What Causes an Ear Infection? Symptoms, Treatment, and Prevention
Learn what causes an ear infection, from blocked Eustachian tubes to viruses. This guide covers symptoms, effective treatments, and prevention tips for both children and adults.

Written by Dr. Shaik Abdul Kalam
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 13th Jan, 2026

That familiar, throbbing earache is a pain almost everyone experiences at some point. An ear infection, known medically as otitis media, is one of the most common reasons parents take their children to the doctor, but adults are certainly not immune. But what exactly is happening inside your ear to cause such significant discomfort? Is it just a random occurrence, or are there specific triggers? This article delves deep into the anatomy, causes, and risk factors behind ear infections. We'll explore everything from the role of the Eustachian tube to why children are more susceptible, arming you with the knowledge to identify symptoms, seek effective treatment, and implement powerful prevention strategies. Understanding what leads to an infection is the first step toward finding relief and safeguarding your health.
Understanding the Anatomy of an Ear Infection
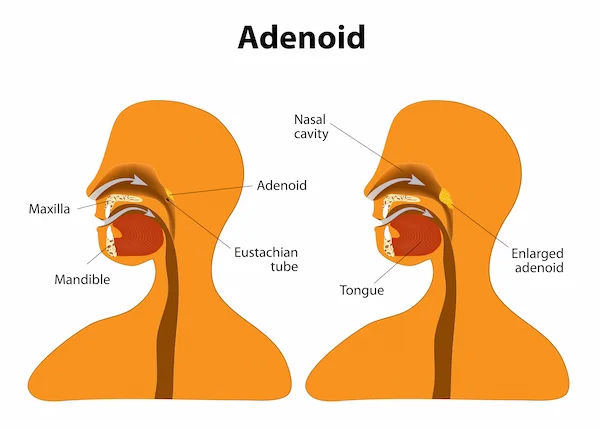
To understand what causes an ear infection, it's helpful to know a bit about the ear's structure. The part usually involved is the middle ear, the air-filled space behind the eardrum that contains tiny vibrating bones. This space is connected to the back of the throat by a narrow channel called the Eustachian tube.
This tube has a critical job: it regulates air pressure in the middle ear, refreshes its air, and drains normal secretions. When the Eustachian tube becomes swollen or blocked—often due to a cold, allergy, or sinus infection—fluid can build up in the middle ear. This stagnant, warm fluid creates a perfect breeding ground for bacteria or viruses, leading to infection and pressure on the eardrum, causing the characteristic pain and swelling.
The Three Main Types of Ear Infections
Not all ear infections are the same. They are categorized based on their location and presentation.
Acute Otitis Media (AOM) - The Most Common Culprit
This is the classic, painful ear infection where parts of the middle ear are infected and swollen, and fluid is trapped behind the eardrum. Symptoms like ear pain and fever are prominent. It often comes on quickly and is the most frequent type.
Otitis Media with Effusion (OME) - The Silent Infection
OME occurs when fluid (effusion) remains in the middle ear after the initial infection has passed. There may be no symptoms of active infection like pain or fever, but the trapped fluid can cause a feeling of fullness and mild, temporary hearing loss. It's often discovered during a routine check-up.
Swimmer's Ear (Otitis Externa) - An Outer Ear Problem
Unlike AOM and OME, swimmer's ear is an infection of the outer ear canal. It's typically caused by water remaining in the ear after swimming, creating a moist environment that aids bacterial growth. It can also result from scratching the ear canal. Symptoms include itchiness, redness, and pain when the outer ear is tugged.
The Primary Causes: Bacteria, Viruses, and Blockages
The direct cause of an ear infection is typically a bacterial or viral pathogen. The most common bacteria are Streptococcus pneumoniae and Haemophilus influenzae, while viruses like those causing the common cold or flu are frequent culprits. However, these germs are only part of the story. The real trigger is often a failure in the ear's drainage system.
How Eustachian Tube Dysfunction Triggers Infection
Eustachian tube dysfunction is the linchpin in the development of most middle ear infections. In children, these tubes are narrower, shorter, and more horizontal than in adults, making them easier to block. When the tube is obstructed, it can't perform its duties. Negative pressure builds up in the middle ear, and normal fluids can't drain. This suction can actually pull bacteria and viruses from the nose and throat into the middle ear space, where they multiply in the trapped fluid, leading to a full-blown infection.
The Role of Preceding Illnesses (Colds, Flu, and Allergies)
Often, an ear infection is not a standalone event but a complication of another illness. A common cold, the flu, or even allergies can cause inflammation and mucus production in the upper respiratory tract. This inflammation can swell shut the Eustachian tubes. Allergies, in particular, can cause chronic inflammation and blockage, making individuals more prone to recurrent infections.
Key Risk Factors: Who is Most Vulnerable?
While anyone can get an ear infection, certain factors significantly increase risk.
Why Children are More Prone to Ear Infections
Immature Immune Systems: Young children are still building immunity to common viruses and bacteria.
Eustachian Tube Anatomy: As mentioned, their smaller, more horizontal tubes are easier to block.
Adenoid Size: Adenoids are gland-like tissues near the Eustachian tubes that are relatively larger in children and can interfere with tube opening if they become infected or swollen.
Lifestyle and Environmental Risk Factors
Group Childcare: Children in group settings are exposed to more colds and other childhood illnesses, increasing opportunities for an ear infection to develop.
Infant Feeding: Babies who drink from a bottle while lying down are more likely to develop infections than those who are breastfed, as breastfeeding provides antibodies and a better feeding angle.
Seasonal Factors: Ear infections are most common during fall and winter when colds and flu are rampant. Seasonal allergies in spring and fall can also spike cases.
Exposure to Smoke: Secondhand tobacco smoke severely irritates the Eustachian tubes and increases inflammation, making infection much more likely.
Altitude Changes: Changes in air pressure can affect Eustachian tube function.
Consult Top Specialists
From Earache to Fever
Identifying an ear infection early leads to quicker relief.
Symptoms in Adults and Older Children
Ear pain (earache), usually sharp, dull, or throbbing.
A feeling of fullness or pressure in the ear.
Fluid drainage from the ear (a sign of a possible small tear in the eardrum).
Muffled hearing or temporary hearing loss.
Signs to Look for in Infants and Toddlers
Since young children can't describe the pain, look for:
Tugging or pulling at an ear.
Fussiness and excessive crying, especially when lying down.
Trouble sleeping.
Fever, particularly in infants.
Fluid draining from the ear.
Clumsiness or problems with balance.
Difficulty hearing or responding to quiet sounds.
How Doctors Diagnose an Ear Infection
If you suspect an ear infection, a doctor will use a lighted instrument called an otoscope to look at the eardrum. A healthy eardrum is pinkish-gray and translucent. An infected eardrum will be red, bulging, and may have fluid or bubbles behind it. They may also use a pneumatic otoscope to puff a small amount of air at the eardrum to see if it moves normally—a stiff eardrum suggests fluid buildup. In cases of recurring infections, a hearing test or tympanometry (which measures eardrum movement) may be recommended.
Effective Treatment Options for Relief
The Wait-and-See Approach and Home Remedies
Many ear infections clear up on their own as the body fights the infection. This is especially true for mild cases. Doctors often recommend a 48-72 hour "wait-and-see" period for certain children. During this time, pain relief is key:
Over-the-counter pain relievers like ibuprofen or acetaminophen.
Warm compress held against the ear.
Hydration and rest to help the immune system.
When are Antibiotics Necessary?
Antibiotics are prescribed for severe cases, infections that don't improve on their own, or for children under 6 months. It is crucial to use antibiotics only when necessary to prevent antibiotic resistance. If your symptoms persist beyond two to three days of home management, consult a doctor online with Apollo24|7 for further evaluation and to determine if a prescription is needed.
Proactive Prevention Strategies
You can reduce the risk of ear infections by:
Vaccinating: Ensure your family is up-to-date on flu and pneumococcal vaccines.
Practicing good hygiene: Frequent handwashing prevents the spread of germs.
Avoiding secondhand smoke.
Breastfeeding infants for at least 6 months to pass on immune-boosting antibodies.
Holding babies upright during bottle-feeding.
Managing allergies effectively with the help of a doctor.
Potential Complications of Untreated Ear Infections
While rare, complications can be serious and include:
Hearing loss: Usually temporary but can become permanent if infections are chronic and damage the eardrum or middle ear bones.
Speech or developmental delays: In young children, persistent hearing loss can affect language acquisition.
Spread of infection: Untreated infections can spread to nearby tissues, including the mastoid bone (mastoiditis) or, very rarely, the brain.
Quick Takeaways: Key Points to Remember
Ear infections are often caused by bacterial or viral growth in fluid trapped by a blocked Eustachian tube.
Children are more susceptible due to their anatomy and developing immune systems.
Symptoms include ear pain, pressure, fever, and irritability in infants.
Not all ear infections require antibiotics; many resolve with pain management.
Prevention through vaccination, hygiene, and avoiding smoke is highly effective.
Always consult a doctor for a proper diagnosis, especially for infants or persistent symptoms.
Conclusion
An ear infection is a common yet painful condition rooted in the complex interplay between our anatomy and everyday germs. Understanding that it's often a secondary issue—a complication of a cold, flu, or allergies that blocks the vital Eustachian tube—empowers us to take proactive steps. From recognizing the early signs in a fussy infant to implementing effective prevention strategies for the whole family, knowledge is your first line of defense. While many cases resolve on their own, it is crucial not to ignore persistent symptoms. Professional medical guidance ensures proper treatment and helps prevent potential complications. If you or your child are experiencing signs of a severe or recurring ear infection, don't hesitate to seek expert advice. You can easily book a physical visit to a doctor with Apollo24|7 to get a thorough examination and peace of mind.
Consult Top Specialists
Consult Top Specialists

Dr. Nishant Rana
Ent Specialist
8 Years • MBBS. MS ENT
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Sreeram Valluri
Ent Specialist
15 Years • MBBS, MS ENT, HEAD & NECK SURGERY
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad

Dr. Madhurima Mandal
Ent Specialist
6 Years • MBBS, MS (Otorhinolaryngology)
Bansdroni
Siddhita Healthcare., Bansdroni
Dr. Mahima H
Ent Specialist
5 Years • MBBS,MD - ENT
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Ramalinga Reddy
General Physician
5 Years • MBBS MD General medicine
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
More articles from Ear infections and earache
Frequently Asked Questions
How can I tell if my child's ear infection is getting better?
Signs of improvement include a reduction in fever, decreased irritability, a return to normal sleep patterns, and resumed interest in play and eating. If symptoms like pain and fever persist beyond 48 hours of starting treatment (or the wait-and-see period), contact your doctor.
Are ear infections contagious?
The ear infection itself is not contagious. However, the colds or respiratory illnesses that often precede and cause them are highly contagious. Practice good hand hygiene to prevent spreading the initial germs.
What's the difference between an ear infection and teething pain?
While both can cause fussiness and drooling, teething rarely causes a high fever (>101°F) or symptoms like fluid drainage from the ear. Teething pain is often soothed by chewing and may be accompanied by gum redness, while ear infection pain is more constant and may worsen when lying down.
How long does an ear infection typically last?
The pain from acute otitis media often improves within the first 24-48 hours. The fluid (effusion) behind the eardrum, however, can linger for 3 months or longer after the infection clears, potentially causing temporary muffled hearing.
Can adults get ear infections from swimming?
Yes, adults can absolutely get swimmer's ear (otitis externa), which is an infection of the outer ear canal caused by water retention. To prevent it, dry your ears thoroughly after swimming, avoid inserting objects into the ear canal, and consider using over-the-counter preventive eardrops.