bone health, heart risk—what to monitor
- Anemia: Low red blood cells cause fatigue; check hemoglobin and iron indices. Treatments include iron and, sometimes, erythropoiesis-stimulating agents .
- Bone-mineral disorders: Monitor calcium, phosphorus, PTH; use diet and medications as advised to protect bones .
- Heart risk: CKD accelerates atherosclerosis. Control BP, diabetes, and lipids; consider vaccines (flu, pneumococcal, hepatitis B in advanced CKD) per clinician guidance .
If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo 24|7.
Stage-based actions and referrals (dietitian, nephrologist)
- G1–G2, A1–A2: Lifestyle, BP/glucose control, yearly labs.
- G3: Add renal dietitian; evaluate for SGLT2 inhibitors and ACEi/ARB if albuminuria; monitor electrolytes.
- G4: Nephrology referral if not already; education on kidney replacement options; vaccine review.
- G5: Dialysis or transplant planning; optimize symptom relief and quality of life.
- Prepared tip: Ask for written action plans for each stage. Long-tail keywords included: CKD stages explained eGFR and ACR; what to ask your nephrologist.
Life events: travel, pregnancy, mental health support
- Travel: Carry medication list, recent labs, and a medical summary; plan dialysis in advance if needed.
- Pregnancy: Preconception counseling is essential; high-risk obstetric and nephrology co-care improves outcomes.
- Mental health: Anxiety and low mood are common; counseling, peer groups, and activity help. The American Kidney Fund and NKF offer community resources .
Conclusion
Being prepared for kidney disease starts with awareness and ends with action. The most powerful steps are simple: know your risk, test on time, and understand your eGFR and urine ACR. Then build smart routines—low-sodium meals, regular activity, good sleep, and smoke-free living—to protect kidney function and your heart. Medications like ACE inhibitors/ARBs and SGLT2 inhibitors can slow CKD progression, especially if you have albuminuria or diabetes. Equally important is having a plan for bumps in the road: sick-day rules, a go-bag for disasters, and a list of your medicines and latest labs.
If you notice new swelling, foamy urine, or rising blood pressure, don’t wait—early conversations change outcomes. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for timely guidance. And because CKD often travels with diabetes and hypertension, consider Apollo 24|7’s home collection for tests like creatinine (eGFR), urine ACR, HbA1c, and lipid profile to keep your care coordinated.
Preparedness isn’t about fear; it’s about confidence. With clear numbers, daily habits that help, and a practical plan, you can lower risks, prevent complications, and live well with kidney disease—today and in the years ahead.
Consult a Top Nephrologist
Consult a Top Nephrologist
Dr. Nikhil Rathi
Nephrologist
5 Years • MBBS, MD General Medicine, DNB Nephrology
Pune
Apollo Hospitals Pune, Pune

Dr. Vamsee Priya Marina
Nephrologist
13 Years • MBBS, MD (Internal Medicine), MD (Nephrology), Diplomate American Board of Internal Medicine
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda
(50+ Patients)

Dr. Kailash Nath Singh
Nephrologist
27 Years • MBBS, MD , DNB
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr Vinay Kumar A V
Nephrologist
8 Years • MBBS, MD - General Medicine, DM - Nephrology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur

Dr. Bhanu Prasad K
Nephrologist
8 Years • DM (Nephro), MD, MBBS
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda
(25+ Patients)
Consult a Top Nephrologist for Personalised Advice
Dr. Nikhil Rathi
Nephrologist
5 Years • MBBS, MD General Medicine, DNB Nephrology
Pune
Apollo Hospitals Pune, Pune

Dr. Vamsee Priya Marina
Nephrologist
13 Years • MBBS, MD (Internal Medicine), MD (Nephrology), Diplomate American Board of Internal Medicine
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda
(50+ Patients)

Dr. Kailash Nath Singh
Nephrologist
27 Years • MBBS, MD , DNB
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr Vinay Kumar A V
Nephrologist
8 Years • MBBS, MD - General Medicine, DM - Nephrology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur

Dr. Bhanu Prasad K
Nephrologist
8 Years • DM (Nephro), MD, MBBS
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda
(25+ Patients)
More articles from Chronic Kidney Disease Ckd
Frequently Asked Questions
What are the earliest signs of kidney disease?
Early CKD is often silent. Subtle clues include fatigue, foamy urine, and mild ankle swelling. If you have diabetes or high blood pressure, ask for an eGFR and urine albumin-to-creatinine ratio test to detect early kidney disease.
Which diet is best for kidney disease stages 1–3?
Focus on a kidney-friendly meal plan: low sodium (<2 g/day), moderate protein (~0.8 g/kg/day), and plenty of fresh, minimally processed foods. Potassium and phosphorus limits depend on your labs. A renal dietitian can personalize your plan.
What medicines help slow CKD progression?
ACE inhibitors/ARBs lower proteinuria and protect kidneys. SGLT2 inhibitors help many people with CKD (with or without diabetes). In diabetic CKD with albuminuria, finerenone may add further protection. Always review your regimen with your clinician.
Are over-the-counter painkillers safe if I have CKD?
Frequent or high-dose NSAIDs (e.g., ibuprofen, naproxen) can harm kidneys, especially if you’re dehydrated or on ACEi/ARB/diuretics. Discuss safer options with your clinician.
How can I be prepared for emergencies if I’m on dialysis?
Keep a go-bag with a two-week medication supply, updated medication and allergy list, recent labs, insurance details, nonperishable kidney-friendly foods, water, and charger. Confirm your dialysis center’s disaster plan and alternate sites. For non-urgent issues, you can consult a doctor online with Apollo 24|7.


.webp)