High Eye Pressure: A Silent Threat to The Optic Nerve
Learn how high eye pressure can silently damage the optic nerve, its symptoms, causes, and ways to protect your vision.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
Imagine a delicate cable carrying millions of visual signals from your eye to your brain. This is your optic nerve, and it's incredibly vulnerable to one thing: pressure. Elevated pressure inside the eye, known medically as intraocular pressure (IOP), is a primary factor behind glaucoma, a leading cause of irreversible blindness worldwide. The insidious nature of this condition lies in its silence; often, there are no early warning signs until significant, permanent damage has already occurred. This article serves as your essential guide to understanding the critical link between pressure inside eyes and potential optic nerve damage. We will demystify how pressure is regulated, explore the conditions it causes, identify your risk factors, and outline the modern diagnostic and treatment strategies that can protect your precious eyesight for years to come.
What Exactly is Intraocular Pressure (IOP)?
Intraocular pressure (IOP) is the fluid pressure inside your eye, much like air pressure inside a tire. It's measured in millimetres of mercury (mmHg). Maintaining a healthy IOP is crucial; it keeps the eye inflated and properly shaped, allowing for clear vision. However, just like an over-inflated tire can damage its structure, excessive pressure inside the eyes can compress and harm the delicate optic nerve at the back of the eye.
The Aqueous Humour: The Key Player in Eye Pressure
The primary determinant of IOP is a clear fluid called the aqueous humour. This isn't the same as tears; it's produced continuously by a structure behind the iris (the ciliary body). This fluid flows through the pupil into the front chamber of the eye, bathing and nourishing the lens and cornea. It then must drain out through a tiny, mesh-like tissue called the trabecular meshwork, located at the angle where the iris and cornea meet. A healthy eye maintains a perfect balance between production and drainage, keeping pressure stable, typically in the range of 10-21 mmHg.
How is Eye Pressure Measured? The Tonometry Test
The only way to know your IOP is through a quick and painless test called tonometry, performed during a comprehensive eye exam. The most common method is the "air puff" test (non-contact tonometry), which uses a brief burst of air to flatten the cornea and estimate pressure. For a more precise measurement, your eye doctor may use an applanation tonometer, which involves a blue light and gently touching the cornea's surface with a small probe after applying numbing drops. This is the gold standard for monitoring ocular hypertension and glaucoma.
Consult a Ophthalmologist for the best advice
When Pressure Becomes a Problem: From Hypertension to Glaucoma
Not all high eye pressure leads to damage, and not all glaucoma is caused by high pressure. Understanding this distinction is key.
Ocular Hypertension: High Pressure Without Damage
Ocular hypertension is diagnosed when your IOP is consistently above 21 mmHg, but your optic nerve appears healthy and you show no signs of vision loss. Think of it as a warning sign. Individuals with this condition are considered "glaucoma suspects" and require more frequent monitoring to ensure damage does not begin. Not everyone with high pressure will develop glaucoma, but their risk is significantly elevated.
Glaucoma: When Pressure Damages the Optic Nerve
Glaucoma is not a single disease but a group of eye conditions that result in progressive damage to the optic nerve. This damage translates to vision loss, starting with the peripheral (side) vision. While high IOP is the biggest risk factor, a form called "normal-tension glaucoma" occurs even when pressure is within the normal range, suggesting that poor blood flow to the nerve is also a critical factor.
The Mechanics of Damage: How Pressure Kills Nerve Cells
The prevailing theory is that elevated IOP physically compresses the axons (the long, thin fibres) of the retinal ganglion cells that make up the optic nerve. This compression at the back of the eye (the optic nerve head) disrupts the flow of essential nutrients and signals to and from the brain. Over time, this leads to cellular dysfunction and, ultimately, the apoptosis (programmed cell death) of these neurons. Once these nerve cells die, they cannot be regenerated, making the vision loss permanent. This is why early detection and intervention are absolutely critical.
Are You at Risk? Key Factors for High Eye Pressure
While anyone can develop high eye pressure, certain factors significantly increase your risk. Age is a major one, particularly being over 60. Family history of glaucoma is a powerful indicator, suggesting a genetic predisposition. Race and ethnicity also play a role; people of African, Hispanic, and Asian ancestry are at higher risk for certain types of glaucoma. Other medical conditions, like severe nearsightedness (myopia), thin corneas, previous eye injuries, and systemic health issues such as diabetes, high blood pressure, and sickle cell anaemia, can also contribute. If you have multiple risk factors, regular dilated eye exams are non-negotiable.
The Silent Thief of Sight: Recognising the Symptoms
The most common type, primary open-angle glaucoma, is notorious for having no symptoms in its early stages. Vision remains normal, and there is no pain. By the time an individual notices patchy blind spots in their peripheral or central vision, the disease is often quite advanced.
Acute Angle-Closure Glaucoma Symptoms
In contrast, acute angle-closure glaucoma is a medical emergency. It occurs when the iris bulges forward, suddenly blocking the drainage angle and causing a rapid, severe spike in IOP. Symptoms are intense and unmistakable:
Sudden onset of severe eye pain
Headache
Nausea and vomiting (accompanying the eye pain)
Seeing halos or rainbows around lights
Blurred vision
Redness in the eye
If you experience these symptoms together, seek immediate medical attention at an emergency room to prevent rapid, permanent vision loss.
How is Optic Nerve Damage Diagnosed?
Diagnosing glaucoma involves far more than just measuring pressure. A comprehensive exam is essential.
The Comprehensive Dilated Eye Exam
Your ophthalmologist will dilate your pupils with eye drops to get a clear, magnified view of the inside of your eye, especially the optic nerve. They will assess its color, size, and shape, looking for signs of cupping, a condition where the central portion of the nerve enlarges as nerve fibres are lost.
Beyond the Pressure Test: Visual Field Testing and OCT
A visual field test maps your entire scope of vision, checking for the subtle, characteristic blind spots that glaucoma causes. Furthermore, Optical Coherence Tomography (OCT) is a revolutionary imaging technology that acts like a microscopic MRI for the eye. It provides high-resolution, cross-sectional images of the retina and optic nerve, allowing doctors to measure the thickness of the nerve fibre layer with incredible precision. This allows for detection of damage long before it shows up on a visual field test, enabling truly early intervention.
Treatment Strategies: Lowering Pressure to Save Your Sight
The goal of all glaucoma treatment is to lower intraocular pressure to a level that will prevent further damage to the optic nerve. This is a lifelong management process.
First-Line Treatment: Prescription Eye Drops
Medicated eye drops are the most common initial treatment. They work in one of two ways: either by reducing the production of aqueous humour or by improving its outflow through the drainage angle. It is vital to use these drops exactly as prescribed, every day, even if you have no symptoms.
Laser Therapy: Trabeculoplasty and Iridotomy
Laser treatments are effective options. For open-angle glaucoma, Selective Laser Trabeculoplasty (SLT) uses a low-energy laser to stimulate the drainage system to work more efficiently. For angle-closure risk, Laser Peripheral Iridotomy (LPI) creates a tiny hole in the iris to improve fluid flow and prevent a sudden attack.
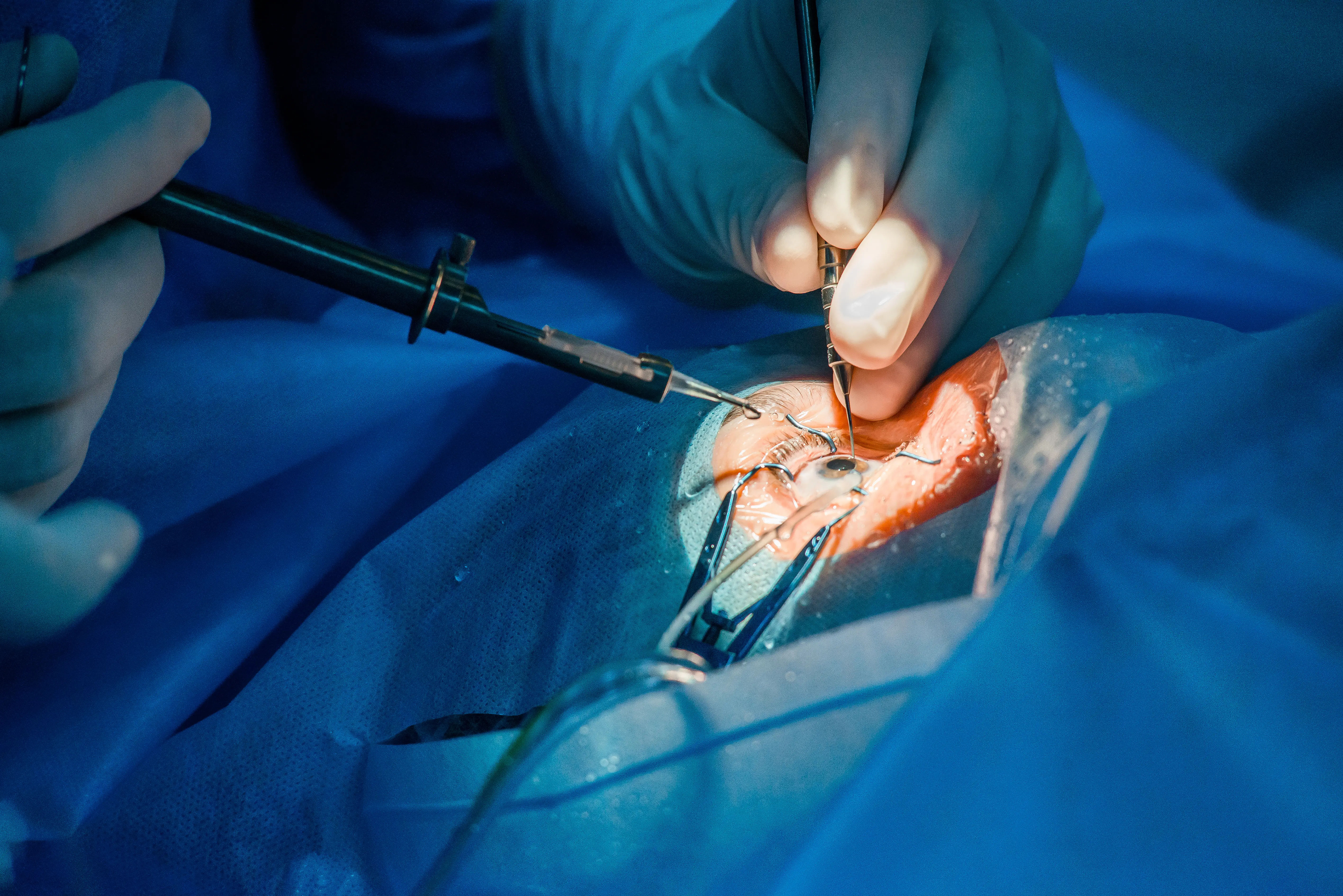
Surgical Options: When Drops and Laser Aren't Enough
If other treatments are insufficient, surgery may be recommended. Minimally Invasive Glaucoma Surgery (MIGS) offers new procedures with faster recovery times. Traditional surgeries like trabeculectomy or the implantation of a drainage device create a new channel for fluid to drain from the eye, effectively lowering pressure.
Can You Prevent High Eye Pressure and Glaucoma?
You cannot prevent glaucoma itself, especially if you have a strong genetic predisposition. However, you can prevent vision loss from glaucoma through proactive care. The single most important thing you can do is to get regular, comprehensive dilated eye exams. This is the only way to catch the disease early. Leading a healthy lifestyle that benefits your overall circulation, such as regular, moderate exercise and a diet rich in leafy greens and omega-3 fatty acids, may also support eye health. Protect your eyes from injury by wearing safety glasses during risky activities. If your condition does not improve after trying these methods, or if you need a specialist's opinion.
Conclusion
The relationship between pressure inside eyes and the health of your optic nerve is one of the most critical in all of ophthalmology. While the threat of glaucoma is real and the potential consequences are severe, the power to protect your vision lies firmly in your hands. Modern medicine offers highly effective ways to monitor, manage, and treat high eye pressure. The key is vigilance. By understanding your personal risk factors, committing to regular check-ups with an eye care professional, and adhering to prescribed treatments, you can successfully manage this condition. Do not wait for symptoms to appear, as that is often too late. Be proactive about your eye health; it is an investment in preserving your ability to see and experience the world around you for a lifetime. Schedule that eye exam today.
Consult a Ophthalmologist for the best advice
Consult a Ophthalmologist for the best advice

Dr. Zennat Tajmin Shah
Ophthalmologist
24 Years • MBBS,DNB (Ophthalmology)
Kolkata
Titanium Eye Care, Kolkata

Dr. Karan Paswan
Ophthalmologist
7 Years • MBBS,MS (Ophthalmology)
Kolkata
VDC Clinic, Kolkata
Dr Aishwarya M Angadi
Ophthalmologist
5 Years • MBBS, MS
Pune
Apollo Clinic, Nigdi, Pune
Dr Kanse Vaibhav
Ophthalmologist
10 Years • MBBS, DO, MS, DNB
Pune
Apollo Clinic, Nigdi, Pune

Dr. Sridhar Annam
Ophthalmologist
15 Years • MBBS, DO, MS (Opthal)
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(25+ Patients)