Guide to What Non Alcoholic Fatty Liver Disease Nafld
Learn about NonAlcoholic Fatty Liver Disease (NAFLD). This comprehensive guide explains the causes, symptoms, diagnosis, and treatment options to help you understand and manage your liver health.


Introduction
Your liver is your body's unsung hero, tirelessly performing over 500 vital functions, from filtering toxins to processing nutrients. But a modern day epidemic is silently compromising this crucial organ: NonAlcoholic Fatty Liver Disease (NAFLD). Affecting an estimated 2530% of people globally, NAFLD occurs when excess fat builds up in the liver cells of people who drink little to no alcohol. Often presenting no symptoms in its early stages, it's frequently discovered incidentally during routine blood tests. However, if left unaddressed, this condition can progress to serious inflammation, scarring (cirrhosis), and even liver failure. This comprehensive guide will demystify NAFLD, exploring its causes, symptoms, and, most importantly, the effective strategies you can use to manage and even reverse it, empowering you to take control of your liver health.
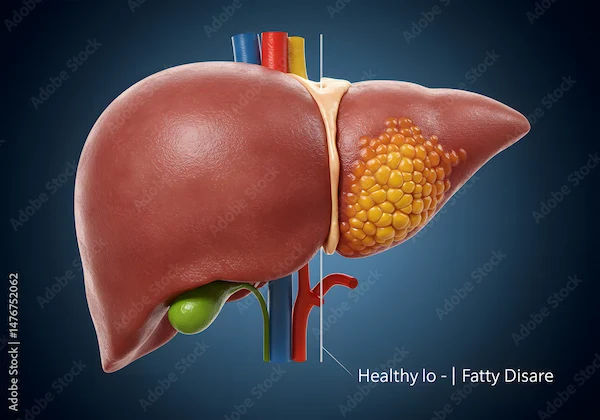
What is NonAlcoholic Fatty Liver Disease (NAFLD)?
NonAlcoholic Fatty Liver Disease (NAFLD) is an umbrella term for a range of liver conditions affecting people who consume little or no alcohol. As the name implies, the primary characteristic is too much fat stored in liver cells. It is intrinsically linked to metabolic health—specifically issues like insulin resistance, obesity, and high blood lipids.
A healthy liver contains little or no fat. Doctors diagnose NAFLD when more than 5% of the liver's weight is fat. It's now the most common cause of chronic liver disease in many Western countries, paralleling the rise in obesity and type 2 diabetes rates.
Consult a Hepatologist for the best advice
NAFLD vs. Alcoholic Liver Disease: What's the Difference?
The key difference is the cause. Alcoholic liver disease is directly caused by excessive alcohol consumption over many years. NAFLD, on the other hand, occurs without that significant alcohol intake. The liver damage in both can look very similar under a microscope, but the driving factors are distinct. Doctors will often ask detailed questions about alcohol use to rule out an alcoholic cause before confirming a NAFLD diagnosis.
The Two Main Types of NAFLD
NAFLD is not a single condition; it exists on a spectrum of severity.
Simple Fatty Liver (Hepatic Steatosis)
- This is the early, more common, and less severe form. It involves fat accumulation in the liver but with little to no inflammation or liver cell damage. Simple fatty liver is generally not considered to cause significant harm on its own and is often reversible with lifestyle changes.
NonAlcoholic Steatohepatitis (NASH)
- This is a more aggressive form of the disease. In NASH, the fat buildup is accompanied by liver inflammation and damage to the liver cells. This inflammation can lead to scarring (fibrosis) of the liver. NASH can progress to advanced scarring (cirrhosis) and liver failure. It is estimated that about 20% of people with NAFLD have NASH.
What Causes NAFLD? The Key Risk Factors
The exact cause of why some people develop NAFLD and others don't isn't fully understood. However, it is strongly associated with a cluster of health issues often referred to as metabolic syndrome.
The Central Role of Insulin Resistance
- This is considered the cornerstone of NAFLD development. Insulin resistance occurs when your body's cells don't respond well to insulin, a hormone that allows sugar (glucose) to enter cells for energy. The pancreas then produces more insulin to compensate. High insulin levels promote the storage of fat, particularly in the liver, initiating the process of NAFLD.
Common Medical Conditions Linked to NAFLD
- Obesity: Over 70% of people with obesity are likely to have NAFLD. Excess fat tissue, especially around the abdomen, contributes to inflammation and insulin resistance.
- Type 2 Diabetes: Insulin resistance is a hallmark of type 2 diabetes, making individuals with this condition highly susceptible to NAFLD.
- High Cholesterol/Triglycerides: High levels of fats, particularly triglycerides, in the blood are a significant risk factor.
- Metabolic Syndrome: This is the combination of at least three of the following: large waist circumference, high blood pressure, high blood sugar, high triglycerides, and low HDL ("good") cholesterol.
- Polycystic Ovary Syndrome (PCOS) and Sleep Apnea are also strongly linked.
Lifestyle and Dietary Contributors
- A diet high in processed foods, sugary beverages (like soda and fruit juice), refined carbohydrates (white bread, pasta), and unhealthy fats (saturated and trans fats) is a major driver. This dietary pattern promotes weight gain and insulin resistance. A sedentary lifestyle further exacerbates these risks.
Recognizing the Signs: Symptoms of NAFLD
The "Silent" Nature of EarlyStage NAFLD
- One of the most challenging aspects of NAFLD is that it is largely a "silent" disease. In the early stages, particularly with simple fatty liver, there are typically no noticeable signs or symptoms. Many people live with it for years without knowing.
Symptoms of Advanced NAFLD and NASH
As the disease progresses to NASH or cirrhosis, symptoms may begin to appear:
- Persistent fatigue and weakness
- Pain or discomfort in the upper right abdomen
- Unexplained weight loss
- Jaundice (yellowing of the skin and eyes)
- Swelling in the abdomen (ascites) or legs (edema)
- Spiderlike blood vessels on the skin
- Itchy skin
If you experience any of these symptoms, especially jaundice or abdominal swelling, it is crucial to consult a doctor online with Apollo24|7 for further evaluation.
How is NAFLD Diagnosed?
Because it's often asymptomatic, NAFLD is frequently first suspected based on abnormal results from routine blood tests.
Initial Blood Tests and Liver Function Tests (LFTs)
- A blood test can show elevated liver enzymes, specifically ALT (Alanine Transaminase) and AST (Aspartate Transaminase). While not definitive for NAFLD (other liver issues can raise these enzymes), it is often the first clue that prompts further investigation. Apollo24|7 offers convenient home collection for tests like liver function panels, making initial screening easier.
Imaging Tests: Ultrasound, FibroScan, and MRI
- Ultrasound: Often the first imaging test used. It can detect the presence of fat in the liver.
- Transient Elastography (FibroScan®): A specialized ultrasound that measures the stiffness of your liver, which indicates fibrosis (scarring). It's a noninvasive alternative to a biopsy for staging the disease.
- MRI: Can provide more detailed images and accurately quantify the amount of fat and scar tissue in the liver.
The Gold Standard: Liver Biopsy
- This is the most accurate way to diagnose NASH and determine the extent of liver damage. A small sample of liver tissue is removed with a needle and examined under a microscope. It confirms the diagnosis, identifies inflammation and scarring, and rules out other liver diseases. It is typically reserved for cases where the diagnosis is unclear or advanced disease is suspected.
The Stages of NAFLD Progression
Understanding the progression is key to understanding the seriousness of the condition.
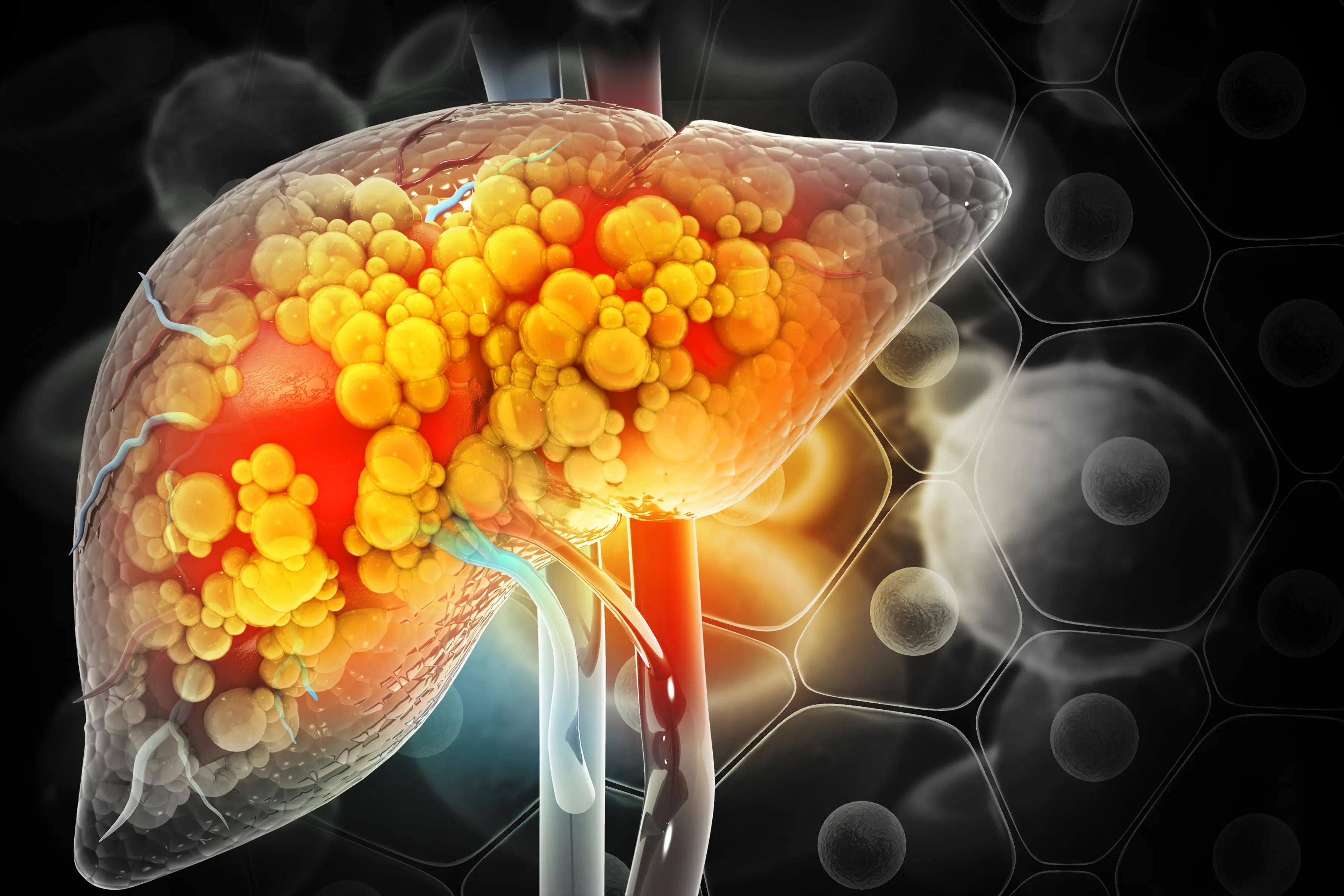
From Simple Fat Buildup to Inflammation (NASH)
- The journey often starts with simple steatosis. For some, this is where it remains. For others, the ongoing fat accumulation and metabolic stress trigger an inflammatory response, turning the condition into NASH.
The Development of Liver Fibrosis and Scarring
- Chronic inflammation from NASH leads to the activation of stellate cells in the liver, which produce collagen, forming scar tissue. This process is called fibrosis. Fibrosis is graded on a scale (F0 to F4). The liver can regenerate, but advanced fibrosis impairs its function.
End Stage: Cirrhosis and Liver Failure
- With continued damage, fibrosis can progress to cirrhosis (F4), where widespread scarring replaces healthy liver tissue. This hard, scarred liver cannot function properly, leading to liver failure. Cirrhosis is irreversible and carries a high risk of liver cancer and the need for a liver transplant.
How to Treat and Manage NAFLD?
The good news? There is no medication specifically approved for NAFLD, yet it is one of the most treatable liver diseases because lifestyle modification is highly effective.
Weight Loss: The Most Effective Strategy
- Weight loss is the cornerstone of NAFLD management. The goal is to lose 710% of your total body weight.
- Studies show that losing just 35% of body weight can reduce liver fat. A 710% loss can improve inflammation and even reverse early fibrosis.
NAFLD Diet: What to Eat and What to Avoid
Focus on a wholefoods, plantforward diet.
- Eat More: Whole grains, vegetables, fruits, legumes, nuts, lean protein (fish, poultry), and healthy fats (olive oil, avocados).
- Avoid/Reduce: Sugary drinks, refined carbs (white bread, pasta, pastries), red meat, and highly processed foods. The Mediterranean diet is often recommended by hepatologists for its proven benefits in improving liver health.
The Importance of Regular Physical Activity
- Aim for at least 150 minutes of moderate intensity exercise (like brisk walking, cycling, swimming) per week. Exercise improves insulin sensitivity and helps with weight loss, even without significant changes on the scale.
Managing Coexisting Conditions (Diabetes, Cholesterol)
- Working with your doctor to tightly control blood sugar if you have diabetes and manage cholesterol and blood pressure levels is crucial. This holistic approach treats the underlying metabolic drivers of NAFLD. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24&7 to create a personalized management plan.
Can NAFLD Be Reversed? The Prognosis
Yes, in its early stages, NAFLD and even early NASH can be reversed. The liver has a remarkable ability to repair itself once the source of the damage is removed. By achieving weight loss through diet and exercise, you can reduce liver fat, decrease inflammation, and even regress fibrosis. The prognosis for most people with NAFLD is excellent if they commit to lifestyle changes. However, once cirrhosis develops, the damage is often permanent, and the focus shifts to managing complications and preventing liver cancer.
Preventing NonAlcoholic Fatty Liver Disease
Prevention mirrors treatment. Adopting a healthy lifestyle is your best defense:
- Maintain a healthy weight.
- Eat a balanced diet rich in whole foods.
- Exercise regularly.
- Limit sugar and processed foods.
- Manage existing health conditions like diabetes.
- Avoid unnecessary medications that can stress the liver.
Conclusion
NonAlcoholic Fatty Liver Disease is a significant but largely manageable health condition. While its silent nature can be concerning, it also means that proactive screening and lifestyle interventions can be incredibly powerful. The key takeaway is that you have a substantial degree of control over your liver health. By understanding the risk factors, recognizing the importance of metabolic health, and committing to sustainable lifestyle changes—primarily through weight management, a nutritious diet, and regular exercise—you can not only prevent NAFLD but also effectively reverse its course if already diagnosed. If you have risk factors, don't wait for symptoms. Talk to your doctor about screening and take the first step towards safeguarding your liver, your body's essential powerhouse.
Consult a Hepatologist
Consult a Hepatologist

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. Akshatha Manjunath
General Surgeon
8 Years • MBBS, MS
Bangalore
Apollo Clinic Bellandur, Bangalore

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Aswin S. Krishna
Hepatologist
10 Years • MBBS, MD (Internal Medicine,MMC), DM (Hepatology, MMC), PDF(Fellowship in Liver Transplanatation)
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)
Consult a Hepatologist for the best advice

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. Akshatha Manjunath
General Surgeon
8 Years • MBBS, MS
Bangalore
Apollo Clinic Bellandur, Bangalore

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Aswin S. Krishna
Hepatologist
10 Years • MBBS, MD (Internal Medicine,MMC), DM (Hepatology, MMC), PDF(Fellowship in Liver Transplanatation)
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)
More articles from Fatty Liver
Frequently Asked Questions
What is the best diet for a fatty liver?
The best diet for fatty liver disease is often based on the Mediterranean diet, which emphasizes fruits, vegetables, whole grains, legumes, nuts, olive oil, and lean proteins like fish. It is low in red meat, sugar, and saturated fats, all of which help reduce liver fat and inflammation.
Can you die from nonalcoholic fatty liver disease?
While simple NAFLD itself is rarely fatal, its advanced complications can be. If it progresses to cirrhosis and liver failure, it can be life threatening. Cirrhosis also significantly increases the risk of liver cancer. This underscores the importance of early management to prevent progression.
How long does it take to reverse NAFLD?
The timeline to reverse NAFLD varies based on the individual and the amount of weight lost. Significant improvements in liver fat can be seen within a few months of consistent lifestyle changes, including a 35% reduction in body weight. Reversing inflammation (NASH) may require a 710% weight loss sustained over a year or more.
Are there any medications to treat NAFLD?
Currently, there are no FDA-approved medications specifically for NAFLD. Treatment focuses on managing the condition through weight loss and controlling associated conditions like diabetes, high blood pressure, and high cholesterol with appropriate medications. Several drugs are in clinical trials.
What are the symptoms of NASH liver disease?
In its early stages, NASH often has no symptoms. As it advances, symptoms may include severe fatigue, weakness, and pain or discomfort in the upper right abdomen. With cirrhosis, symptoms can include jaundice (yellowing skin), abdominal swelling, and confusion.


_2.webp)