Post-Hysterectomy Care: Essential Do's and Don'ts
Discover the essential do’s and don’ts after a hysterectomy to support recovery, reduce complications, and promote better healing.

Written by Dr. Vasanthasree Nair
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Introduction
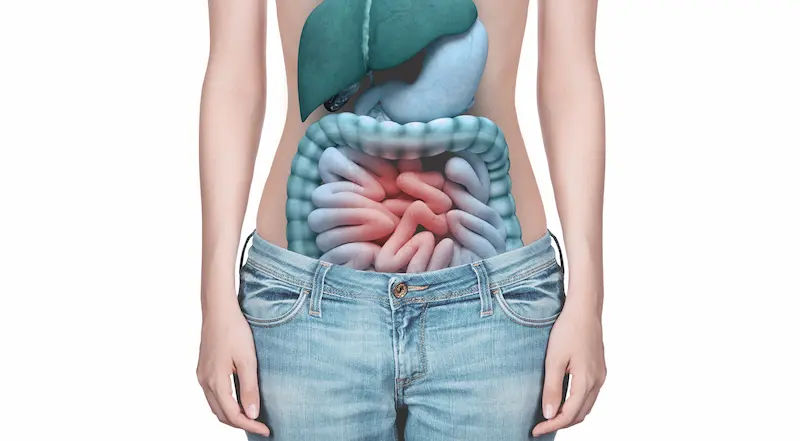
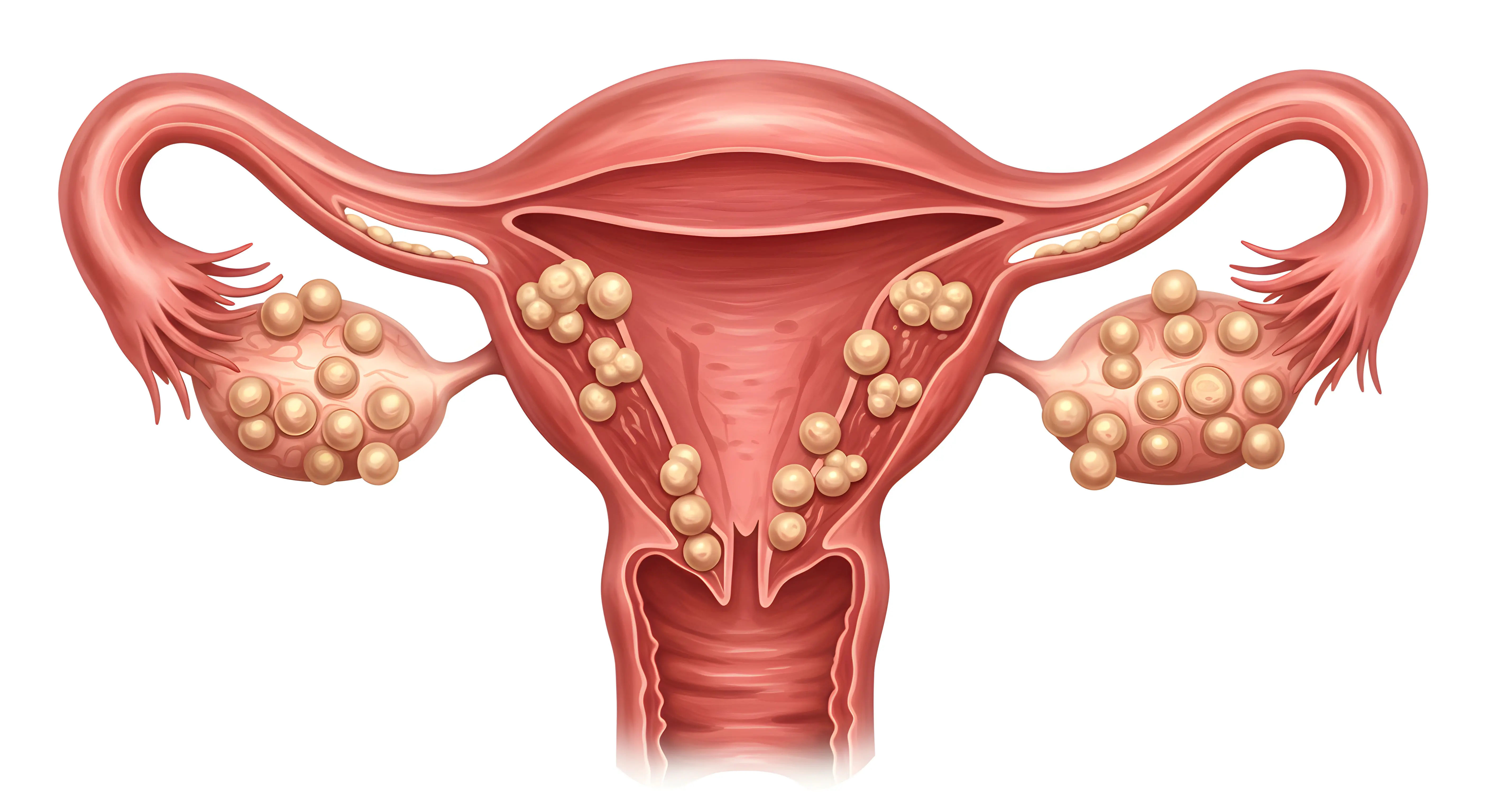
Undergoing a hysterectomy is a major surgery, and a smooth recovery is crucial for returning to your normal life with strength and vitality. The weeks following your procedure are a dedicated time for healing, and knowing what to expect can make all the difference. This comprehensive guide is designed to walk you through the essential do's and don'ts of post hysterectomy care, from the first few hours after surgery to the weeks ahead. We'll cover everything from pain management and incision care to nutrition, activity, and emotional well-being. Whether you had an abdominal, laparoscopic, or vaginal hysterectomy, these evidence-based tips will empower you to navigate your recovery journey confidently, avoid complications, and support your body's incredible healing process. Remember, every woman's experience is unique, so always prioritise the specific instructions from your healthcare team.
The First 24-48 Hours: Immediate Post-Op Care
The initial period after your surgery is about managing immediate post-operative effects and setting the stage for healing. You'll likely be in the hospital during this time, with nurses closely monitoring you.
Do: Manage Your Pain Effectively
Don't try to tough it out. Effective pain management is not a luxury; it's a critical part of recovery. It allows you to breathe deeply, move more easily, and rest properly, all of which prevent complications like pneumonia and blood clots. Take your prescribed pain medication on schedule, even if you feel okay. Staying ahead of the pain is much easier than trying to chase it down once it's severe.
Do: Focus on Deep Breathing
Anaesthesia can cause shallow breathing, increasing the risk of lung infections. Practice deep breathing exercises every hour while awake. Inhale slowly through your nose, feeling your abdomen expand, and exhale slowly through your mouth. Using an incentive spirometer (provided by the hospital) is also highly effective for keeping your lungs clear.
Don't: Ignore Your Fluid Intake
Anaesthesia and pain medications can cause constipation. Hydration is your first defense. Start with sips of water or ice chips and gradually increase as tolerated. Proper hydration also helps maintain blood pressure and aids in overall healing. If you experience nausea, inform your nurse, as they can provide medication to help.
Consult a Gynaecological Surgeon for the best advice
The First Two Weeks: Rest, Heal, and Recover
Once you're home, your focus shifts to creating a peaceful environment for recovery. This phase is arguably the most important for setting a positive trajectory.
Do: Listen to Your Body and Rest
Your body is using a tremendous amount of energy to heal internally. Fatigue after surgery is normal and expected. Plan to nap frequently throughout the day. Set up a comfortable recovery station with pillows, water, snacks, medications, books, and a phone charger within easy reach. This is not the time to be a hero; it's the time to be a patient.
Do: Prioritise Walking and Gentle Movement
While rest is key, so is gentle movement. Walking after hysterectomy is the best exercise during recovery. It stimulates circulation, preventing dangerous blood clots, and helps restore normal bowel function. Start with short, slow walks around your house every few hours. Gradually increase to walking down your driveway or street as you feel able. Listen to your body and stop if you feel pain.
Don't: Lift Anything Heavy
This is the golden rule. Most surgeons impose a strict lifting restriction of nothing heavier than 5-10 pounds (about a gallon of milk) for at least the first six weeks. This includes toddlers, heavy grocery bags, laundry baskets, and vacuum cleaners. Lifting strains your abdominal muscles and internal stitches, risking bleeding, injury, or poor healing of the vaginal cuff.
Don't: Strain During Bowel Movements
Constipation is a common challenge due to pain meds and reduced activity. Straining puts undue pressure on your healing tissues. To avoid constipation after surgery, follow a fibre-rich diet, stay hydrated, and use stool softeners as recommended by your doctor. Don't wait; start stool softeners as soon as you are home.
Nutrition and Hydration: Fueling Your Recovery
The right foods and fluids provide the building blocks your body needs to repair tissue and regain strength.
Do: Eat a Fibre-Rich Diet
To combat constipation, focus on the best foods to eat after hysterectomy that are high in fibre. Think fruits (prunes, berries, pears), vegetables (broccoli, leafy greens), and whole grains (oatmeal, whole-wheat toast). Small, frequent meals are often easier to digest than three large ones.
Do: Stay Hydrated
Continue drinking plenty of water throughout the day. Herbal teas, broth, and diluted fruit juices also contribute to your fluid intake. Proper hydration keeps tissues supple and helps flush out anaesthesia and medication from your system.
Don't: Consume Gas-Producing Foods Initially
For the first week or so, your digestive system may be sluggish. Avoid foods known to cause gas and bloating, such as beans, cabbage, carbonated drinks, and fried foods. This can help minimise the discomfort of post-surgical gas pain, which can sometimes radiate to the shoulder.
Incision and Personal Care
Proper care of your incision site is vital to prevent infection and ensure a clean scar.
Do: Keep Your Incision Clean and Dry
Gently wash the area with mild soap and water during your shower and pat it completely dry. Let it air out for a bit each day. Wear loose, comfortable clothing made from breathable fabrics like cotton to avoid irritation.
Don't: Take Baths or Soak in Water
Until your surgeon gives you the all-clear (usually at your post-op appointment around 6 weeks), you must stick to showers. Submerging your incision in a bath, hot tub, or swimming pool can introduce bacteria and lead to a serious infection.
Don't: Use Products on Your Incision
Avoid applying powders, lotions, oils, or antibiotic creams to your incision unless specifically instructed by your doctor. These can irritate the skin and trap moisture.
Weeks 3-6: Gradually Increasing Activity
As you approach the end of the initial recovery period, you'll likely start feeling more like yourself. The key is to increase activity gradually.
Do: Slowly Increase Your Walking Distance
If short walks are feeling easy, you can gradually extend your distance and duration. Pay attention to how you feel during and after. A little muscle soreness is normal, but sharp or pulling pain is a sign to pull back.
Don't: Engage in Strenuous Exercise or Chores
Even if you feel great, your internal tissues are still healing. This is not the time to return to running, weight lifting, cycling, or intense aerobic classes. Similarly, avoid heavy housework like mopping, vacuuming, or changing bed linens. Wait for your doctor's explicit permission at your follow-up visit.
The Emotional Journey After Hysterectomy
Recovery isn't just physical. The emotional changes after hysterectomy can be significant, influenced by anesthesia, pain meds, hormonal shifts (if ovaries were removed), and the psychological impact of the surgery itself.
Do: Acknowledge Your Feelings
It's normal to experience a rollercoaster of emotions, from relief and gratitude to sadness, anxiety, or mood swings. Allow yourself to feel these emotions without judgment. Journalling can be a helpful outlet.
Do: Seek Support
Talk to your partner, a trusted friend, or a family member about what you're experiencing. Consider joining a post hysterectomy support group, either online or in person. Connecting with others who have been through the same experience can be incredibly validating and reassuring.
When to Call Your Doctor: Recognizing Red Flags
While some discomfort is normal, certain symptoms require immediate medical attention.
Signs of Infection
Fever over 100.4°F (38°C).
Redness, swelling, warmth, or pus-like drainage from your incision.
Foul-smelling vaginal discharge.
Increasing abdominal pain.
Signs of Blood Clots
Pain, redness, warmth, and swelling in one calf (signs of Deep Vein Thrombosis - DVT).
Sudden shortness of breath, chest pain, or coughing up blood (signs of Pulmonary Embolism - PE). This is a medical emergency; seek help immediately.
Other Concerning Symptoms
Heavy vaginal bleeding (soaking a pad in an hour).
Pain or burning when urinating, or inability to urinate.
Persistent nausea or vomiting.
Fainting or dizziness.
If you experience any of these red flag symptoms, do not wait. Consult a doctor online immediately with Apollo24|7 for further evaluation, or proceed to the nearest emergency room.
Returning to Normal Life
Gradually resuming daily activities is key to a smooth recovery.
Resuming Work
The timeline depends on your surgery type and job demands. Desk jobs may be manageable in 3-4 weeks, while physically demanding jobs may require 6-8 weeks or more. Get clearance from your doctor before returning.
Resuming Sexual Activity
This is a common concern. Pelvic rest after hysterectomy is typically mandated for 6-8 weeks to allow the vaginal cuff to heal completely. Never resume intercourse before your doctor examines you and gives the go-ahead. When you do, go slowly, use lubrication, and communicate with your partner.
Conclusion
Recovering from a hysterectomy is a journey that requires patience, self-compassion, and a dedicated focus on healing. By following these essential do's and don'ts, you are actively investing in a smooth and successful recovery. Remember that this period of rest is temporary but its impact on your long-term health is permanent. Use this time to reconnect with your body, allow others to care for you, and gradually rebuild your strength. Every day will bring small improvements. Trust the process, follow your doctor's specific advice, and be proud of the strength it took to undergo this procedure. If you have any concerns at any point during your recovery, your medical team is your best resource.
Consult a Gynaecological Surgeon for the best advice
Consult a Gynaecological Surgeon for the best advice

Dr. Sravanthi Pandala
Obstetrician and Gynaecologist
9 Years • MBBS, MMS(OBG).,FMAS.,F.ART.,DRM(Germany).,
Nellore
Apollo Speciality Hospitals, Nellore
(100+ Patients)

Dr. Lavanya S
Obstetrician and Gynaecologist
14 Years • MBBS., MD(Obstetrics & Gynaecology)
Nellore
Apollo Speciality Hospitals, Nellore
(150+ Patients)

Dr. Savitha Shetty
Obstetrician and Gynaecologist
24 Years • MBBS, MRCOG, MD (Obs & Gyn) , DGO
Bengaluru
Apollo Hospitals Sheshadripuram, Bengaluru
(200+ Patients)

Dr. Damayanti Pentiyala
Obstetrician and Gynaecologist
27 Years • MBBS, MD
Khammam
Kinnera Hospital, Khammam
(275+ Patients)

Dr. Abhishek Daga
Obstetrician and Gynaecologist
20 Years • MBBS, MS (Obstetrics & Gynaecology)
Kolkata
Gynae Care Fertility Centre, Kolkata
(150+ Patients)
More articles from Endometriosis
Frequently Asked Questions
1. What is the best way to sleep after a hysterectomy?
A. The best way to sleep after hysterectomy is on your back with a pillow under your knees to take pressure off your abdomen. If you're a side sleeper, try transitioning to your side with a pillow between your knees and another supporting your belly for comfort and alignment.
2. How long will I need to take pain medication?
A. This varies. Most women rely on prescription pain meds for the first few days to a week at home, then transition to over-the-counter options like ibuprofen or acetaminophen as needed. Always follow your doctor's dosing instructions.
3. When can I drive after my hysterectomy?
A. Generally, you can drive when you are no longer taking opioid pain medication and can react quickly without pain. This is typically around 2-4 weeks post-op. Test your ability by sitting in the car and simulating braking movements. Always get your surgeon's approval first.
4. Is it normal to feel emotional and cry after surgery?
A. Absolutely. The emotional changes after hysterectomy are very common due to a combination of factors: anesthesia, pain medications, hormonal fluctuations, and the psychological impact of the surgery. Be gentle with yourself; it's a normal part of the process.
5. What happens at my 6-week post-op appointment?
A. Your doctor will examine your incision and may perform an internal exam to check that your vaginal cuff is healed. This is when you'll get clearance for activities like bathing, intercourse, and more strenuous exercise, provided everything has healed correctly.