Essential Guide to Poison Ingestion: Recognition, Types, and Symptoms
Discover key information on poison ingestion, including how to recognise symptoms, common toxins, and important steps to take during an emergency. This guide covers essential actions to manage poisoning effectively.

Written by
Last updated on 13th Jan, 2026
Poison ingestion represents a critical medical emergency that requires swift identification and response. Each year, millions of poisoning cases occur worldwide, with children under six being particularly vulnerable. Understanding various forms of poisoning and their effects enables faster recognition and appropriate emergency action.
Healthcare providers emphasise that the initial hours following ingestion are crucial for successful treatment outcomes. Keep reading for detailed insights into poison ingestion treatments.
Common Types of Poisoning
Household poisoning usually occurs due to accidental ingestion of common cleaning products and chemicals stored in homes. The following substances often attract children due to their bright colours or familiar containers:
Cleaning products (bleach, detergents, drain cleaners)
Personal care items (cosmetics, mouthwash, perfumes)
Medications (both prescription and over-the-counter drugs)
Garage and garden chemicals (pesticides, antifreeze, paint thinners)
Laundry products (pods, fabric softeners, stain removers)
Paint, paint thinners, and other maintenance products
Natural toxins present in plants and certain foods can cause significant poisoning when consumed. Many toxic plants grow in gardens and wild areas. However, the following foods can become dangerous under specific conditions:
Wild mushrooms and toxic fungi
House plants (philodendron, peace lily, pothos)
Contaminated or spoiled foods
Raw or undercooked seafood
Poisonous berries and seeds
Symptoms of Poison Ingestion
Early recognition of poisoning symptoms enables faster treatment response. The following initial signs often appear within minutes to hours after ingestion and vary based on the type of poison:
Nausea, vomiting, and abdominal pain
Burning sensation in mouth, throat, or stomach
Drowsiness or confusion
Difficulty breathing or rapid breathing
Changes in pupil size
Excessive drooling or dry mouth
Severe symptoms develop as the poisoning progresses. This indicates a medical emergency requiring immediate professional intervention. Here are some severe and life-threatening signs of poison ingestion:
Seizures or convulsions
Loss of consciousness or unresponsiveness
Severe difficulty breathing or respiratory arrest
Irregular heartbeat or chest pain
Blue lips or extremities
Severe chemical burns around the mouth or throat
First Aid and Emergency Response
The safety of the person exposed and of the respondent should be prioritised as initial steps for administering first aid when poisoned. Here are some guidelines for first aid:
One must remove the individual from exposure to further toxins and prepare to receive medical aid.
It is essential to call poison control or emergency services immediately for professional guidance.
The person must save any containers, labels, or samples of the poison for identification.
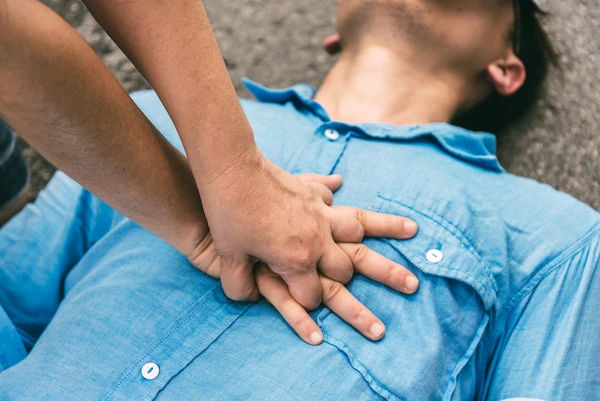
Monitoring vital signs, such as breathing, pulse, and consciousness level, is crucial.
Vomiting should not be induced unless specifically instructed by medical professionals.
Medical emergency services should be contacted immediately in poisoning cases. The below steps can be helpful as emergency responses:
One must dial for emergency assistance immediately if the patient is unresponsive or unable to breathe.
Emergency services should be contacted if the poison involves hydrocarbons or corrosive materials.
Immediate help must be sought if multiple individuals are affected by the same poison.
It is crucial to seek emergency response if the person shows severe symptoms, such as seizures.
Professional help is necessary if the poison is unknown or potentially lethal.
Medical Management of Poisoning
Hospital treatment for poisoning follows established protocols based on the type and amount of poison involved. Medical staff conduct rapid assessments and begin these appropriate interventions:
Immediate assessment of airway, breathing, and circulation
Blood tests to identify toxins and assess organ function
Activated charcoal administration to absorb remaining toxins
Gastric lavage in specific cases under medical supervision
Continuous monitoring of vital signs and organ function
Antidotes play a crucial role in treating particular types of poisoning. Not all poisons have antidotes, but when available, they can be lifesaving in the following ways:
Specific antidotes target known poisons to neutralise their effects.
Timing of antidote administration is critical for effectiveness.
Multiple doses may be required depending on the poison's severity.
Some antidotes can have side effects requiring monitoring.
Antidotes work alongside supportive care measures.
Long-term Impact and Recovery
Poisoning can cause lasting damage to various organ systems. The extent of damage depends on the type of poison and the time before treatment in the following ways:
Liver damage may result in chronic dysfunction or failure.
Kidney damage can lead to long-term filtration problems.
Neurological systems may show persistent effects.
The respiratory system might have reduced function.
The digestive system can develop chronic issues.
Recovery from poisoning requires time and often involves multiple healthcare professionals. The recovery period varies based on poison severity and organ involvement. Patients are usually followed up regularly and may require continued medical support.
Poisoning Prevention Strategies
Proper storage of potentially harmful substances prevents accidental poisoning. Hazardous materials should be kept in their original containers with clear labels. Storage areas must remain locked and inaccessible to children and vulnerable individuals.
Here are a few prevention strategies:
House chemicals must be stored in high cabinets fitted with child-proof locks.
Medications must be kept in secure cabinets away from heat and moisture.
Pesticides and garden chemicals have to be kept in locked outdoor sheds.
Cleaning products should never be transferred to food or beverage containers.
Different types of chemicals must be stored separately to prevent dangerous reactions.
Education plays a vital role in poison prevention. Regular discussions and demonstrations help vulnerable individuals understand potential dangers in their environment in the following ways:
Children should learn to ask adults before touching or consuming unknown substances.
Visual aids and warning symbols help identify dangerous products.
Role-playing scenarios reinforce proper responses to potentially dangerous situations.
Caregivers need training in identifying common household poisons.
Regular family discussions about poison safety create awareness and preparedness.
The Role of Poison Control Centres
Poison control centres provide emergency guidance for poison exposures. They connect callers with trained toxicologists and medical professionals who offer immediate assistance. Here are some important roles poison control centres play:
Assessing the severity of poison exposure through detailed questioning
Providing first-aid instructions specific to the substance involved
Coordinating with emergency services when necessary
Following up on cases to ensure proper treatment and recovery
Legal and Regulatory Aspects
Healthcare professionals should report any suspicions of poisoning cases to the appropriate authorities. Employers are legally mandated to maintain information safety sheets relating to hazardous material.
Property managers are mandated to safely store and dispose of toxic products. Failure to fulfil these statutory requirements may trigger liability and a lawsuit for a causally related injury.
Organisations must maintain accurate records of poison exposure incidents. Regular safety audits ensure compliance with storage and handling regulations.
Mandatory reporting helps authorities track poisoning trends and implement preventive measures. This data supports the development of improved safety standards and regulations.
Conclusion
Poison ingestion remains a significant public health concern requiring continuous vigilance and prevention efforts. Understanding proper storage, education, and emergency response procedures helps reduce poisoning risks.
Poison control centres provide essential services in managing exposures and preventing serious outcomes. Legal frameworks ensure accountability and promote safety standards.
Consult Top General Physicians
Consult Top General Physicians

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Srujana Mulakalapalli
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD (GENERAL MEDICINE)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
(25+ Patients)

Dr. Harshendra Jaiswal
General Physician/ Internal Medicine Specialist
12 Years • MBBS , MD (General medicine)
Kolkata
108 DHANA DHANVANTARI Clinic, Kolkata
(25+ Patients)

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad