Understanding Ear Infections: Causes, Symptoms, and Relief
Know about ear infections, what it is, causes, types, causes, risk factors, recognising the signs and symptoms, diagnosis, treatment options and prevention of ear infections.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
That deep, throbbing pain inside your ear, the muffled hearing, and the general feeling of discomfort an ear infection is common yet uniquely unpleasant experiences. While often associated with children, adults are certainly not immune. This article demystifies the causes of ear infections, moving beyond the basic "it's an infection" explanation. We'll explore and identify the primary culprits (bacteria, viruses, and fungi), and delve into the risk factors that make some people more susceptible than others. By understanding the "why" and "how" behind ear infections, you'll be better equipped to recognise the symptoms, seek appropriate treatment, and, most importantly, take steps to prevent them from recurring.
What Exactly is an Ear Infection?
An ear infection, known medically as otitis, occurs when a bacterial or viral infection affects parts of the ear. It often causes inflammation and a buildup of fluid behind the eardrum, leading to pain and other symptoms. It's not just a single condition; where the infection occurs defines its type and severity.
Consult an ENT Specialist for Personalised Advice
The Anatomy of the Ear
To understand ear infections, a basic knowledge of ear anatomy is helpful. Your ear is divided into three parts:
- Outer Ear: This includes the part you see (the pinna) and the ear canal, ending at the eardrum (tympanic membrane).
- Middle Ear: This is an air-filled space behind the eardrum that contains tiny vibrating bones (ossicles). It is connected to the back of the nose and throat by the Eustachian tube.
- Inner Ear: This contains the snail-shaped cochlea (for hearing) and the vestibular system (for balance).
The Three Main Types of Ear Infections
Otitis Externa (Swimmer's Ear)
This is an infection of the outer ear canal. It's often caused by water remaining in the ear after swimming, creating a moist environment that promotes bacterial growth. However, scratching the ear or inserting objects like cotton swabs can also damage the skin and lead to an outer ear infection.
Otitis Media (Middle Ear Infection)
This is the most common type, especially in children. It involves an infection in the air-filled space behind the eardrum. It typically starts when a cold, allergy, or upper respiratory infection causes congestion and swelling of the nasal passages, throat, and Eustachian tubes. When these tubes become blocked, fluid builds up in the middle ear, creating a perfect breeding ground for microbes.
Otitis Interna (Labyrinthitis)
This is an infection of the inner ear, which is less common but more serious. It often involves inflammation that affects your balance and hearing. It's frequently viral in origin.
The Primary Culprits: What Causes an Ear Infection?
The pain and pressure of an ear infection are symptoms; the real causes are microscopic organisms and physiological dysfunctions.
Bacterial Invaders
Bacteria are responsible for the majority of painful ear infections. The most common strains include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. These bacteria are often already present in our noses and throats. When the Eustachian tube becomes blocked due to swelling from a cold, these bacteria can travel up into the middle ear and multiply in the trapped fluid, causing a severe inflammatory response. This is why many middle ear infections require antibiotic treatment.
Viral Intruders
Viruses that cause the common cold or flu are also frequent initiators of ear infections. They cause the initial inflammation and congestion that block the Eustachian tube. While the virus itself may not infect the ear, it sets the stage for a secondary bacterial infection. In some cases, viruses can directly cause an ear infection, but these often resolve on their own without antibiotics.
Fungal Infections (Less Common)
Fungal ear infections, or otomycosis, are more prevalent in tropical climates and are a common cause of otitis externa. They thrive in warm, dark, and humid environments like the ear canal. People with diabetes, compromised immune systems, or those who use antibiotic ear drops for prolonged periods are at higher risk.
Beyond Germs: Key Risk Factors and Contributors
While germs are the direct cause, certain factors significantly increase your odds of developing an ear infection.
Age and Anatomical Factors (Why Children Are More Prone)
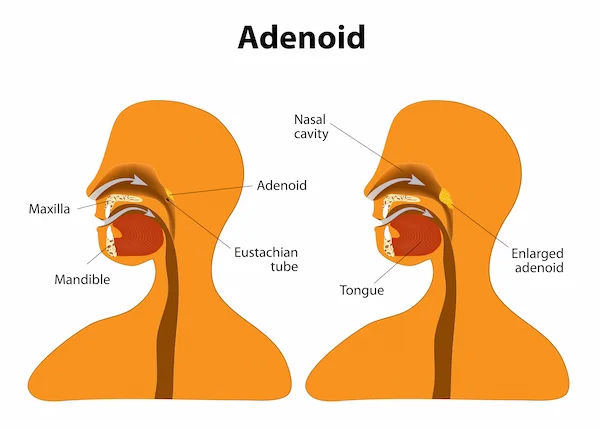
Children between 6 months and 2 years are most susceptible. This is due to their still-developing immune systems and the anatomy of their Eustachian tubes. In kids, these tubes are shorter, narrower, and more horizontal than in adults, making them much easier to block. Furthermore, children's large adenoids (tissue near the Eustachian tubes) can easily swell and obstruct the tubes.
Environmental and Lifestyle Triggers
- Swimming: Frequent exposure to water, especially in lakes or pools with higher bacteria levels, is a leading cause of swimmer's ear.
- Climate and Season: Ear infections are more common during fall and winter when colds and flu are rampant. High humidity and pollution can also contribute.
- Pacifier Use: Studies have shown that children who use pacifiers have a slightly higher incidence of recurring ear infections.
- Secondhand Smoke: Exposure to tobacco smoke irritates the Eustachian tube and increases inflammation, making children particularly vulnerable.
Allergies, Colds, and Sinus Infections
Any condition that causes congestion and mucus production can lead to Eustachian tube dysfunction. Severe allergies can cause chronic inflammation and blockage, creating a persistent risk for fluid buildup and subsequent infection. This is a key reason why managing allergies is crucial for preventing chronic ear problems.
Recognising the Signs: Symptoms of an Ear Infection
Symptoms can vary based on the type of infection and the age of the person.
Symptoms in Adults and Older Children
- Earache: A sharp, sudden pain or a dull, continuous ache.
- Feeling of Fullness: A blocked ear feeling or pressure inside the ear.
- Fluid Drainage: Pus or fluid draining from the ear is a clear sign of a rupture in the eardrum.
- Muffled Hearing: Due to fluid obstruction.
- Sore Throat & Nasal Congestion: Often accompany the ear infection.
Symptoms in Infants and Toddlers
Since young children can't verbalise pain, look for:
- Tugging or pulling at an ear.
- Fussiness and excessive crying, especially when lying down.
- Trouble sleeping.
- Fever (particularly in infants and younger children).
- Loss of appetite or difficulty feeding (swallowing and sucking can change pressure in the middle ear).
- Fluid draining from the ear.
- Clumsiness or problems with balance.
How Are Ear Infections Diagnosed?
A doctor typically uses an otoscope, a lighted instrument to look inside the ear. A healthy eardrum is pearly grey and translucent. An infected eardrum will be red, bulging, and may have fluid or pus behind it. They may also perform a tympanometry test, which measures the eardrum's movement, to confirm the presence of fluid in the middle ear. If your condition does not improve after trying initial home methods, consult a doctor online with Apollo24|7 for further evaluation and a potential diagnosis.
Finding Relief: Treatment Options for Ear Infections
Treatment depends on the type and severity of the infection, as well as the patient's age.
Home Remedies and Pain Management
- For mild cases, especially those likely viral, doctors often recommend a wait-and-see approach for 2-3 days.
- Pain Relievers: Over-the-counter ear infection pain relief medications like ibuprofen or acetaminophen can effectively manage pain and fever.
- Warm Compress: Holding a warm washcloth against the affected ear can soothe pain.
- Hydration and Rest: Supporting the body's immune system is crucial.
Medical Treatments: When to Use Antibiotics
If symptoms are severe, don't improve within 48-72 hours, or if the patient is a young infant, a doctor will likely prescribe antibiotics for an ear infection. It is critical to finish the entire course of antibiotics even if symptoms improve. For swimmer's ear, medicated antibiotic ear drops are the standard treatment. If your symptoms persist beyond two weeks, book a physical visit to a doctor with Apollo24|7 to ensure proper treatment and rule out complications.
Can You Prevent an Ear Infection?
While not always preventable, you can significantly reduce the risk:
- Practice Good Hygiene: Wash hands frequently to prevent the spread of colds.
- Manage Allergies: Keep allergy symptoms under control with medication.
- Avoid Secondhand Smoke.
- Vaccinate: Ensure children receive the pneumococcal conjugate vaccine (PCV13) and the annual flu shot.
- Feed Babies Upright: Avoid giving a bottle to a baby who is lying down.
- Dry Ears Thoroughly: After swimming or bathing, dry your ears completely and tilt your head to help water drain out.
Conclusion
Ear infections, while common and often painful, are usually a temporary setback. Understanding their root causes, from bacterial growth in blocked Eustachian tubes to the environmental triggers like swimming and seasonal colds, empowers you to take proactive steps. While many infections resolve with simple pain management and rest, it's important to know when professional medical intervention is necessary. Persistent symptoms, severe pain, or high fever warrant a doctor's evaluation to prevent potential complications and ensure a swift recovery. By incorporating preventive measures like good hygiene, vaccination, and keeping ears dry, you can significantly reduce the frequency and impact of these infections.
Consult an ENT Specialist for Personalised Advice
Consult an ENT Specialist for Personalised Advice

Dr. Sreeram Valluri
Ent Specialist
15 Years • MBBS, MS ENT, HEAD & NECK SURGERY
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad

Dr. Ravi Y L
Ent Specialist
15 Years • MBBS, MS (ENT)
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(175+ Patients)

Dr. Sreeram Valluri
Ent Specialist
15 Years • MBBS, MS ENT
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir

Dr. Ashwani Kumar
Ent Specialist
11 Years • MBBS, DNB (Otorhinolaryngology)
Delhi
Apollo Hospitals Indraprastha, Delhi
(50+ Patients)

Dr Manoj Jondhale
Ent Specialist
7 Years • MBBS , M.S., DNB, FCPS (Gold Medalist) Fellowship: Fellow in Head Neck Oncosurgery
Mumbai
Apollo Hospitals CBD Belapur, Mumbai
Consult an ENT Specialist for Personalised Advice

Dr. Sreeram Valluri
Ent Specialist
15 Years • MBBS, MS ENT, HEAD & NECK SURGERY
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad

Dr. Ravi Y L
Ent Specialist
15 Years • MBBS, MS (ENT)
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(175+ Patients)

Dr. Sreeram Valluri
Ent Specialist
15 Years • MBBS, MS ENT
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir

Dr. Ashwani Kumar
Ent Specialist
11 Years • MBBS, DNB (Otorhinolaryngology)
Delhi
Apollo Hospitals Indraprastha, Delhi
(50+ Patients)

Dr Manoj Jondhale
Ent Specialist
7 Years • MBBS , M.S., DNB, FCPS (Gold Medalist) Fellowship: Fellow in Head Neck Oncosurgery
Mumbai
Apollo Hospitals CBD Belapur, Mumbai
More articles from Ear infections and earache
Frequently Asked Questions
Is an ear infection contagious?
No, the ear infection itself is not contagious. However, the cold or respiratory illness that preceded it is contagious. The bacteria or viruses that cause these initial illnesses can be spread from person to person.
How long does an ear infection last?
Middle ear infection symptoms usually improve within the first 2-3 days, and most infections clear up completely within 1-2 weeks without any treatment. Swimmer's ear symptoms often start to improve within a few days of starting medicated eardrops.
Can an ear infection cause hearing loss?
Yes, but usually temporarily. The fluid buildup behind the eardrum causes conductive hearing loss, which typically resolves once the infection clears and the fluid drains. Permanent hearing loss is extremely rare from a standard infection but can occur with severe, untreated cases.
What's the difference between an ear infection and an earache?
An earache is a symptom—it's the pain you feel. An ear infection is one of many possible causes of an earache. Other causes can include TMJ disorders, sinus pressure, a sore throat, or a foreign object in the ear.
When should I see a doctor for an ear infection?
You should consult a doctor if symptoms last more than 2-3 days, if the pain is severe, if fluid/pus is draining from the ear, if a fever is present (especially in a young child), or if you suspect an ear infection in an infant under 6 months old.