Guide to Faq On Non Alcoholic Fatty Liver Disease
Get answers to frequently asked questions about Non-Alcoholic Fatty Liver Disease (NAFLD), including symptoms, diagnosis, causes, and the best dietary and lifestyle changes for management.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026
_4.webp?tr=q-80,f-webp,w-350,dpr-2,c-at_max 700w)
Introduction
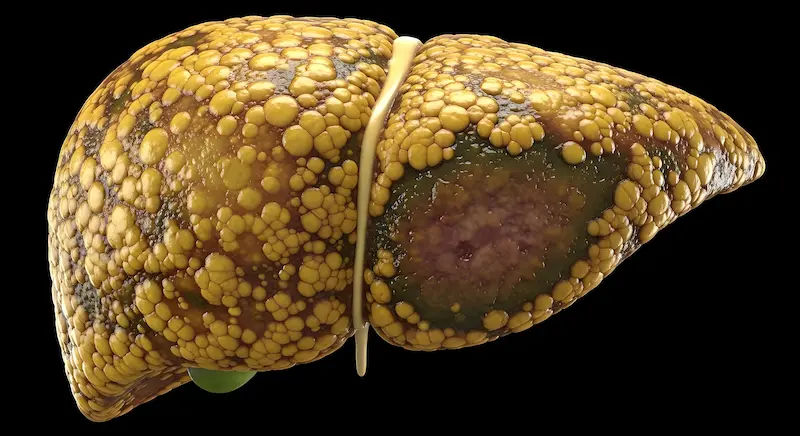
If you’ve been told you have a “fatty liver” on a routine ultrasound or blood test, you’re not alone. Non‑alcoholic fatty liver disease (now often called MASLD—metabolic dysfunction‑associated steatotic liver disease) is one of the most common liver conditions worldwide. Many people have no symptoms, yet the disease can quietly progress over the years if risk factors aren’t addressed. This practical FAQ walks you through what the disease is, who gets it, how it’s diagnosed, and—most importantly—what really works to protect your liver and overall health. You’ll learn how much weight loss makes a difference, the best eating and exercise patterns, which medicines are (and aren’t) helpful, and when to see a doctor. We’ve included evidence-based tips, examples, and new developments, along with easy-to-understand visuals to clarify the science. If symptoms persist beyond two weeks or your liver tests remain abnormal, consider consulting a doctor online with Apollo 24|7 for personalized guidance. Let’s get you confident about your liver and back in charge of your health.
What Is Non‑Alcoholic Fatty Liver Disease (NAFLD/MASLD)?
The condition in plain English
Non‑alcoholic fatty liver disease (NAFLD) describes excess fat stored in the liver of people who drink little to no alcohol. In 2023–2024, experts introduced a new name—metabolic dysfunction‑associated steatotic liver disease (MASLD)—to better reflect the tight links with metabolic health (weight, blood sugar, blood pressure, and lipids). Whichever term you see, the concept is the same: too much fat in liver cells raises the risk of inflammation and scarring over time.
NAFL vs NASH and why it matters
There are two main forms:
- Simple fatty liver (NAFL): Fat accumulates, but there’s minimal inflammation. This often stays stable and is reversible with lifestyle change.
- NASH (non‑alcoholic steatohepatitis): Fat plus inflammation and liver cell injury. NASH can lead to fibrosis (scar tissue), cirrhosis, liver failure, or liver cancer in a subset of people.
Staging the disease
Doctors stage fibrosis from F0 (none) to F4 (cirrhosis). Fibrosis stage predicts long‑term outcomes more than the amount of fat itself. The good news: losing weight and improving metabolic health can halt—and sometimes reverse—fibrosis, especially in early to mid stages.
Unique insight: Think of fatty liver as a “metabolic barometer.” When the liver fills with fat, it often signals broader insulin resistance in muscle and fat tissue. Tackling the whole metabolic picture—food quality, movement, sleep, and stress—helps both the liver and your long‑term heart and kidney health.
How Common Is This Disease and Who Is at Risk?
How many people have it?
Globally, roughly 25–30% of adults have fatty liver, and rates are rising alongside obesity and type 2 diabetes. In some regions and age groups (including adolescents), prevalence is higher.
Key risk factors
- Overweight/obesity, especially central (abdominal) fat
- Type 2 diabetes or prediabetes
- High triglycerides or low HDL cholesterol
- High blood pressure
- Polycystic ovary syndrome (PCOS) and hypothyroidism
- Obstructive sleep apnea (OSA)
- Sedentary lifestyle and diets high in refined carbs and sugary drinks
- Certain medications (e.g., long‑term steroids), though MASLD is usually metabolic.
Lean fatty liver is real
Up to 10–20% of people with NAFLD/MASLD have a normal BMI (“lean NAFLD”), especially in some Asian populations. Risk still tracks with visceral fat, waist size, genetics (e.g., PNPLA3), and metabolic markers. If you have a family history of fatty liver or diabetes, request screening even if you’re not overweight.
Unique insight: Waist size can be more predictive than scale weight. Track your waist circumference and aim for reductions of 5–10 cm over time.
What Are the Signs and Symptoms?
Often silent until advanced
Most people feel fine. When symptoms occur, they’re usually nonspecific: fatigue, mild right‑upper‑abdominal discomfort, or a sense of fullness. Jaundice, swollen legs or abdomen, and confusion are late signs of cirrhosis, not early fatty liver.
When to see a doctor?
- Persistently elevated ALT/AST on routine bloodwork
- Ultrasound showing steatosis (fat)
- Type 2 diabetes with suspected fatty liver
- Signs of advanced disease (jaundice, swelling, easy bruising)
If symptoms persist beyond two weeks or your liver tests remain abnormal for three months, consult a doctor online with Apollo 24|7 for further evaluation and a tailored plan.
Red flags not to ignore
- Rapidly worsening fatigue, yellowing eyes/skin
- Abdominal swelling, leg edema
- Black stools or vomiting blood
- These warrant urgent in‑person care.
Unique insight: Fatty liver itself rarely hurts. Pain is a poor guide. Rely on tests and risk factors rather than symptoms alone to decide on next steps.
How Is Fatty Liver Diagnosed?
Blood tests and scores
- Liver enzymes (ALT, AST): Can be normal even with significant disease.
- Platelets, albumin, and INR help assess advanced disease.
- FIB‑4 score (uses age, AST, ALT, platelets) helps rule out advanced fibrosis in primary care. Low
- FIB‑4 often avoids specialty referral; high or indeterminate FIB‑4 triggers further testing (e.g., FibroScan).
- Apollo 24|7 offers convenient home collection for labs like liver function tests (LFT), lipid profile, and HbA1c, which are often part of the evaluation.
Imaging
- Ultrasound: Common first step; detects moderate‑to‑severe fat but may miss mild cases.
- FibroScan (transient elastography): Quick, noninvasive measure of liver stiffness (fibrosis) and controlled attenuation parameter (CAP) for fat.
- MRI‑PDFF: Most accurate for liver fat in research and some clinical settings.
These tests help distinguish simple fat from fibrotic disease without a biopsy in many cases.
Liver biopsy: who needs it
Biopsy is reserved for unclear cases, suspected advanced fibrosis, or when results will change treatment (e.g., confirming NASH before certain therapies). Most people can be managed without a biopsy by combining noninvasive scores and elastography.
Unique insight: Ask your provider about a “two‑step” pathway—FIB‑4 in primary care, followed by FibroScan if needed. It’s efficient, cost‑effective, and evidence‑based for finding those who truly need specialist care.
Is Fatty Liver Dangerous? Complications to Know
Liver‑related risks
A subset of people with NASH develop progressive fibrosis, cirrhosis (F4), portal hypertension, liver failure, or hepatocellular carcinoma (HCC). Risk rises with older age, diabetes, obesity, and higher fibrosis stage.
Heart disease leads the risk list
For most people with NAFLD/MASLD, the leading cause of illness and death is cardiovascular disease, not liver failure. That’s why treating blood pressure, cholesterol, and blood sugar—and quitting smoking—is as important as reducing liver fat.
Kidney and cancer risks
Fatty liver is associated with chronic kidney disease and some extra‑hepatic cancers. Proactive screening and lifestyle changes can reduce these risks.
Unique insight: Track your “metabolic bundle” every 6–12 months—blood pressure, lipids, HbA1c, weight/waist, and a noninvasive fibrosis assessment when indicated. Steady improvements compound benefits across organs.
What Actually Works to Treat Fatty Liver?
- Weight loss targets that change outcomes
- 3–5% weight loss: reduces liver fat (steatosis)
- 7–10% weight loss: improves inflammation (NASH) and can regress fibrosis
- ≥10%: highest chance of fibrosis regression
- Aim for 0.5–1% body weight loss per week. Even if weight loss plateaus, continued physical activity yields liver and heart benefits.
Eating patterns that help
- Mediterranean‑style diet: Emphasizes vegetables, legumes, whole grains, fish, olive oil, and nuts; consistently improves liver fat and cardiometabolic health.
- Reduce fructose and sugary beverages; limit refined starches.
- Calorie deficit matters most; low‑carb and low‑fat both work if sustainable. In some people with diabetes, a lower‑carb diet can especially reduce triglycerides and liver fat.
- Practical tip: Fill half your plate with non‑starchy vegetables, a quarter with lean protein, and a quarter with whole grains or starchy veg. Swap sugary drinks for water or unsweetened tea.
Exercise specifics
- Target 150–300 minutes/week of moderate aerobic activity (e.g., brisk walking) plus 2–3 days of resistance training.
- Even without weight loss, exercise reduces liver fat and improves insulin sensitivity.
- Micro‑habits: 7,000–10,000 steps/day; 1–2 minute movement breaks every 30–60 minutes of sitting.
Consult a Top General Physician
A realistic one‑week plan
- Mon/Wed/Fri: 35 minutes brisk walking + 10 minutes bodyweight strength (squats, push‑ups, rows)
- Tue/Thu: 25 minutes cycling or swimming
- Sat: Active chores or hike
- Daily: Replace dessert with fruit + yogurt; skip sugary drinks
- This adds up to >180 minutes/week and supports a 300–500 kcal/day calorie deficit.
Unique insight: Consistency beats intensity. A “minimum effective dose” you can repeat for months is better than a heroic week you can’t sustain.
Are There Medications or Supplements?
Approved medication: resmetirom
In 2024, the first medication for noncirrhotic NASH with moderate‑to‑advanced fibrosis (F2–F3)—resmetirom, a thyroid hormone receptor‑β agonist—gained FDA approval in the U.S., improving liver fat and histologic features in trials. It’s considered for carefully selected patients alongside lifestyle therapy, usually by specialists.
Off‑label options in guidelines
- Vitamin E (800 IU/day): May benefit non‑diabetic adults with biopsy‑proven NASH; potential risks (e.g., prostate cancer signal in some studies) must be discussed.
- Pioglitazone: Improves NASH in people with and without diabetes; weight gain and edema are considerations.
- GLP‑1 receptor agonists (e.g., semaglutide): Not yet approved specifically for NASH, but effective for weight loss and can reduce liver fat; widely used in patients with obesity/diabetes.
What to avoid?
- Unproven supplements like high‑dose herbal “liver cleanses” can be harmful. Always review supplements with your clinician.
- Alcohol: If you have fatty liver, keep it minimal or avoid; alcohol plus fatty liver accelerates risk.
Unique insight: Ask your doctor about medications that indirectly help the liver by targeting weight and metabolic health (e.g., GLP‑1 RAs, SGLT2 inhibitors in diabetes). The liver benefits when the whole metabolic picture improves.
Prevention, Screening, and Day‑to‑Day Living
Who should be screened?
- Adults with type 2 diabetes or multiple metabolic risks should be assessed with FIB‑4 and, if needed, FibroScan.
- People with obesity or metabolic syndrome benefit from periodic evaluation even if liver enzymes are normal.
- If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo 24|7.
Daily living tips that add up
- Coffee: 2–3 cups/day (without excessive sugar/cream) is associated with lower liver fibrosis risk.
- Sleep: 7–9 hours; treat sleep apnea if present (improves insulin resistance).
- Stress: Mindfulness, social support, and regular movement help appetite regulation.
- Eating window: Some people find time‑restricted eating (e.g., 10–12‑hour daytime window) supports calorie control. Choose a pattern you can sustain.
Special situations
- Children/teens: Rising rates; emphasize family‑based nutrition changes and active play. Pediatric evaluation is recommended for elevated ALT or obesity with risk factors.
- Pregnancy: Preconception weight optimization and diabetes screening reduce risk; coordinate care with obstetrics and hepatology if you already have liver disease.
- Lean NAFLD: Focus on waist reduction, fitness, and metabolic markers rather than scale weight alone.
Unique insight: Build an “environmental nudge” system—keep high‑fiber foods visible, schedule movement breaks, and set phone reminders for water and short walks after meals to lower glucose spikes.
Myths vs Facts: Quick Clarifications
“I don’t drink, so I can’t have fatty liver.”
- Fact: Most fatty liver today is metabolic, not alcohol‑related.
“Normal liver enzymes mean my liver is fine.”
- Fact: Enzymes can be normal even with fibrosis; use FIB‑4 and elastography when at risk.
“Keto is the only way.”
- Fact: Various diets work if they create a calorie deficit and are sustainable; Mediterranean‑style has the best long‑term evidence.
“Supplements can ‘detox’ my liver.”
- Fact: There’s no shortcut; some supplements are harmful. Focus on diet, activity, and evidence‑based care.
Working With Your Care Team
Who’s on the team?
Primary care, endocrinology/diabetology, hepatology/gastroenterology, dietitians, and sometimes sleep medicine and bariatric surgery. Digital care platforms like Apollo 24|7 can coordinate labs, follow‑ups, and lifestyle coaching.
How often to monitor?
- Every 6–12 months: weight/waist, blood pressure, lipids, HbA1c, LFTs
- FIB‑4 annually (or per clinician advice); FibroScan if FIB‑4 is indeterminate/high
- More frequent checks if you have diabetes or established fibrosis
- Apollo 24|7 offers home collection for HbA1c, lipid profile, and LFTs to simplify follow‑up.
Unique insight: Treat fatty liver like you would high blood pressure—track it, tweak it, and celebrate small improvements—momentum matters.
Conclusion
Fatty liver disease is common, often silent, and strongly linked to our overall metabolic health. The same choices that help your waistline—whole‑food eating, steady movement, restorative sleep, and stress control—also lighten the liver’s load and protect your heart and kidneys. Aim for realistic, sustainable steps: a Mediterranean‑style plate, 7,000–10,000 daily steps, and 150–300 minutes of weekly activity. Track your numbers—weight, waist, blood pressure, lipids, HbA1c—and use simple tools like FIB‑4 and FibroScan to check liver risk. Medications, including the newly approved resmetirom for selected patients, can complement lifestyle changes when appropriate. If your liver enzymes stay elevated, your ultrasound shows fat, or you live with diabetes or multiple metabolic risks, get personalized advice. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo 24|7. Taking charge now can stabilize or even reverse disease progression—and add years of healthy living.
Consult a Top General Physician
Consult a Top General Physician

Dr. Rohinipriyanka Reddy
General Practitioner
9 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Dhankecha Mayank
General Practitioner
6 Years • MBBS
Hyderabad
Apollo 24|7 Clinic - Telangana, Hyderabad

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Utsa Basu
Diabetologist
14 Years • MBBS , MD
Barasat
Diab-Eat-Ease, Barasat
(75+ Patients)

Dr. Santanu Mandal
General Physician/ Internal Medicine Specialist
17 Years • MD (Physician), DNB (General Medicine)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
(25+ Patients)
Consult a Top General Physician

Dr. Rohinipriyanka Reddy
General Practitioner
9 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Dhankecha Mayank
General Practitioner
6 Years • MBBS
Hyderabad
Apollo 24|7 Clinic - Telangana, Hyderabad

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Utsa Basu
Diabetologist
14 Years • MBBS , MD
Barasat
Diab-Eat-Ease, Barasat
(75+ Patients)

Dr. Santanu Mandal
General Physician/ Internal Medicine Specialist
17 Years • MD (Physician), DNB (General Medicine)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
(25+ Patients)
More articles from Fatty Liver
Frequently Asked Questions
Can fatty liver go away?
Yes. Many people reduce liver fat and inflammation with 7–10% weight loss, Mediterranean‑style eating, and regular exercise. Early stages are most reversible. Ask your doctor about tracking progress with FIB‑4 or FibroScan.
What’s the best diet for fatty liver disease?
A Mediterranean diet pattern—vegetables, legumes, whole grains, fish, olive oil, nuts—has strong evidence. Reducing sugary drinks and refined carbs is key. Choose a sustainable calorie deficit to support steady weight loss.
Do I need a FibroScan or a biopsy?
Start with FIB‑4. If it’s low, a FibroScan may not be needed immediately. If FIB‑4 is intermediate/high, FibroScan helps assess fibrosis. Biopsy is reserved for selected cases where results change management.
Are there medications for NAFLD/NASH?
Lifestyle change is foundational. Resmetirom is approved for certain adults with noncirrhotic NASH and fibrosis. Some patients may benefit from vitamin E or pioglitazone (case‑by‑case), and weight‑loss medications like GLP‑1 RAs can indirectly help the liver.
Should I stop drinking alcohol entirely?
If you have fatty liver, minimizing or avoiding alcohol is advisable, as alcohol plus metabolic liver disease raises risks. Discuss what’s safe for you with your clinician.

.webp)