Understanding Bypass Surgery
Learn what bypass surgery (CABG) is, why it's performed, the procedure steps, and what to expect during recovery. Get clear, reliable information here.


Introduction
Bypass surgery—often called heart bypass or CABG—is a proven operation that restores blood flow around blocked heart arteries so your heart gets the oxygen it needs. If you or a loved one has been advised to consider bypass surgery, it’s normal to have questions: Do I really need it? How is it performed? What are the risks and how long is recovery? Most importantly, what will life look like after surgery?
This guide walks you through bypass surgery from start to finish. You’ll learn who needs bypass surgery, what happens in the operating room, how doctors reduce risks, and how to recover confidently at home. We’ll explain graft choices (arteries vs veins), compare bypass to stents, share practical pre-op and recovery tips, and outline the lifestyle steps that help your results last. We also include expert-backed facts and patient-friendly checklists so you can prepare, ask the right questions, and make informed decisions with your care team.
Let’s demystify bypass surgery—so you can focus on healing and getting back to the life you love.
What Is Bypass Surgery?
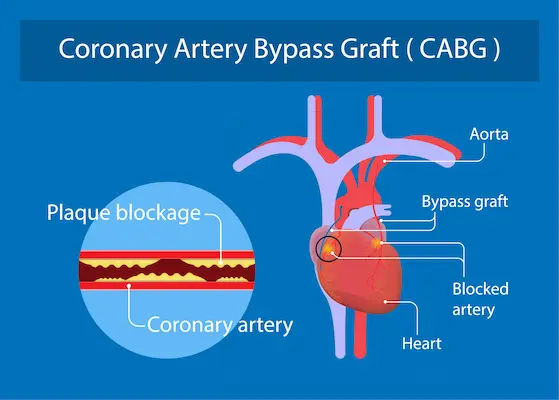
Bypass surgery for the heart—formally called coronary artery bypass grafting (CABG)—reroutes blood around blocked or narrowed coronary arteries using new pathways (“grafts”) taken from elsewhere in your body. Surgeons commonly use an artery from your chest (the left internal mammary artery, or LIMA), an artery from your forearm (radial artery), or a vein from your leg (saphenous vein) to create these detours, restoring blood flow to the heart muscle [1][2]. In everyday language, “heart bypass surgery” provides the heart with a fresh “road” around traffic jams caused by plaque buildup.
You may also hear terms like single, double, triple, or quadruple bypass; these refer to how many arteries are bypassed, not the surgery’s complexity alone. CABG is one of the most studied and time-tested treatments for coronary artery disease, with decades of data on safety and outcomes.
Other procedures called “bypass surgery” exist—such as gastric bypass for weight loss and peripheral bypass for leg arteries—but they address different conditions. This article focuses on heart bypass surgery (CABG), the most common and well-researched form of bypass. If you’ve been told you need bypass surgery after an angiogram or stress test, you’re likely dealing with coronary artery disease significant enough to warrant re-routing blood to protect the heart muscle.
Unique insight: Think of graft choice as the foundation of your new “bridges.” Arterial grafts, especially the LIMA, often last longer than vein grafts; the specific mix your surgeon selects can influence long-term durability. Asking “Which grafts are planned, and why?” is a smart, underused question.
Consult a Top Cardiologist
Who Needs Bypass Surgery?
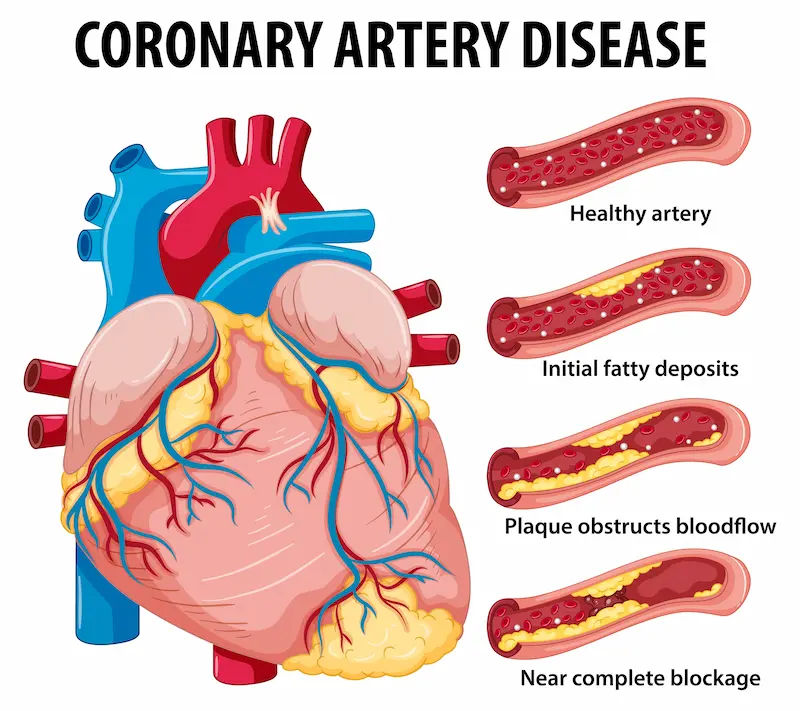
Bypass surgery is recommended when blockages in the coronary arteries are severe enough that medication alone—or
even stenting—may not provide durable relief or survival benefit. Typical scenarios include:
- Persistent angina (chest pain/pressure) despite medications.
- Significant narrowing in the left main coronary artery or multiple major vessels (often called “three-vessel disease”).
- Diabetes with multivessel disease, where CABG has shown better long-term outcomes compared to stents in key
studies. - Reduced heart function due to coronary blockages, where revascularization can improve symptoms and sometimes
survival.
How doctors decide:
Your cardiology team looks at symptoms, stress testing, imaging (CT angiography), and especially coronary
angiography to map the exact blockages. They weigh anatomy complexity (e.g., SYNTAX score), your overall health
(diabetes, kidney function), and your preferences. A “Heart Team”—cardiologist and cardiac surgeon—often reviews
your case together.
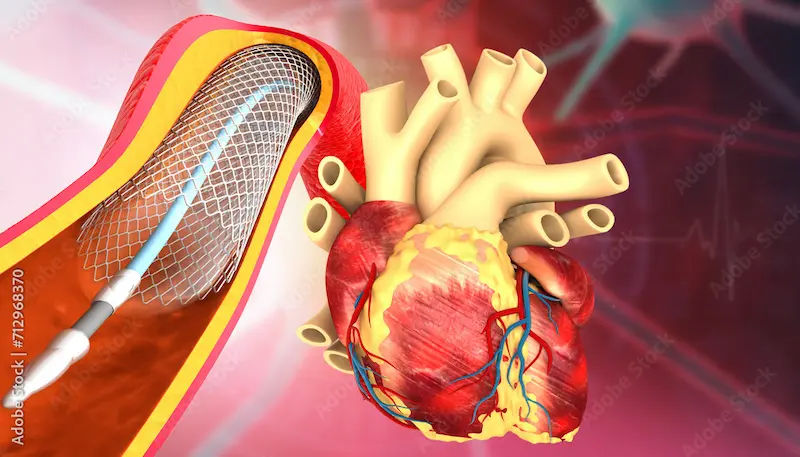
CABG vs stents vs medicines:
Stents (PCI) are excellent for focal blockages and quick relief, but bypass surgery can be better for complex, diffuse
disease, especially in diabetics and those with left main or multivessel disease. Medications remain essential either way
for long-term protection.
Example: A 62-year-old with diabetes and three-vessel disease who still has angina on optimal medication—many Heart Teams would favor CABG here based on trials showing lower repeat procedures and improved outcomes vs stents in similar patients.
If you’re unsure whether bypass surgery is right for you—or if chest discomfort persists beyond a couple of weeks—consult a doctor online with Apollo24|7 for further evaluation and next steps.
How Bypass Surgery Works?
Grafts: the “detours”
- LIMA (left internal mammary artery): The gold-standard graft for the left anterior descending (LAD) artery; patency
(staying open) rates frequently exceed 90% at 10 years. - Radial artery (forearm): An excellent arterial option when suitable; typically better long-term patency than vein grafts.
- Saphenous vein (leg): Common and versatile but more prone to narrowing over time; roughly half may narrow within
10 years, though results vary.
Technique choices
- On-pump vs off-pump: On-pump uses a heart-lung machine with the heart temporarily stopped; off-pump (beating-heart)
avoids the machine. Outcomes are similar in most groups; your surgeon chooses based on experience, your anatomy, and overall risk . - Minimally invasive and robotic options: In selected patients (often single-vessel LAD disease), minimally invasive direct
CABG (MIDCAB) or robotic-assisted approaches use smaller incisions and may speed recovery, though not everyone is
a candidate.
How many bypasses?
“Double,” “triple,” and “quadruple” refer to the number of arteries bypassed. More grafts do not automatically mean a
riskier surgery; the decision depends on the number and location of significant blockages.
Unique insight: Surgeons don’t just pick “the best” graft in general—they match grafts to the target artery’s size,
location, and blood-flow demand. For example, using LIMA to the LAD has proven survival benefits, while a radial
artery might be chosen for a high-quality target with good runoff. Asking about the “graft map” for your case can help
you understand your personalized plan.
Preparing for Bypass Surgery
Pre-op testing and optimization
- Tests often include ECG, echocardiogram, blood work (including HbA1c and kidney function), chest X-ray, and
sometimes lung tests or carotid ultrasound [1][5]. Dental checkups can reduce the risk of infection seeds. - Risk factor tune-up: Stop smoking as soon as possible; control blood pressure, blood sugar, and cholesterol aggressively;
practice breathing exercises (incentive spirometer) to strengthen lungs.
Medications: what to stop or continue
- Aspirin is often continued; other antiplatelets like clopidogrel/ticagrelor are typically stopped about 5 days pre-op (your
team will guide this). - Blood thinners (e.g., DOACs/warfarin) are held with a plan to bridge if needed.
- High-intensity statins are commonly continued and may reduce complications.
- Nasal mupirocin and skin prep may be used to reduce infection risk.
Smart home prep and caregiver planning
- Prepare a recovery space with a firm chair, side table, and items within easy reach; remove trip hazards.
- Line up help for the first 2 weeks (meals, bathing assistance, transport).
- Cook and freeze heart-healthy meals in advance; stock fiber-rich foods to prevent constipation.
Convenience tip: If your clinician orders pre-op labs like HbA1c or lipid profile, Apollo24|7 offers a convenient home
collection so you don’t have to travel.
Unique insight: “Prehabilitation”—gentle walking, breathing exercises, and nutrition optimization for a few weeks
before surgery—improves strength and confidence and can reduce complications. Ask your team for a prehab plan tailored to your fitness and timing.
The Operation: Step by Step
What happens on the day
- Pre-op: You’ll meet anesthesia and surgical teams. An IV, monitoring lines, and (in some cases) a catheter are placed.
- Anesthesia: You’ll be fully asleep and pain-free.
- Surgical steps: The surgeon harvests grafts (often with minimally invasive tools), opens the chest via a midline incision
(sternotomy) or smaller incisions for select cases, and performs the bypasses. On-pump CABG involves stopping the
heart temporarily with cardioplegia while the heart-lung machine oxygenates your blood; off-pump CABG is done on the beating heart. - Completion: After grafting, the team restarts the heart (if on-pump), places chest tubes to drain fluid, and closes the
incisions.
How long does it take?
Most operations take 3–6 hours depending on the number of grafts and your anatomy. Many patients spend the first
night in the ICU and move to a step-down unit the next day.
What “success” means
A successful operation restores blood flow to areas at risk, relieves angina, and sets you up for long-term protection—
especially when paired with medications and lifestyle changes.
Safety and checklists
Operating rooms use rigorous protocols (e.g., WHO surgical safety checklists) and team briefings to minimize errors
and infections. Surgeons and anesthesiologists also plan for blood conservation and strict temperature and glucose
control—all of which improve outcomes.
Unique insight: Ask your team how they prevent sternal wound infection (skin prep, glucose control, graft choices in
diabetics) and how they minimize stroke risk (aortic handling techniques). These are nuanced topics that can
meaningfully affect outcomes.
Risks and Complications
Common and usually temporary
- Pain and fatigue: Expect soreness around the chest and graft sites; pain is controllable, and movement actually speeds
healing. - Swelling at the leg/arm graft site, constipation, appetite changes, and sleep disruption are common and improve with
time. - Post-op atrial fibrillation (irregular rhythm) occurs in about 20–40% of patients but is usually temporary and treatable.
Serious but less common
- Bleeding requiring transfusion or rarely re-operation.
- Infection: Superficial or, less commonly, deep sternal wound infection (risk higher with diabetes/obesity) [5].
- Stroke: Generally 1–2% risk in average-risk patients; risk varies with age, atherosclerosis burden, and operative factors [2][5].
- Kidney injury: Usually mild and temporary but can be serious in high-risk patients.
Operative mortality for CABG in contemporary practice is often in the 1–3% range, depending on individual risk factors and complexity. Teams use risk calculators (STS, EuroSCORE) to personalize risk estimates.
How teams reduce risk—and what you can do
- Evidence-based antibiotic timing, tight glucose control, meticulous aortic handling, and choosing arterial grafts when
appropriate all help. - Your role: Stop smoking, take medications as prescribed (especially statins and beta-blockers if directed), use your
incentive spirometer, walk early, and follow wound-care instructions closely.
Unique insight: Early recognition is powerful. Report fever, drainage, worsening leg swelling, shortness of breath, or chest pain promptly. Wearables that track heart rate and rhythm can sometimes help flag issues like atrial fibrillation—ask your team if remote monitoring is available.
Recovery and Rehabilitation
Hospital milestones
- Day 0–1: ICU care with close monitoring. Breathing tube removed once you’re awake and stable. Pain controlled with
medication. Start incentive spirometry and gentle leg movements. - Day 2–4: Move to the step-down unit. Begin walking with assistance; eating and bowel function normalize. Education
on wound care and medications begins. - Discharge: Many patients go home within 4–7 days if stable.
At-home care: first 6–8 weeks
- Sternal care: Avoid heavy lifting (>2–5 kg per arm) and activities that strain the chest (pushing/pulling) until cleared—
your surgeon will provide a timeline. - Wounds: Keep clean and dry; watch for redness, separation, discharge, or fever.
- Activity: Start with short, frequent walks and increase gradually. Gentle daily routines are encouraged; driving typically
resumes around 4–6 weeks if no sternum pain and after medical clearance. - Emotions and sleep: Mood changes are common. Prioritize sleep hygiene and speak up about anxiety or low mood—
brief counseling or medication can help.
Cardiac rehabilitation
A supervised cardiac rehab program improves fitness, reduces readmissions, and is associated with lower mortality after
bypass surgery. It includes monitored exercise, education, and coaching on diet, stress, and medications. If access is difficult, ask about home-based or hybrid programs.
When to seek help
Call your care team or emergency services for chest pain at rest, shortness of breath, fainting, fever or chills, wound
redness/drainage, or new palpitations. If symptoms persist beyond two weeks or you’re unsure about a symptom,
consult a doctor online with Apollo24|7 for further evaluation. For follow-up labs like lipid profile or HbA1c, Apollo24|7 offers home collection so you can track progress without leaving home.
Unique insight: Think “pace, not race.” Small, consistent gains—like adding 2–5 minutes to your daily walk each week—beat overexertion. Pair a new habit with an existing one (e.g., walk after morning tea) to make it stick.
Living Well After Bypass
Medications for protection
- Antiplatelet therapy: Aspirin long-term; additional agents sometimes used based on your case.
- Statins: High-intensity statins to target LDL cholesterol—often <70 mg/dL (or <55 mg/dL for very-high risk); your
clinician will set your target. - Beta-blockers, ACE inhibitors/ARBs, and others as indicated (e.g., for blood pressure, heart function).
Diet, exercise, and targets
- Diet: Emphasize vegetables, fruits, whole grains, legumes, nuts, olive oil, and fish (Mediterranean-style). Limit refined
sugar, salt, and processed meats. - Exercise: Aim for 150 minutes/week of moderate activity plus muscle strengthening twice weekly, adjusted to your
recovery stage. - Targets: BP generally <130/80; LDL to guideline targets; HbA1c individualized (often <7% for many with diabetes).
Work, sex, and travel
- Work: Many return to desk jobs in 6–8 weeks; physically demanding jobs may take longer.
- Sex: If you can climb two flights of stairs without symptoms, sexual activity is often safe—ask your doctor for
personalized advice. - Travel: After initial follow-up and if stable, short trips are reasonable. Carry a medication list and recent medical
summary.
Long-term outcomes and graft longevity
- LIMA-to-LAD grafts often remain open for decades; saphenous vein grafts have lower long-term patency.
- CABG may reduce the need for repeat procedures compared with stents in complex multivessel disease, especially in
patients with diabetes. - Healthy living and consistent medications greatly influence how long your benefits last.
Unique insight: Make your future appointments “automatic.” Book your 6–12 week surgical and cardiology follow-ups
before leaving the hospital, and set recurring reminders for yearly check-ins and lab tests.
Conclusion
Bypass surgery can sound daunting, but understanding the process makes it far more manageable. At its core, CABG
restores vital blood flow to your heart, relieving symptoms and helping prevent future cardiac events. For many people—especially those with complex blockages or diabetes—bypass surgery offers more durable benefits than stents alone. The operation is only part of the journey, though. Your graft choices, risk-factor control, and day-to-day habits strongly influence how well you do in the years ahead.
Approach recovery as a series of small, steady steps: breathe deeply, walk a little more each day, care for your wounds, and stick to your medication plan. Enroll in cardiac rehab and ask questions—about your grafts, targets for cholesterol and blood pressure, and when you can return to favorite activities. If something doesn’t feel right, contact your care team promptly. If you need quick advice or can’t get to a clinic, consult a doctor online with Apollo24|7. Remember, you can use home collection for follow-up labs, such as lipid profiles or HbA1c.
With the right preparation, a supportive care team, and healthy routines, most people reclaim active, satisfying lives after bypass surgery. Use this guide to spark informed conversations and to chart your path to recovery—one confident step at a time.
Consult a Top Cardiologist
Consult a Top Cardiologist

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Tripti Deb
Cardiologist
40 Years • MBBS, MD, DM, FACC, FESC
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
Dr Moytree Baruah
Cardiologist
10 Years • MBBS, PGDCC
Guwahati
Apollo Clinic Guwahati, Assam, Guwahati

Dr. Zulkarnain
General Physician
2 Years • MBBS, PGDM, FFM
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Haider Shaik.
Cardiologist
5 Years • MBBS, MD (Pulmonology) DrNB (Cardiology)
Guntur
Kalam chest and multi-speciality clinic, Guntur
Consult a Top Cardiologist

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Tripti Deb
Cardiologist
40 Years • MBBS, MD, DM, FACC, FESC
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
Dr Moytree Baruah
Cardiologist
10 Years • MBBS, PGDCC
Guwahati
Apollo Clinic Guwahati, Assam, Guwahati

Dr. Zulkarnain
General Physician
2 Years • MBBS, PGDM, FFM
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Haider Shaik.
Cardiologist
5 Years • MBBS, MD (Pulmonology) DrNB (Cardiology)
Guntur
Kalam chest and multi-speciality clinic, Guntur
More articles from Coronary artery disease
Frequently Asked Questions
1) Is bypass surgery better than stents?
It depends on your anatomy and health. For complex multivessel disease, left main disease, or diabetes, bypass surgery often provides better long-term outcomes and fewer repeat procedures than stents. Your Heart Team will compare PCI vs CABG for your case.
2) How long is the recovery from bypass surgery?
Hospital stay is typically 4–7 days. Most people need 6–8 weeks for the breastbone to heal and to feel steadily stronger. Cardiac rehab can speed and smooth this process. Ask your doctor about a personalized timeline.
3) What are the main risks of bypass surgery?
Common issues include pain, fatigue, temporary irregular heartbeat (atrial fibrillation), and swelling at graft sites. Less common but serious complications include bleeding, infection, stroke, and kidney problems. Overall risk depends on your age, health, and anatomy.
4) How long do bypass grafts last?
Arterial grafts like the LIMA often stay open for many years—often over 90% patency at 10 years for LIMA-to-LAD. Vein grafts have lower long-term patency. Medications and lifestyle changes help all grafts last longer.
5) What lifestyle changes should I make after bypass surgery?
Take prescribed medications (aspirin, statin, and others), follow a Mediterranean-style diet, exercise regularly (often 150 minutes/week when cleared), and keep targets for LDL cholesterol, blood pressure, and blood sugar. Enroll in cardiac rehab for coaching and support.
 Purpose, Procedure, and Results.webp)