Hysterectomy Complication Rate
Understand the complication rates associated with hysterectomy procedures, including common risks, factors influencing complications, and tips to reduce risks for a safer recovery.

Written by Dr. Siri Nallapu
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 13th Jan, 2026

Introduction
If you or a loved one is considering a hysterectomy, it’s natural to have concerns about potential complications. A hysterectomy—the surgical removal of the uterus—is a common procedure, often recommended for conditions like fibroids, endometriosis, or cancer. While it can significantly improve quality of life, understanding the possible risks helps in making an informed decision.
This article explains hysterectomy complication rates, what factors influence them, and how you can minimise risks for a smoother recovery.
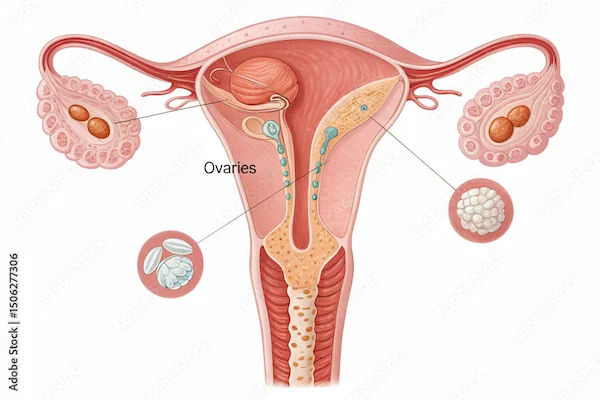
What Is a Hysterectomy?
A hysterectomy involves removing the uterus, and sometimes the cervix, ovaries, or fallopian tubes, depending on the reason for surgery. There are three main types:
1. Total Hysterectomy: Removal of the uterus and cervix.
2. Partial (Supracervical) Hysterectomy: Only the upper part of the uterus is removed.
3. Radical Hysterectomy: Removal of the uterus, cervix, and surrounding tissues (usually for cancer).
The surgery can be performed through:
Abdominal incision
Vaginal approach
Laparoscopic or robotic-assisted
What Are the Common Complications?
While hysterectomies are generally safe, like any surgery, they carry some risks. Complication rates vary depending on the type of hysterectomy, the patient’s health, and the surgeon’s experience.
Short-Term Complications (Within 30 Days of Surgery)
1. Infection: Urinary tract, vaginal, or surgical site infections may occur.
2. Bleeding: Some blood loss is normal, but excessive bleeding may require intervention.
3. Blood Clots: Deep vein thrombosis (DVT) can develop, especially in prolonged recovery.
4. Anaesthesia Risks: Rare but possible reactions like breathing difficulties.
5. Damage to Nearby Organs: The Bladder, bowel, or blood vessels may be accidentally injured.
To Know More Consult Top Gynaecologists
Long-Term Complications (Months or Years Later)
1. Early Menopause: If the ovaries are removed, hormonal changes can trigger menopause symptoms.
2. Pelvic Organ Prolapse: Weakened pelvic muscles may lead to bladder or bowel issues.
3. Chronic Pain: Some women experience persistent pelvic or abdominal discomfort.
4. Emotional Impact: Feelings of loss or depression may arise, especially if fertility is affected.
What Influences Complication Rates?
Several factors determine how likely complications are:
Type of Hysterectomy: Vaginal and laparoscopic procedures typically have fewer complications than abdominal surgeries.
Patient’s Age & Health: Older women or those with diabetes, obesity, or heart disease face higher risks.
Surgeon’s Experience: Skilled surgeons lower complication rates.
Reason for Surgery: Cancer-related hysterectomies may involve more complex procedures.
How Can You Reduce Risks?
Here are some practical steps you can take to reduce the risks associated with hysterectomy surgery:
Before Surgery
Choose an Experienced Surgeon: Ask about their success rates and preferred technique.
Optimise Your Health: Manage chronic conditions like diabetes or hypertension.
Quit Smoking: Smoking increases infection and healing risks.
After Surgery
Follow Post-Op Instructions: Rest, avoid heavy lifting, and keep the incision clean.
Monitor for Warning Signs: Fever, severe pain, or unusual bleeding need immediate attention.
Pelvic Floor Exercises: Strengthening muscles helps prevent prolapse.
Hormone Therapy (if needed): If ovaries are removed, discuss hormone replacement with your doctor.
When to Seek Help?
Contact your doctor if you experience:
High fever or chills
Heavy vaginal bleeding
Severe abdominal pain
Swelling, redness, or discharge from the incision
Difficulty urinating
Conclusion
While hysterectomy complication rates are relatively low, being informed helps you prepare and take preventive steps. If you’re considering this surgery, discuss all options with your doctor to choose the best approach for your health.
If you have concerns or want to explore alternatives, Apollo 24|7 offers consultations with experienced gynaecologists. Book an appointment today for personalised care.
Consult Top Gynaecologists
To Know More Consult Top Gynaecologists

Dr. Sheetal Aggarwal
Obstetrician and Gynaecologist
17 Years • MBBS, MS (Obstetrics & Gynaecology)
Gurugram
Dr Sheetal's clinic, Gurugram

Dr. Mona Yadav
Obstetrician and Gynaecologist
19 Years • MBBS, MD (Obstetrics & Gynaecology)
Dombivli
Nulife multispeciality, Dombivli

Dr. Ramya G S
Obstetrician and Gynaecologist
11 Years • MBBS, DGO - Obstetrics & Gynaecology, DNB - Obstetrics & Gynaecology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Soumya P
Obstetrician and Gynaecologist
6 Years • MBBS,MS (OBST & GYNAE)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Damayanti Pentiyala
Obstetrician and Gynaecologist
27 Years • MBBS, MD
Khammam
Kinnera Hospital, Khammam
(275+ Patients)
Consult Top Gynaecologists

Dr. Sheetal Aggarwal
Obstetrician and Gynaecologist
17 Years • MBBS, MS (Obstetrics & Gynaecology)
Gurugram
Dr Sheetal's clinic, Gurugram

Dr. Mona Yadav
Obstetrician and Gynaecologist
19 Years • MBBS, MD (Obstetrics & Gynaecology)
Dombivli
Nulife multispeciality, Dombivli

Dr. Ramya G S
Obstetrician and Gynaecologist
11 Years • MBBS, DGO - Obstetrics & Gynaecology, DNB - Obstetrics & Gynaecology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Soumya P
Obstetrician and Gynaecologist
6 Years • MBBS,MS (OBST & GYNAE)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Damayanti Pentiyala
Obstetrician and Gynaecologist
27 Years • MBBS, MD
Khammam
Kinnera Hospital, Khammam
(275+ Patients)