Understanding Dermatomyositis
Understand dermatomyositis, a rare inflammatory disease that affects muscles and skin. Learn about its symptoms, causes, diagnosis, treatment options, and ways to manage the condition effectively.

Written by Dr. Shaik Abdul Kalam
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Introduction
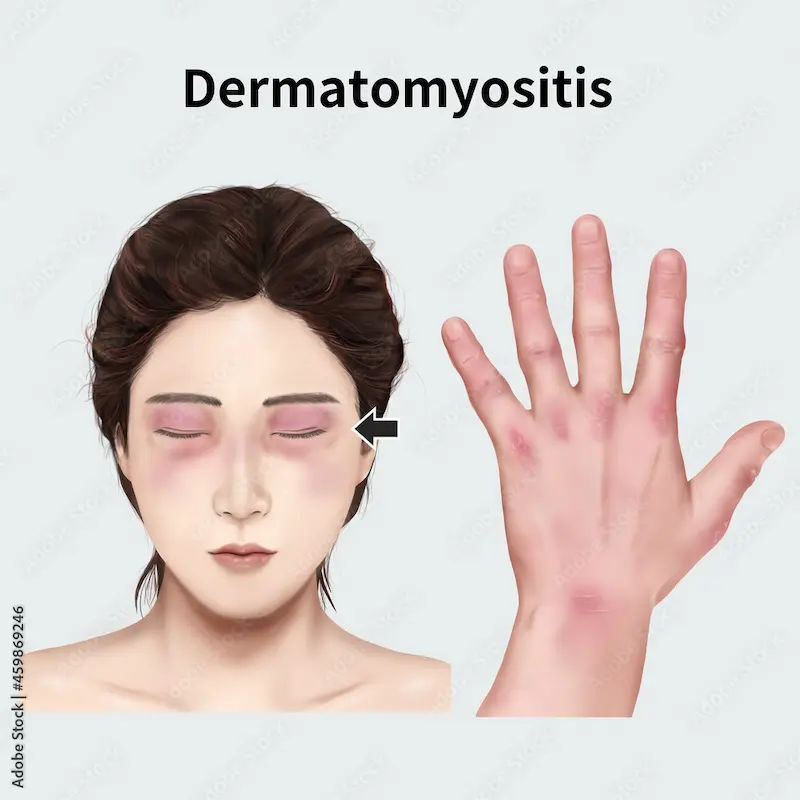
Have you noticed a strange, violet-colored rash on your eyelids or knuckles, accompanied by unexplained muscle weakness that makes climbing stairs or lifting objects a struggle? These could be more than just isolated issues; they might be signs of a rare condition called dermatomyositis. This inflammatory disease is a type of autoimmune disorder where the body's immune system mistakenly attacks its own muscles and skin. Navigating a dermatomyositis diagnosis can feel overwhelming, but understanding the condition is the first step toward effective management. This article will serve as your comprehensive guide, breaking down everything you need to know—from identifying the hallmark symptoms of dermatomyositis and understanding its potential causes to exploring the latest treatment options and strategies for living well with this chronic condition. We’ll empower you with knowledge to have informed conversations with your healthcare provider.
What is Dermatomyositis?
Dermatomyositis is a rare inflammatory disease marked by muscle weakness and a distinctive skin rash. The term itself provides clues: "dermo" refers to skin, and "myositis" means muscle inflammation. It is one of a group of diseases known as inflammatory myopathies.
An Autoimmune Disorder
At its core, dermatomyositis is an autoimmune disorder. Normally, your immune system defends against foreign invaders like viruses and bacteria. In autoimmune conditions, this system malfunctions and produces antibodies that attack the body's own tissues—in this case, the small blood vessels within muscle tissue and skin. This attack leads to inflammation, which causes the characteristic muscle damage and skin changes.
How It Differs from Polymyositis
It's often grouped with a similar condition called polymyositis. The key difference is the presence of skin involvement. Polymyositis causes muscle inflammation and weakness but does not feature a rash. The appearance of the skin rash is what definitively separates dermatomyositis from other muscle diseases.
Consult a Top Dermatologist
Recognizing the Signs: Dermatomyositis Symptoms
Symptoms can develop gradually or appear suddenly. They vary from person to person but typically involve both the skin and muscles.
Skin Changes and Rashes (The Hallmark Sign)
The skin manifestations are often the first and most noticeable clue. These rashes can appear before, after, or simultaneously with muscle weakness and are frequently made worse by sun exposure (photosensitivity).
The Heliotrope Rash
This is a unique, reddish-purple or dusky violet rash that appears on the upper eyelids. It is often accompanied by swelling and is a classic sign of dermatomyositis.
Gottron's Papules and Gottron's Sign
Another hallmark is a rash over the knuckles, elbows, knees, and ankles. It can appear as raised, scaly, reddish bumps called Gottron's papules, or as a flat, reddened patch known as Gottron's sign.
Muscle Weakness and Myopathy
The muscle weakness associated with dermatomyositis is progressive and symmetrical, meaning it affects both sides of the body. It primarily impacts the muscles closest to the trunk, such as those in the hips, thighs, shoulders, upper arms, and neck. This can make it difficult to:
- Rise from a chair
- Climb stairs
- Lift arms to brush hair or reach overhead
- Lift the head from a pillow
Other Common Symptoms
- Fatigue and general malaise
- Difficulty swallowing (dysphagia)
- Muscle pain or tenderness
- Scaly, rough, dry skin that may resemble psoriasis
- Hard lumps under the skin (calcinosis), especially in children
- Fever
- Weight loss
What Causes Dermatomyositis?
The exact cause of dermatomyositis remains unknown. However, researchers have strong theories about the mechanisms at play.
The Role of the Immune System
As an autoimmune disease, the primary problem is immune dysregulation. In dermatomyositis, autoantibodies are created that target specific cellular components within muscle and skin. This triggers a complement system, a part of the immune system to damage the small blood vessels (capillaries) in these tissues. The resulting reduced blood flow is what leads to muscle fiber degeneration and the visible skin changes.
Potential Triggers and Risk Factors
While the root cause is unclear, certain factors may trigger the onset of the disease in genetically predisposed individuals:
- Genetics: Certain genetic markers may increase susceptibility.
- Infections: A previous viral or bacterial infection might act as a trigger.
- Environmental Exposures: UV light exposure, certain medications, and even smoking have been studied as potential contributors.
Cancer: In adults, dermatomyositis can sometimes be a paraneoplastic syndrome—a remote effect of an underlying cancer. This association is why newly diagnosed adults often undergo cancer screening.
Potential Complications of Dermatomyositis
If left untreated, the disease can lead to several serious complications.
Calcinosis
This occurs when calcium deposits form in lumps under the skin or in the muscle. These hard, painful deposits can break through the skin's surface, leading to infections and ulcers. Calcinosis is more common in juvenile dermatomyositis.
Interstitial Lung Disease (ILD)
This is a serious complication where the lung tissue becomes scarred and stiff, making it difficult to absorb oxygen. Symptoms include a dry cough and shortness of breath. Certain autoantibodies, like anti-MDA5, are strongly associated with rapidly progressive ILD. If you experience a persistent dry cough or worsening breathlessness, it is crucial to consult a doctor immediately for evaluation.
How is Dermatomyositis Diagnosed?
Diagnosing dermatomyositis can be complex because it is rare and shares symptoms with other conditions. A combination of assessments is used.
Medical History and Physical Examination
A doctor will start by taking a detailed history of your symptoms and performing a physical exam to assess muscle strength and inspect the skin rash.
Blood Tests and Muscle Enzyme Levels
Blood tests are crucial. They can detect:
- Elevated muscle enzymes: such as Creatine Kinase (CK) and Aldolase, which leak into the bloodstream from damaged muscles.
- Autoantibodies: Specific dermatomyositis-associated antibodies (e.g., anti-Mi-2, anti-Jo-1, anti-MDA5) can help confirm the diagnosis and predict potential complications. Apollo24|7 offers convenient home collection for these tests, allowing for a more comfortable diagnostic process.
Electromyography (EMG) and MRI
- EMG: Measures the electrical activity in muscles, identifying patterns of inflammation and damage typical of myositis.
- MRI: Can detect areas of muscle inflammation and edema (swelling) before significant muscle breakdown occurs. It can also guide the site for a muscle biopsy.
Muscle and Skin Biopsy
This is often the gold standard for diagnosis. A small sample of muscle tissue or affected skin is removed and examined under a microscope. The biopsy can reveal characteristic inflammatory changes and blood vessel damage, confirming the diagnosis.
Dermatomyositis Treatment: Managing the Condition
While there is no cure for dermatomyositis, treatment is highly effective at controlling symptoms, improving muscle strength and skin rash, and preventing complications. The goal is to achieve remission.
First-Line Medications: Corticosteroids and Immunosuppressants
- Corticosteroids (e.g., Prednisone): These powerful anti-inflammatory drugs are usually the first treatment. High doses are used initially to quickly control inflammation, then slowly tapered down.
- Immunosuppressants: To reduce the steroid dosage and its side effects (steroid-sparing agents), drugs like Methotrexate, Azathioprine, or Mycophenolate are often added. These suppress the overactive immune system.
Advanced Therapies: IVIG and Biologics
For more severe or treatment-resistant cases:
- Intravenous Immunoglobulin (IVIG): An infusion of donated antibodies that can help modulate the immune system and block harmful antibodies.
- Biologics: Drugs like Rituximab target specific parts of the immune system (like B-cells) and have shown promise in difficult cases.
Physical and Occupational Therapy
Therapy is a cornerstone of management. A physical therapist designs exercises to maintain and improve muscle strength and flexibility. An occupational therapist helps you learn ways to perform daily tasks more easily, conserving energy and protecting your joints.
Skin Care and Sun Protection
Managing the skin rash is critical:
- Use high-SPF (50+) broad-spectrum sunscreen daily.
- Wear protective clothing and wide-brimmed hats.
- Topical corticosteroids or calcineurin inhibitors can be prescribed for the rash.
- Antimalarial drugs like Hydroxychloroquine are often very effective for controlling skin symptoms.
Living with Dermatomyositis: Diet and Lifestyle Tips
A holistic approach can significantly improve quality of life. A balanced diet rich in anti-inflammatory foods (like fruits, vegetables, and omega-3 fatty acids) can be beneficial. Staying active within your limits, as guided by your therapist, is key to preventing muscle atrophy. Most importantly, prioritize rest, as fatigue is a major component of the disease. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24|7 to create a personalized and comprehensive management plan.
Dermatomyositis in Children (Juvenile Dermatomyositis)
Juvenile dermatomyositis (JDM) is the pediatric form of the disease. While similar to the adult version, it has key differences: it more commonly causes calcinosis (calcium deposits) and abdominal pain, and it is less frequently associated with cancer. Treatment is also similar, focusing on aggressive control of inflammation to prevent long-term damage and allow for normal growth and development.
Conclusion
Dermatomyositis is a rare but serious condition that requires timely diagnosis and proper medical care. With early treatment, lifestyle adjustments, and ongoing monitoring, many individuals can manage symptoms, improve muscle strength, and maintain a better quality of life. Seeking medical guidance at the first sign of symptoms is crucial for effective management and long-term health.
Consult a Top Dermatologist
Consult a Top Dermatologist
Dr. Mayuri Jain
Dermatologist
11 Years • MBBS, MD Dermatology , Venereology & Leprosy
Delhi
Dr Mayuri Jain Clinic, Delhi
Dr. Kavitha Killaparthy
Dermatologist
23 Years • MBBS,DIPLOMA(DERMATOLOGY,VENEREOLOGY,LEPROSY)
Hyderabad
JDS Skin & Hair Clinic, Hyderabad

Dr Ekansh Shekhar
Dermatologist
10 Years • MBBS MD
Lucknow
Apollo Clinic Hazratganj, Lucknow
Dr.j Girishma
Dermatologist
6 Years • MBBS MD DERMATOLOGY
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
Dr. Praveen Kumar
Dermatologist
5 Years • MBBS, MD DVL
Yenugonda
SVS Hospital ., Yenugonda
Consult a Top Dermatologist
Dr. Mayuri Jain
Dermatologist
11 Years • MBBS, MD Dermatology , Venereology & Leprosy
Delhi
Dr Mayuri Jain Clinic, Delhi
Dr. Kavitha Killaparthy
Dermatologist
23 Years • MBBS,DIPLOMA(DERMATOLOGY,VENEREOLOGY,LEPROSY)
Hyderabad
JDS Skin & Hair Clinic, Hyderabad

Dr Ekansh Shekhar
Dermatologist
10 Years • MBBS MD
Lucknow
Apollo Clinic Hazratganj, Lucknow
Dr.j Girishma
Dermatologist
6 Years • MBBS MD DERMATOLOGY
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
Dr. Praveen Kumar
Dermatologist
5 Years • MBBS, MD DVL
Yenugonda
SVS Hospital ., Yenugonda