Platelet Count in Dengue Fever: A Complete Guide to Low Levels & Recovery
Know about the platelet count and dengue fever connection, what dengue fever is, its impact, why platelet counts and monitoring are essential and more.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026

Introduction
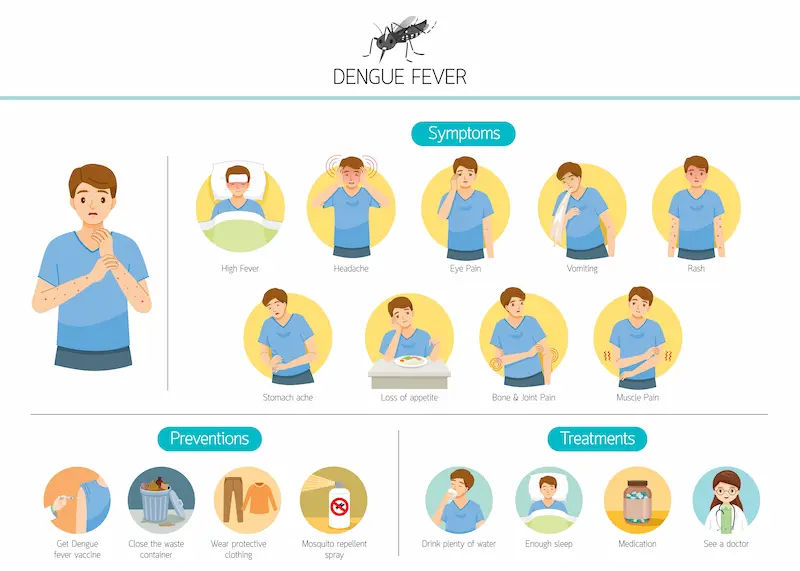
Dengue fever is a mosquito-borne illness that affects millions worldwide each year. While often causing high fever and severe body aches, one of its most talked-about and worrying aspects is its impact on platelet count. This drastic drop in platelets, a condition known as thrombocytopenia, is a hallmark of dengue.
This comprehensive guide demystifies the relationship between dengue fever and platelet count, separating fact from fiction. We'll walk you through why it happens, how it's monitored, the real thresholds for medical intervention, and evidence-based ways to support your body's recovery.
Understanding Dengue Fever and Its Impact
The Dengue Virus and Its Phases
The illness typically unfolds in three phases: febrile, critical, and recovery. The initial febrile phase involves high fever, headache, and joint pain. This is followed by the critical phase, usually around the time the fever subsides, where plasma leakage and a significant drop in platelet count can occur, increasing the risk of complications. Finally, the recovery phase sees gradual reabsorption of fluids and a steady rise in platelets.
Consult a General Practitioner for Personalised Advice
What Are Platelets and Why Are They Crucial?
Platelets, or thrombocytes, are tiny, colourless cell fragments in our blood that are essential for clotting. When you get a cut, platelets rush to the site, clump together, and form a plug to stop the bleeding.
A normal platelet count ranges from 150,000 to 450,000 platelets per microliter of blood. When this number falls too low, the body's ability to clot is impaired, leading to an increased risk of bleeding, from minor bruises to serious internal haemorrhage.
The Critical Link Between Dengue and Platelet Count
It includes
How the Dengue Virus Causes Thrombocytopenia
The drop in platelet count in dengue fever isn't due to a single cause but a perfect storm of several factors. Firstly, the dengue virus can directly infect and damage the cells in the bone marrow (megakaryocytes) that are responsible for producing platelets. This is known as bone marrow suppression, effectively shutting down the factory where platelets are made.
Bone Marrow Suppression: A Key Factor
Studies have shown that the dengue virus suppresses bone marrow function. This means that even if the body needs to produce more platelets to counter the loss, it temporarily cannot. This suppression is often most significant during the critical phase of the illness, explaining why platelet levels continue to fall even after the initial viral infection.
The Role of Antibodies and Immune Response
The immune system's response to the virus also plays a role. Antibodies created to fight the dengue virus can sometimes mistakenly recognise platelets as foreign invaders and destroy them. Furthermore, the widespread inflammation caused by the infection can lead to increased consumption of platelets, further depleting their numbers.
Monitoring Your Platelet Count: What the Numbers Mean
The platelet count interpretation includes:
Normal Platelet Count Range
A healthy individual typically has a platelet count between 150,000 and 450,000/µL. During dengue fever, it is common to see this number begin to fall around day 3-4 of the illness.
Interpreting a Declining Platelet Count in Dengue
Doctors monitor the trend, not just a single number. A steady decline is expected. Counts between 100,000-150,000/µL indicate mild thrombocytopenia. Between 20,000-100,000/µL is considered moderate, and this is the range where most dengue patients will find themselves. Counts below 20,000/µL are severe and require very close monitoring.
When is the Lowest Platelet Count Reached?
The platelet count usually reaches its nadir (lowest point) during the critical phase, around days 4-7 of the illness. After this point, as the patient enters the recovery phase, the bone marrow function recovers, and the count begins to steadily rise again on its own.
Symptoms and Risks of a Low Platelet Count (Thrombocytopenia)
The symptoms and risks of low platelet count include:
Warning Signs to Watch For
While a low count itself may not cause symptoms, the resulting bleeding tendency can. Be vigilant for:
Petechiae: Tiny red or purple spots on the skin, like a rash that doesn't fade when pressed.
Purpura: Larger purple bruise-like areas.
Bleeding: From the nose (epistaxis) or gums.
Heavier-than-normal menstrual bleeding.
Blood in urine or stool.
Understanding the Risk of Bleeding and Haemorrhage
The primary risk of severe thrombocytopenia is spontaneous bleeding or haemorrhage. However, it's crucial to understand that a low platelet count is not the only factor determining bleeding risk. The integrity of the blood vessels also plays a key role. This is why doctors look for these clinical signs of bleeding rather than transfusing platelets based on a number alone.
Medical Management and Platelet Transfusions
When is a Platelet Transfusion Necessary?
This is the most common question. According to the World Health Organisation (WHO) and other health bodies, platelet transfusion is not automatically required for a low count. It is primarily recommended in two scenarios:
1. When the platelet count is below 20,000/µL AND there is active bleeding.
2. When the count is below 10,000/µL as a prophylactic measure to prevent spontaneous bleeding is used even if no bleeding is present.
Unnecessary transfusions can lead to adverse reactions and fluid overload.
The Process of a Platelet Transfusion
A transfusion involves intravenously administering donated platelets from a healthy donor. This is a medical procedure done in a hospital setting. The effect is temporary, as the transfused platelets have a short lifespan of a few days, but it can provide a crucial bridge until the patient's own bone marrow begins to recover.
Other Medical Treatments and Supportive Care
The mainstay of dengue fever treatment is supportive care: staying hydrated with oral rehydration solutions (ORS) or intravenous fluids to maintain blood volume and pressure. This is often more critical than focusing solely on the platelet count. Close monitoring of vital signs and hematocrit levels is standard practice.
Diet and Natural Ways to Support Platelet Production
The Role of Hydration
Adequate hydration is paramount. It helps maintain blood volume, supports overall organ function, and can aid in a smoother recovery. Water, ORS, coconut water, and clear soups are excellent choices.
Key Nutrients and Vitamins for Platelet Health
Once the recovery phase begins and the patient can eat, certain nutrients can support the bone marrow:
Vitamin B12 and Folate: Crucial for the production of all blood cells, including platelets. Found in leafy greens, eggs, and dairy.
Iron: Essential for healthy blood cell production. Found in lean meats, beans, and lentils.
Vitamin C: Helps with iron absorption and is a powerful antioxidant. Found in citrus fruits, kiwi, and bell peppers.
Vitamin K: Plays a key role in clotting. Found in green leafy vegetables like spinach and kale.
Food Myths to Avoid
Include: Papaya (and its leaves), pomegranate, pumpkin, lean proteins, and whole grains.
Myths to Avoid: The evidence for papaya leaf juice is mixed. Some small studies suggest it may help increase platelet count, but larger, robust clinical trials are needed. It is not a substitute for medical care. Kiwi fruit and beetroot are often recommended for their nutrient profile, but are not magic bullets. Always prioritise a balanced diet and follow your doctor's advice.
The Recovery Phase: Watching Platelets Rise
What to Expect During Recovery
As the critical phase passes, the body begins to heal. The bone marrow resumes normal function, and the platelet count will start to climb. This rise can be rapid, often increasing by 30,000-50,000/µL per day in the initial recovery stage.
How Long Until Platelets Return to Normal?
It typically takes 1-2 weeks for the platelet count to normalise after it has bottomed out. Doctors will often continue to monitor it until it is consistently within the normal range to ensure full recovery.
Conclusion
Navigating a dengue fever diagnosis can be frightening, especially with the constant worry about a dropping platelet count. However, knowing the science behind it, you can be a proactive participant in care. Remember, thrombocytopenia is a common and expected part of dengue.
The key is not to fixate on a single number but to focus on comprehensive medical management, primarily staying hydrated and watching for clinical signs of bleeding. Support your body's innate recovery process with rest and good nutrition.
Consult a General Practitioner for Personalised Advice
Consult a General Practitioner for Personalised Advice

Dr. Mainak Baksi
General Practitioner
13 Years • MBBS , MD (MPH)
Howrah
Mainak Baksi Clinic, Howrah
(50+ Patients)

Dr. Shesham Srinidhi
General Practitioner
5 Years • MD(physician)
Hyderabad
Apollo 24|7 Clinic, Hyderabad
(150+ Patients)

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Ashita Kuruvilla
General Practitioner
7 Years • MBBS
Kolkata
KVC CLINIC, Kolkata

Dr. Debdatta Pati
Psychiatrist
18 Years • MBBS, DPM, MD (PSYCHIATRY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata