Guide to Understanding Neurological Emergencies
Learn the signs, symptoms, and first response steps for neurological emergencies like stroke, seizures, head injuries, and infections to save lives and prevent disability.


Introduction
A sudden, severe headache unlike any you've felt before. An unexpected wave of confusion or weakness on one side of your body. A loved one collapsing into a seizure. Neurological emergencies are frightening, high-stakes medical events that involve the brain, spinal cord, and nerves. They strike without warning and demand immediate action. Your ability to recognise the signs and know how to respond can make the critical difference between life and death, or between a full recovery and long-term disability. This guide is designed to empower you, not to scare you. We will break down the most common types of neurological emergencies, detail their key symptoms, and provide a clear, step-by-step action plan for what to do when every second counts. Understanding these conditions is the first step in protecting yourself and those you care about.
What is a Neurological Emergency?
A neurological emergency is any sudden-onset medical condition where the function of the brain, spinal cord, or nerves is severely compromised, posing an immediate risk to the patient's life or long-term health. These are not like a common headache or a brief dizzy spell. They are characterised by the rapid appearance of dramatic and often debilitating symptoms that signal a crisis within the nervous system.
Why Time is Critical: The Brain and Spinal Cord Under Threat
The phrase "time is brain" is commonly used by doctors to emphasise the urgency of events like a stroke. Brain and spinal cord tissues are extremely delicate and require a constant supply of oxygen and nutrients from blood flow. When this supply is interrupted—by a clot, a bleed, swelling, or an infection—brain cells begin to die within minutes. The longer the condition goes untreated, the more extensive and permanent the damage becomes. This is why rapid recognition and seeking immediate emergency medical care are non-negotiable. There is no time to "wait and see."
Consult a Neurologist for the best advice
Recognising the Most Common Neurological Emergencies
Stroke (Brain Attack)
A stroke occurs when the blood supply to a part of the brain is interrupted or severely reduced. It is a leading cause of adult disability and death worldwide. There are two main types: ischaemic (caused by a clot blocking an artery) and haemorrhagic (caused by a blood vessel bursting and bleeding into the brain).
The FAST Acronym: Remember the Signs
The FAST test is a simple tool to help identify the most common symptoms of a stroke:
F - Face Drooping: Does one side of the face droop or feel numb? Ask the person to smile.
A - Arm Weakness: Is one arm weak or numb? Ask the person to raise both arms. Does one drift downward?
S - Speech Difficulty: Is speech slurred, strange, or impossible to understand? Ask the person to repeat a simple sentence.
T - Time to call for help: If you see any of these signs, even if they go away, call an ambulance immediately.
Other stroke warning signs include sudden numbness in the leg, sudden confusion, trouble seeing in one or both eyes, sudden trouble walking, dizziness, loss of balance, or a sudden severe headache with no known cause.
Ischaemic vs. Haemorrhagic Stroke
While both are catastrophic, the treatment is different. Ischaemic strokes may be treated with clot-busting drugs (thrombolytics) or mechanical clot retrieval, but these are only effective within a narrow time window. Haemorrhagic strokes require controlling the bleed and reducing pressure on the brain. This is why a rapid diagnosis at a hospital is essential.
Seizures and Status Epilepticus
A seizure is a sudden, uncontrolled electrical disturbance in the brain. It can cause changes in behavior, movements, feelings, and levels of consciousness. While many seizures are brief and stop on their own, a neurological emergency occurs when:
A seizure lasts longer than 5 minutes.
A second seizure begins immediately after the first without the person regaining consciousness.
The person has difficulty breathing afterward.
The person is injured during the seizure, is pregnant, or has a known medical condition like diabetes.
Prolonged, continuous seizure activity is called status epilepticus and is life-threatening, as it can cause permanent brain damage.
Traumatic Brain Injury (TBI) and Spinal Cord Injury
These are caused by a sudden trauma from a blow, jolt, or penetrating injury to the head or spine. Emergency signs of a TBI after a fall or accident include:
Loss of consciousness, even briefly.
Repeated vomiting or nausea.
Convulsions or seizures.
Inability to awaken from sleep.
Dilation of one or both pupils.
Slurred speech and weakness/numbness in extremities.
Increasing confusion, restlessness, or agitation.
For a potential spinal cord injury, never move the person unless they are in immediate danger. Look for loss of movement or sensation, intense pain in the back or neck, and an oddly positioned neck or back.
Meningitis and Encephalitis (Brain Infections)
These are infections causing inflammation of the brain (encephalitis) or the protective membranes surrounding it (meningitis). They are medical emergencies. Symptoms can appear suddenly and include:
Sudden high fever with a severe headache.
Stiff neck (nuchal rigidity).
Sensitivity to light (photophobia).
Confusion or difficulty concentrating.
Nausea and vomiting.
In severe cases, seizures.
A key sign is the inability to touch the chin to the chest due to neck stiffness and pain. A rash that doesn't fade under pressure can be a sign of bacterial meningitis and requires instant emergency care.
What to Do in a Neurological Emergency: Your First Response
Step 1: Call for Emergency Help Immediately
Do not hesitate. Do not drive the person to the hospital yourself unless you have absolutely no other choice. Paramedics can begin life-saving treatment on the way to the hospital and alert the emergency department to prepare for arrival.
Step 2: While Waiting for Help – Do's and Don'ts
DO stay calm and reassure the person.
DO note the time when symptoms first started (critical for stroke treatment).
DO if they are conscious, try to keep them still and comfortable. If they are vomiting or drooling, gently roll them onto their side into the recovery position to prevent choking.
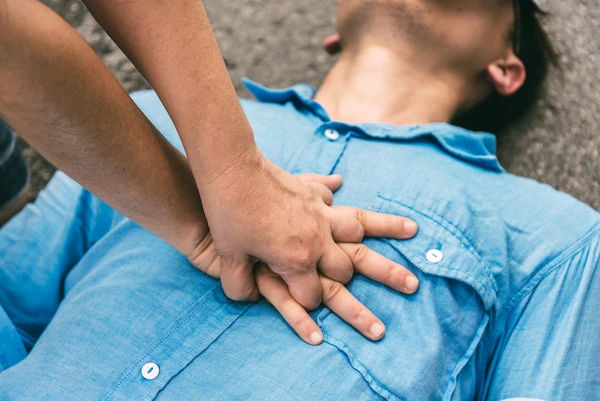
DO perform CPR if they stop breathing and you are trained to do so.
DON'T give them anything to eat or drink, as it could cause choking.
DON'T try to restrain someone having a seizure. Simply clear the area around them and put something soft under their head.
DON'T move anyone you suspect has a neck or spinal injury.
How Are Neurological Emergencies Diagnosed?
Upon arrival at the hospital, the medical team acts quickly. Diagnosis typically involves:
A rapid physical and neurological exam to assess function.
Imaging tests: A CT scan is often the first test to quickly rule out bleeding in the brain. An MRI provides more detailed images of brain tissue.
Blood tests to check for signs of infection, clotting issues, or electrolytes.
Lumbar puncture (spinal tap) may be performed if meningitis or encephalitis is suspected to analyse cerebrospinal fluid.
If your condition is less severe but you have lingering concerns like persistent headaches or dizziness after a minor head injury, consulting a neurologist online with Apollo24|7 can be a good first step for evaluation and guidance.
Prevention and Risk Reduction
While not all neurological emergencies can be prevented, you can significantly reduce your risk by managing underlying health conditions:
Manage Blood Pressure and Cholesterol: This is the number one way to prevent strokes.
Quit Smoking and Limit Alcohol: Both are major risk factors for stroke and other vascular issues.
Control Diabetes: Maintain healthy blood sugar levels.
Wear Protective Gear: Use seatbelts, helmets for biking and sports, and prevent falls, especially in older adults.
Stay Updated on Vaccinations: Vaccines can prevent certain viruses that lead to meningitis and encephalitis.
For those managing chronic conditions, Apollo24|7 offers a convenient home collection for tests like HbA1c and lipid profiles to help you stay on top of your health.
Conclusion
Understanding neurological emergencies is a crucial aspect of personal and public health. The sudden and severe nature of these events can leave people feeling helpless, but knowledge is power. By familiarising yourself with the signs of a stroke, seizure, serious head injury, or brain infection, you transform from a bystander into a vital first responder. Your ability to recognise the red flags and act decisively—by calling for emergency help immediately—can save a life and preserve a future. Share this information with your family and friends. Being prepared isn't about living in fear; it's about living with the confidence that you can protect yourself and your loved ones when it matters most. If you have specific risk factors, speak to a doctor on Apollo24|7 to create a personalised prevention plan.
Consult a Neurologist for the best advice
Consult a Neurologist for the best advice

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS,MD(GENL. MED.),DM(NEUROLOGY)
Kolkata
VDC Clinic, Kolkata
(25+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Avinash Gupta
Neurologist
12 Years • MBBS, DNB - Neurology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)
More articles from Emergency Care
Frequently Asked Questions
1. What is the difference between a stroke and a mini-stroke (TIA)?
A TIA (transient ischaemic attack) produces stroke-like symptoms that typically last only a few minutes and leave no permanent damage. However, a TIA is a major warning sign that a full stroke may be imminent. It should be treated as a neurological emergency and requires immediate medical evaluation to prevent a major stroke.
2. What should I do if I live alone and think I'm having a stroke?
Call for emergency help immediately. Do not hesitate because you are alone. Unlock your door so paramedics can enter. If you can, call a neighbor or family member to let them know. If you have difficulty speaking, try to leave the line open with the emergency dispatcher so they can locate you.
3. Can a very bad migraine be mistaken for a stroke?
Yes, the symptoms can sometimes overlap, including aura, confusion, and weakness (hemiplegic migraine). It can be difficult to tell them apart. The safest rule is to treat it as a potential stroke, especially if it's the 'first and worst' headache of your life or if the symptoms are new to you. When in doubt, get it checked out.
4. How long does a seizure have to last to be dangerous?
Any seizure lasting longer than 5 minutes is considered a medical emergency (status epilepticus) and requires an ambulance. You should also call for help if a person has repeated seizures without regaining consciousness in between.
5. Are sudden severe headaches always a sign of something serious?
Not always, but they can be. A 'thunderclap headache'—a headache that peaks in intensity within 60 seconds—is a classic red flag for a serious issue like a brain bleed (haemorrhagic stroke) or meningitis. Any new, severe, and debilitating headache warrants immediate medical attention.