Dermatomyositis Symptoms, Causes, and Treatment Options
Dermatomyositis is a rare autoimmune disease causing muscle weakness and a distinct skin rash. Learn about its symptoms, causes, diagnosis, treatment options, and daily management strategies to improve quality of life.

Written by Dr. Siri Nallapu
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026
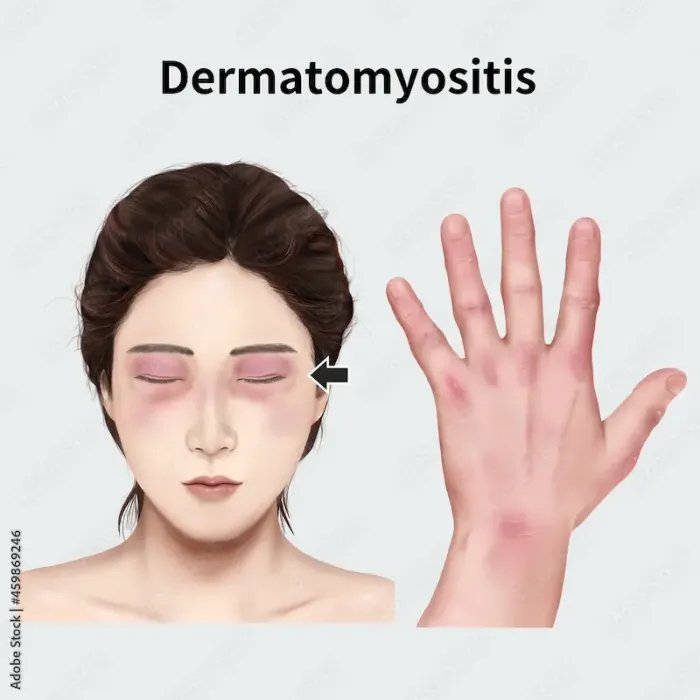
Have you noticed a strange, violet-colored rash on your eyelids alongside unexplained muscle weakness that makes climbing stairs a struggle? These seemingly unrelated symptoms could be signs of a rare condition called dermatomyositis. This inflammatory disease is more than just a skin deep issue; it's a chronic autoimmune disorder where the body's immune system mistakenly attacks its own muscles and skin. The journey from first noticing symptoms to getting a definitive diagnosis can be long and frustrating, often filled with uncertainty. This article will serve as your comprehensive guide, breaking down everything you need to know about dermatomyositis—from its distinctive red flags and underlying causes to the latest diagnostic methods and effective treatment strategies. We'll explore how to manage the condition day-to-day and how to advocate for your health. If your symptoms persist beyond two weeks, consult a doctor online with Apollo24|7 for further evaluation.
What is Dermatomyositis? An Overview
Autoimmunity and Muscle Inflammation
Dermatomyositis is classified as an idiopathic inflammatory myopathy. In simpler terms, it's a disease causing muscle inflammation ("myositis") and a distinctive skin rash ("dermato"), with no known exact cause ("idiopathic"). It is an autoimmune condition, meaning the body's natural defense system, designed to fight off viruses and bacteria, goes haywire and launches an attack on its own tissues—specifically, the small blood vessels within muscles and skin. This attack leads to inflammation, which subsequently causes the hallmark symptoms: muscle damage and weakness, and various skin manifestations.
Who is Affected? Demographics and Risk Factors
Dermatomyositis can affect both adults and children (where it's known as Juvenile Dermatomyositis or JDM). In adults, it most commonly appears in their late 40s to early 60s. Women are about twice as likely as men to develop the condition. While the exact cause remains elusive, certain risk factors have been identified, including a genetic predisposition that may be triggered by environmental factors like viral infections, sun exposure, certain medications, or even cancer. It's a rare disease, affecting an estimated 9 to 10 people per million, which often contributes to delays in diagnosis.
Recognizing the Signs: Symptoms of Dermatomyositis
Characteristic Skin Rash and Changes
The skin involvement in dermatomyositis is often the most visible clue and can sometimes appear even before muscle weakness begins.
The Heliotrope Rash and Gottron's Papules
Two of the most tell-tale signs are the heliotrope rash and Gottron's papules. The heliotrope rash is a purplish or reddish rash that appears on the upper eyelids, often with accompanying swelling. Gottron's papules are raised, scaly, red or violet bumps that appear over the knuckles, elbows, knees, or ankles. Unlike eczema or psoriasis, these rashes are highly characteristic of this autoimmune disease.
Other Dermatological Signs
Other common skin symptoms include a red rash on the face, neck, shoulders, upper chest, and back (often called the "V-neck" or "shawl" sign), cuticles that become red and ragged, and dilated blood vessels visible at the nail folds. Another sign is "mechanic's hands," where the skin on the sides of the fingers becomes rough and cracked.
Progressive Muscle Weakness
The muscle inflammation leads to a symmetric weakness, meaning it affects both sides of the body equally. This weakness is typically progressive and proximal, meaning it primarily affects muscles closest to the trunk of the body—the shoulders, hips, and thighs. Patients may find it difficult to rise from a chair, climb stairs, lift objects, or even comb their hair. In some cases, neck muscle weakness can make it hard to hold the head up, and involvement of the throat or esophagus can lead to swallowing difficulties (dysphagia) and speech changes.
Systemic and Overlapping Symptoms
Beyond the skin and muscles, dermatomyositis is a systemic disease. Patients often experience severe fatigue, general malaise, unintentional weight loss, and low-grade fever. A serious and common complication is interstitial lung disease (ILD), which causes inflammation and scarring of lung tissue, leading to a dry cough and shortness of breath. It's also crucial to be aware of its association with an increased risk of underlying malignancy, making cancer screening a vital part of the initial diagnostic workup.
How is Dermatomyositis Diagnosed?
The Diagnostic Process
Diagnosing dermatomyositis requires a multifaceted approach, as no single test is conclusive. The process usually begins with a thorough physical exam where a doctor will assess the characteristic rash and test muscle strength. Due to the complexity of this inflammatory myopathy, patients are typically referred to a rheumatologist or a neurologist for specialist care.
Key Diagnostic Tests
A combination of tests is used to confirm the diagnosis, rule out other conditions, and assess the extent of the disease.
Blood Tests
Blood tests look for evidence of muscle inflammation. Elevated levels of muscle enzymes like creatine kinase (CK) and aldolase in the bloodstream indicate muscle damage. Doctors also test for specific autoantibodies, such as anti-Mi-2, anti-Jo-1, and anti-MDA-5, which can help confirm the diagnosis and predict potential complications (e.g., MDA-5 is associated with rapidly progressive ILD). Apollo24|7 offers convenient home collection for these crucial blood tests.
Consult a Specialist for the best advice
Electromyography (EMG) and Muscle Biopsy
An EMG involves inserting a thin needle electrode into the muscle to record its electrical activity. In dermatomyositis, it can identify muscle weakness caused by inflammation. A muscle biopsy, however, is often considered the gold standard. A small sample of muscle tissue is removed and examined under a microscope to reveal characteristic inflammatory changes and damage, providing a definitive confirmation.
Imaging (MRI)
Magnetic Resonance Imaging (MRI) can detect inflammation and swelling in muscles before significant weakness occurs. It is a non-invasive tool that can help guide where to perform a muscle biopsy for the most accurate results.
Treatment and Management Strategies
First-Line Medications
The primary goal of treatment is to reduce inflammation, suppress the errant immune response, improve muscle strength and skin symptoms, and prevent complications. Corticosteroids like prednisone are the first-line treatment for rapid inflammation control. Due to the long-term side effects of high-dose steroids, doctors simultaneously prescribe steroid-sparing immunosuppressants like methotrexate, azathioprine, or mycophenolate mofetil to allow for a lower steroid dose.
Advanced Therapies
For patients who don't respond adequately to first-line treatments, several advanced options are available. Intravenous Immunoglobulin (IVIG) is a blood product infusion that can help modulate the immune system. Biologic therapies, such as Rituximab, have also shown promise in treating refractory cases of dermatomyositis.
The Role of Therapy and Supportive Care
Physical therapy is crucial for maintaining range of motion, preventing muscle atrophy, and gradually rebuilding strength. Occupational therapy can teach energy conservation techniques and recommend adaptive devices to help with daily activities. Furthermore, because sun exposure can worsen the skin rash, strict sun protection—using high-SPF sunscreen, wearing protective clothing, and avoiding peak sun hours—is a non-negotiable part of daily management.
Potential Complications and Associated Conditions
Two significant complications require ongoing vigilance. Calcinosis, the formation of painful calcium deposits under the skin or in the muscle, is more common in Juvenile Dermatomyositis but can occur in adults. Interstitial Lung Disease (ILD) is a leading cause of morbidity, requiring regular lung function tests and sometimes targeted therapy. Most critically, adults with dermatomyositis have a significantly elevated cancer risk compared to the general population. This risk is highest in the first few years after diagnosis, necessitating a thorough initial cancer screening (e.g., CT scans, mammograms, colonoscopies, etc.) and continued surveillance.
Living with Dermatomyositis
Living with a chronic illness requires adaptation. A balanced diet, tailored exercise during remission, and pacing activities to manage fatigue are essential. The emotional toll is also significant. Connecting with support groups through organizations like The Myositis Association can provide invaluable community, resources, and psychological support to help patients and their families cope.
Conclusion
Understanding dermatomyositis is the first powerful step toward managing it effectively. While it is a serious chronic condition with potential complications like interstitial lung disease, advancements in treatment have significantly improved the prognosis and quality of life for those diagnosed. The journey involves a careful partnership with your healthcare team, a commitment to your treatment plan, and a focus on adaptive lifestyle changes. Remember, you are not alone. Leveraging support networks and staying informed are your greatest tools. If you are experiencing persistent muscle weakness or an unexplained rash, it is essential to seek professional medical advice. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24|7 for a comprehensive evaluation and personalized care plan.
Consult a Specialist for the best advice
Consult a Specialist for the best advice

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Bhargav Vuppumalla
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD GENERAL MEDICINE
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr D M Karthik
General Practitioner
4 Years • MBBS, Fellowship in Diabetes Mellitus, Advance certificate in Diabetes Mellitus, Derma Nutrition Certification
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Ritesh Motghare
General Practitioner
18 Years • MBBS PGCDM
Nagpur
HEALTH CENTRE VNIT NAGPUR, Nagpur
Consult a Specialist for the best advice

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Bhargav Vuppumalla
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD GENERAL MEDICINE
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr D M Karthik
General Practitioner
4 Years • MBBS, Fellowship in Diabetes Mellitus, Advance certificate in Diabetes Mellitus, Derma Nutrition Certification
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Ritesh Motghare
General Practitioner
18 Years • MBBS PGCDM
Nagpur
HEALTH CENTRE VNIT NAGPUR, Nagpur
More articles from Dermatomyositis
Frequently Asked Questions
1. What is the life expectancy for someone with dermatomyositis?
With modern treatments, most people with dermatomyositis have a normal life expectancy. The prognosis is highly individual and depends on the severity of symptoms, the presence of complications (especially interstitial lung disease or cancer), and how well the patient responds to treatment. Early and aggressive management is key to a positive long-term outcome.
2. Is dermatomyositis considered a disability?
Yes, depending on its severity, dermatomyositis can be considered a disability. The progressive muscle weakness and chronic fatigue can significantly impair a person's ability to perform daily activities and work. Many patients qualify for disability benefits. It's important to discuss this with your doctor and document all limitations thoroughly.
3. What is the difference between polymyositis and dermatomyositis?
The key difference is the skin involvement. Polymyositis also causes muscle inflammation and weakness but does not include the characteristic skin rash of dermatomyositis. Dermatomyositis also has distinct features on muscle biopsy and is more commonly associated with cancer risk.
4. Can dermatomyositis go into remission?
Yes, dermatomyositis can go into remission, where symptoms significantly improve or disappear entirely. Remission is often achieved and maintained with ongoing medication. Some patients may be able to reduce their medication dosage, but relapse is common, so long-term management under a doctor's supervision is necessary.
5. Are there any specific triggers for a dermatomyositis flare-up?
Common triggers for a flare-up include viral infections, excessive sun exposure, stress, surgery, or stopping medications too quickly. Identifying and avoiding personal triggers, in consultation with your doctor, is an important part of managing the disease.

