Guide to Fractional Flow Reserve (FFR) Purpose, Procedure, and Results
Learn about fractional flow reserve (FFR), a key test in cardiology that measures blood flow across coronary blockages, guiding decisions on stents or medication for heart health.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026
%20Purpose,%20Procedure,%20and%20Results.webp?tr=q-80,f-webp,w-350,dpr-2,c-at_max 700w)
Introduction: Beyond the Angiogram – The Need for a Functional Measurement
When you have symptoms like chest pain or shortness of breath, your cardiologist might recommend an angiogram—a special X-ray that takes pictures of your heart's arteries. This test can reveal if there are narrowings or blockages caused by plaque. But here's the catch: an angiogram is like a road map; it shows where the narrow spots are, but it doesn't tell you if those narrowings are actually causing a significant traffic jam for blood flow. This is where fractional flow reserve (FFR) comes in. Think of FFR as the "rush hour test" for your coronary arteries. It's a sophisticated wire-based technique performed during an angiogram that precisely measures blood pressure and flow across a blockage. This guide will demystify FFR, explaining why it's a game-changer in cardiology, what the procedure involves, and how its results empower you and your doctor to make the most informed decision about your heart health, whether that means placing a stent or managing with medication.
What is Fractional Flow Reserve (FFR)? A Simple Explanation
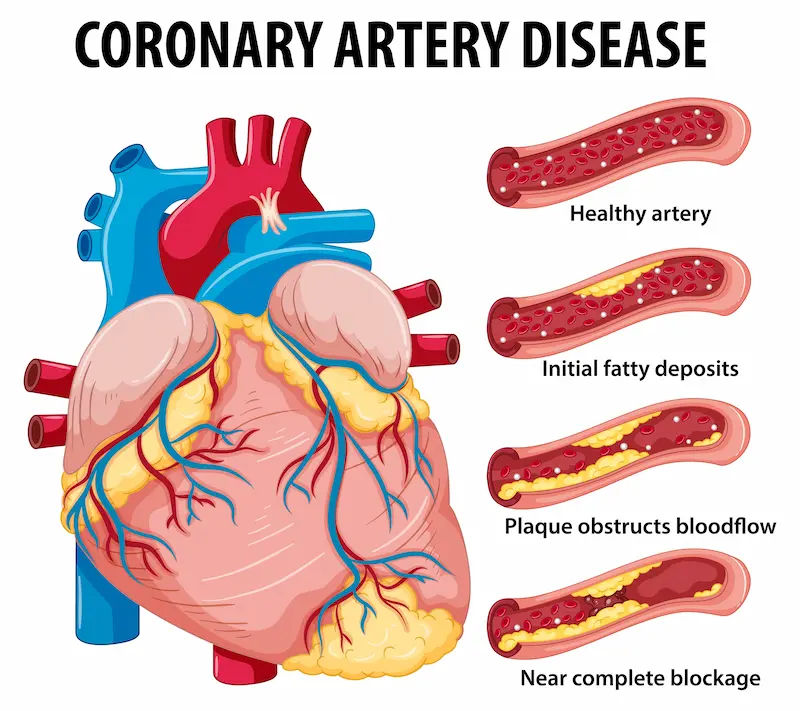
Fractional flow reserve (FFR) is a minimally invasive procedure used to measure the pressure and blood flow around a blockage in a coronary artery. It provides a specific number that helps cardiologists determine if a particular narrowing is severe enough to deprive the heart muscle of adequate oxygen, a condition known as ischaemia.
The Plumbing vs. Physiology Analogy
Imagine your heart's arteries are pipes. An angiogram is a camera that shows a narrowing in the pipe. But is that narrowing just a cosmetic issue, or is it severely restricting water flow to a critical part of the house? FFR answers this question. It measures the physiology—the actual flow—rather than just the anatomy. By comparing the blood pressure before and after the blockage, FFR calculates the fraction of normal flow that's getting through.
The Key Number: What Does an FFR Value Mean?
The result is a simple ratio, typically between 0.50 and 1.00.
An FFR value of 1.00 means there is no pressure drop across the blockage; it's not significant.
The universally accepted cut-off point is 0.80. An FFR value above 0.80 suggests the blockage is not flow-limiting, and medication is often the best course of action. A value at or below 0.80 indicates the blockage is significantly reducing blood flow and that placing a stent would likely benefit the patient by relieving ischaemia.
Consult a Cardiologist for the best advice
Why is an FFR Test Performed? The Critical Decision Point
The primary purpose of an FFR test is to remove the guesswork from treating coronary artery disease. It answers the critical question: "Does this specific blockage need to be stented?"
When Angiography Isn't Enough: Moderate Blockages
On an angiogram, blockages that appear to be between 40% and 70% narrowed are often in a "gray zone." It's difficult to tell from pictures alone if they are severe enough to cause symptoms or future risk. FFR provides objective data, preventing unnecessary stent placements for blockages that aren't truly harmful and ensuring that significant ones are not missed.
Guiding Treatment: Stent or Medication?
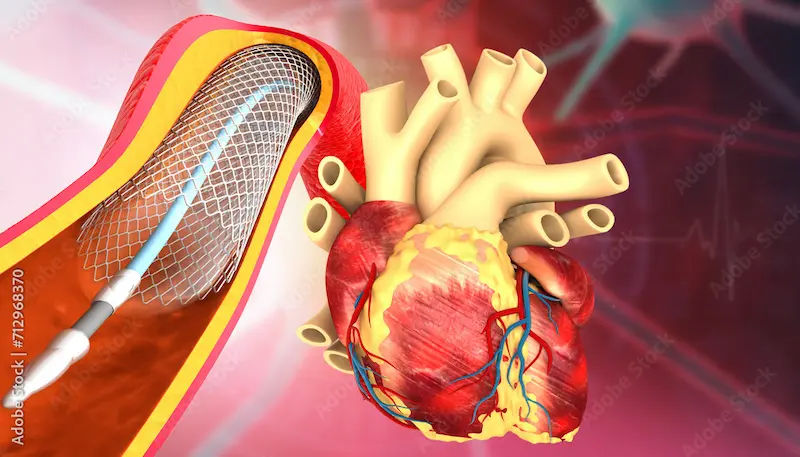
This is the most crucial application. Studies like the landmark FAME trial have proven that using FFR-guided PCI (percutaneous coronary intervention, or stenting) leads to better patient outcomes than using angiography alone. It helps avoid implanting stents where they aren't needed, which is beneficial because every stent carries a small, long-term risk of clotting. By stenting only the arteries that are proven to be ischaemic, patients often have better symptom relief and a lower risk of future heart attacks.
The FFR Procedure: What to Expect Step-by-Step
An FFR measurement is performed during a standard coronary angiogram. You will already be in the catheterisation lab, so the process is an extension of that procedure.
Preparation: Before Your Cardiac Catheterisation
Your preparation is the same as for a standard angiogram. This typically involves fasting for several hours beforehand. You will receive sedation to help you relax, but you will be awake. Your doctor will discuss all risks and benefits with you before the procedure.
During the Procedure: The Pressure Wire and Hyperaemia
The procedure is carried out in a series of steps:
1. The Angiogram: The doctor first performs the angiogram to visualise the blockages.
2. Inserting the Wire: A very thin, specialised pressure wire is passed through the same catheter and guided into the coronary artery, moving it across the blockage.
3. Measuring Pressure: The wire measures the blood pressure on the far side of the blockage.
4. Inducing Hyperaemia: To simulate the stress of exercise, a medication (usually adenosine) is administered through an IV. This drug temporarily maximally dilates the heart's arteries, increasing blood flow. If the blockage is significant, the pressure will drop dramatically across it during this peak flow.
5. Calculation: The wire's sensor and a computer calculate the FFR ratio in real-time. The doctor sees the result on a screen immediately.
After the Procedure: Recovery and Next Steps
The pressure wire is removed. Your recovery is identical to a standard angiogram—a few hours of lying flat to ensure the insertion site (usually in the wrist or groin) heals properly. Based on the FFR result, your doctor will discuss the next steps with you right away.
Interpreting Your FFR Results: What the Numbers Tell Your Doctor
The FFR value provides a clear, evidence-based roadmap for treatment.
FFR > 0.80: Optimal Medical Therapy
If the FFR value is above 0.80, it indicates the blockage is not causing significant ischaemia. In this case, the best approach is usually optimal medical therapy. This includes medications like statins to lower cholesterol, aspirin to prevent clots, and drugs to control blood pressure and heart rate, along with lifestyle changes. If you are prescribed new medications, it's important to follow up with your cardiologist. You can easily manage your prescriptions and schedule follow-up consultations online with Apollo24|7.
FFR ≤ 0.80: Considering a Stent
An FFR value of 0.80 or lower is a strong indicator that the blockage is hemodynamically significant. Placing a stent to prop the artery open is likely to improve blood flow, relieve symptoms like chest pain, and potentially reduce the long-term risk of heart attack related to that specific artery.
The Gray Zone and Other Factors
While 0.80 is the standard threshold, decisions are not made by numbers alone. Your doctor will consider your specific symptoms, the location of the blockage, and other clinical factors to make the final, personalised treatment recommendation.
Benefits and Risks of Fractional Flow Reserve
Evidence-Based Benefits: The FAME Study and Beyond
The benefits of FFR are well-documented. The FAME study showed that compared to angiography-guided stenting, FFR-guided PCI resulted in:
1. Lower rates of death and heart attack at one and two years.
2. Fewer stents used per patient.
3. Lower overall procedure costs and improved patient outcomes.
Potential Risks and Safety Profile
Since FFR is performed during an angiogram, it shares the same low risks, such as bleeding or infection at the insertion site. The administration of adenosine causes a brief, harmless feeling of flushing or chest warmth, and it may slow the heart rate or cause shortness of breath for a few seconds. These effects stop as soon as the medication is discontinued. Serious complications are very rare.
FFR vs. Other Tests: How It Compares to iFR and IVUS
FFR is the gold standard, but other technologies exist:
• iFR (Instantaneous Wave-Free Ratio): Similar to FFR, iFR also uses a pressure wire but does not require adenosine. It measures pressure during a specific, quiet phase of the heartbeat. Studies show iFR is non-inferior to FFR in guiding stent decisions. The choice between FFR vs iFR often depends on physician preference and patient factors (e.g., if adenosine cannot be used).
• IVUS (Intravascular Ultrasound): This uses sound waves to create a detailed, 3D image of the artery wall and plaque from the inside. It provides anatomical detail, while FFR provides functional data. They are sometimes used together for complex cases.
Conclusion
Fractional flow reserve (FFR) represents a significant advancement in personalised cardiology. It moves beyond simply what a blockage looks like to understand what it actually does. By providing a precise, numerical value for blood flow, FFR empowers you and your doctor to make a more confident, evidence-based decision about whether a stent is necessary. This approach helps ensure that patients receive the right treatment at the right time, avoiding unnecessary procedures while effectively treating dangerous blockages. If you are undergoing an angiogram for suspected coronary artery disease, discussing the potential use of FFR with your cardiologist is a crucial step in your care journey.
Consult a Cardiologist for the best advice
Consult a Cardiologist for the best advice

Dr. Srinivasan K N
Cardiologist
11 Years • MD, DNB (Cardio)
Chennai
Apollo Hospitals Greams Road, Chennai
(200+ Patients)
Dr. Raman Puri
Cardiologist
29 Years • MD, DM
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Vijayakumar Subban
Cardiologist
15 Years • MD, DM (Cardiology), FNB (Intreventional Cardiology), Fellowship in Interventional Cardiology (The Prince Charles Hospital, Brisbane, Australia), Fellowship in Intravascular Imaging and Physiology (Asan Medical Center, Seoul, Korea), Cardiac CT (SCCT- Level II), Cardiac MRI (SCMR- Level I)
Chennai
Apollo Hospitals Greams Road, Chennai
(150+ Patients)

Dr. Zulkarnain
General Physician
2 Years • MBBS, PGDM, FFM
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. A Ravindra
Cardiologist
16 Years • MBBS, M.D-GENERAL MEDICINE, D.M-CARDIOLOGY
Hyderabad
Apollo Clinic Chanda Nagar, Hyderabad
Consult a Cardiologist for the best advice

Dr. Srinivasan K N
Cardiologist
11 Years • MD, DNB (Cardio)
Chennai
Apollo Hospitals Greams Road, Chennai
(200+ Patients)
Dr. Raman Puri
Cardiologist
29 Years • MD, DM
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Vijayakumar Subban
Cardiologist
15 Years • MD, DM (Cardiology), FNB (Intreventional Cardiology), Fellowship in Interventional Cardiology (The Prince Charles Hospital, Brisbane, Australia), Fellowship in Intravascular Imaging and Physiology (Asan Medical Center, Seoul, Korea), Cardiac CT (SCCT- Level II), Cardiac MRI (SCMR- Level I)
Chennai
Apollo Hospitals Greams Road, Chennai
(150+ Patients)

Dr. Zulkarnain
General Physician
2 Years • MBBS, PGDM, FFM
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. A Ravindra
Cardiologist
16 Years • MBBS, M.D-GENERAL MEDICINE, D.M-CARDIOLOGY
Hyderabad
Apollo Clinic Chanda Nagar, Hyderabad
More articles from Coronary artery disease
Frequently Asked Questions
1. Is the FFR test painful?
No, the FFR test itself is not painful. It is performed under local anaesthesia and sedation. You might feel a warm, flushing sensation when the adenosine is administered, but this lasts only for a short time.
2. What is the cost of a fractional flow reserve test?
The cost of a fractional flow reserve test can vary depending on the hospital, geographic location, and insurance coverage. Since it's an integral part of a therapeutic procedure, it's best to check with your hospital and insurance provider for specific cost details.
3. How long does the FFR procedure take?
The actual FFR measurement typically adds only about 5-10 minutes to a standard angiogram procedure.
4. Can FFR be used for all coronary blockages?
FFR is most valuable for evaluating blockages of intermediate severity (40-70% narrowing). It is generally not needed for very mild blockages or for severely blocked arteries where the need for a stent is already clear from the angiogram.
5. What are the risks of the adenosine medication?
Adenosine is very safe when used in a controlled setting. Common, transient side effects include flushing, chest warmth, and shortness of breath. It is avoided in patients with severe asthma or COPD, and your doctor will review your history beforehand.