Guide to Introduction Fatty Liver Disease
Learn everything about fatty liver disease — its causes, signs to watch for, and steps you can take toward recovery and prevention.”

Introduction
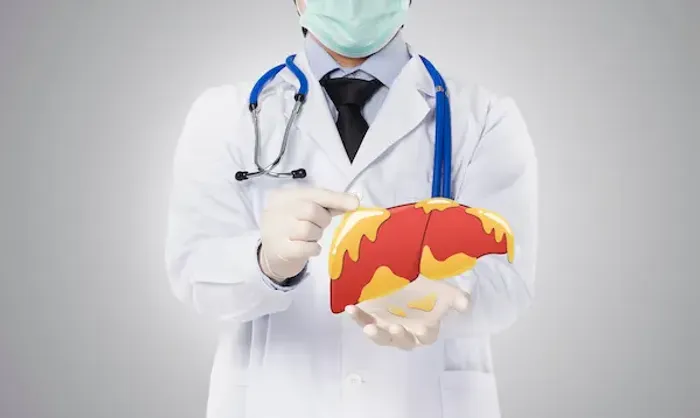
Fatty liver disease is a common condition, affecting millions worldwide, yet it often flies under the radar until it reaches a more advanced stage. Essentially, it occurs when excess fat builds up in the cells of your liver. While a healthy liver contains a small amount of fat, trouble begins when fat constitutes 5% or more of the liver's weight. This comprehensive guide will walk you through everything you need to know about this condition. We'll demystify the two main types—alcoholic and non-alcoholic—unpack the often subtle symptoms, and outline the key risk factors. More importantly, we will focus on the empowering news: for most people, fatty liver disease is reversible with early intervention and the right lifestyle changes. Whether you're looking for prevention tips or management strategies, this article will provide a clear roadmap to understanding and protecting your liver health.
The Two Main Types: Understanding NAFLD and AFLD
Not all fatty liver disease is the same. The primary distinction lies in its cause, which splits the condition into two main categories:
1. Non-alcoholic Fatty Liver Disease (NAFLD): The Silent Epidemic
NAFLD is the most common form of liver disease in Western countries and is not related to heavy alcohol use. It's
closely linked to metabolic syndrome—a cluster of conditions including obesity (particularly around the abdomen), type2 diabetes, high blood pressure, and abnormal cholesterol levels. The rise in NAFLD parallels the global rise in these conditions. It's often called a "silent" disease because it can progress for years without causing any noticeable
symptoms. NAFLD itself can be broken down further:
- Simple Fatty Liver (Steatosis): This is the initial, relatively benign stage where fat is present but little to no inflammation
or liver cell damage exists. - Non-alcoholic Steatohepatitis (NASH): This is a more aggressive form where the fat accumulation is accompanied by
liver inflammation and cell damage. NASH can lead to scarring (fibrosis) and significantly increase the risk of cirrhosis and liver cancer.
2. Alcoholic Fatty Liver Disease (AFLD): The Role of Toxins
As the name implies, AFLD is directly caused by excessive alcohol consumption. The liver is your body's primary
detoxification organ, and processing alcohol can produce harmful substances that damage liver cells, promote
inflammation, and weaken the body's natural defenses. The good news is that alcoholic fatty liver is usually reversible if you stop drinking alcohol completely. However, continued drinking can lead to alcoholic hepatitis and eventually
cirrhosis.
Consult a Specialist for the best advice
Key Risk Factors You Need to Know
Understanding your risk factors is the first step in prevention. While some factors are beyond your control, many are modifiable through lifestyle choices.Major Risk Factors Include:
- Overage 50: The risk increases with age.
- Obesity: A high body mass index (BMI), especially with excess abdominal fat, is a primary driver.
- Type 2 Diabetes and Insulin Resistance: These conditions disrupt how your body processes fuel, encouraging fat storage
in the liver. - High Cholesterol or Triglycerides: Elevated levels of fats in your blood can contribute to fat buildup in the liver.
- Metabolic Syndrome: Having three or more of its components (large waist circumference, high blood pressure, high
blood sugar, high triglycerides, low HDL cholesterol) significantly increases risk. - Rapid Weight Loss or Poor Diet: Diets high in sugar, processed carbohydrates, and saturated fats can overwhelm the
liver. - Certain Medications: Some drugs, like corticosteroids and tamoxifen, can contribute.
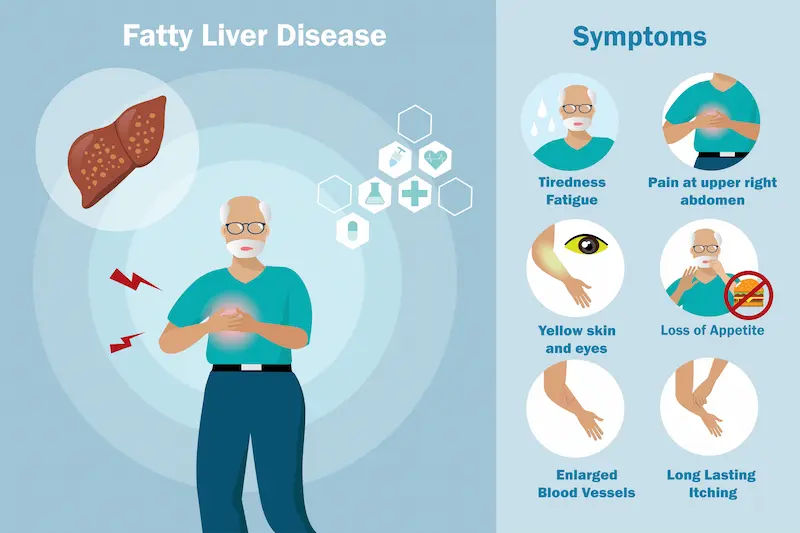
Decoding the Signs: Symptoms of Fatty Liver Disease
Fatty liver disease is notoriously asymptomatic in its early stages, often discovered incidentally during blood tests for
other reasons.
1. Early-Stage Symptoms: Often Silent and Missed
Most people with simple fatty liver or early NASH experience no symptoms at all. If any symptoms do appear, they are
typically vague and non-specific, such as:
- Persistent fatigue or weakness
- A general feeling of being unwell
- Discomfort or mild pain in the upper right abdomen
Advanced-Stage Symptoms: As the disease progresses to cirrhosis (severe scarring), the liver's function is significantly
impaired. Symptoms then become more pronounced and serious:
- Jaundice: Yellowing of the skin and eyes.
- Ascites: Swelling and fluid buildup in the abdomen.
- Easy Bruising and Bleeding: Due to reduced production of clotting factors.
- Confusion or Brain Fog (Hepatic Encephalopathy): Caused by the buildup of toxins affecting the brain.
- Intense Itching: From bile products deposited in the skin.
- Spider-like Blood Vessels: Visible on the skin.
If you experience any of these advanced symptoms, it is crucial to seek immediate medical attention. If symptoms
persist beyond two weeks, consult a doctor online with Apollo24|7 for further evaluation.
Getting a Diagnosis: How Doctors Identify Fatty Liver
Since symptoms are rare early on, diagnosis often relies on a combination of methods. Common blood tests and
imaging are:
- Liver Function Tests (LFTs): A blood test that measures liver enzymes (ALT, AST). Elevated levels can indicate
inflammation or damage. Apollo24|7 offers convenient home collection for tests like these. - Imaging Studies:
- Ultrasound: Often the first test used, as it can easily detect fat infiltration in the liver.
- FibroScan®: A specialised, non-invasive ultrasound that measures liver stiffness, which correlates with fibrosis
(scarring). - The Gold Standard: Liver Biopsy: In uncertain cases or to definitively diagnose NASH and stage the fibrosis, a doctor
may recommend a liver biopsy. A small sample of liver tissue is extracted with a needle and examined under a
microscope. This provides the most accurate assessment of inflammation and scarring.
Get Your Health Assessed
Reversing the Trend: Effective Treatment and Management Strategies
The most powerful message about fatty liver disease is that it is largely reversible, especially in the early stages. There is
no specific medication approved solely for NAFLD; instead, treatment focuses on addressing the underlying causes.
- Lifestyle Modifications: This is the most critical aspect of how to reverse fatty liver naturally.
- Designing a Liver-Friendly Diet: Focus on whole foods: fruits, vegetables, whole grains, lean proteins (like fish and
chicken), and healthy fats (like those in nuts and olive oil). Strictly limit added sugars, refined carbs (white bread,
pasta), saturated fats, and processed foods. The Mediterranean diet is often recommended. - The Power of Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity exercise (like brisk walking,
cycling, or swimming) per week. Exercise helps reduce liver fat independently of weight loss by improving insulin
sensitivity. - Managing Underlying Conditions: Working with your doctor to effectively manage diabetes, high cholesterol, and high blood pressure is essential. This may involve medication and regular monitoring.
Prevention is Key: How to Protect Your Liver Health
Preventing fatty liver disease revolves around maintaining a healthy metabolic profile. Here’s how to prevent:
- Maintain a Healthy Weight: If you are overweight, losing even 5-10% of your body weight can make a significant difference.
- Eat a Balanced Diet: Make plant-based foods the star of your plate.
- Exercise Regularly: Incorporate both cardio and strength training.
- Limit Alcohol: If you drink, do so in moderation.
- Use Medications Wisely: Take all medications as prescribed and discuss potential side effects with your doctor.
Conclusion
Fatty liver disease may be common, but it is not a fate you have to accept. By understanding the risk factors and
recognising the power of proactive lifestyle choices, you can take control of your liver health. The journey to reversal
begins with manageable steps: swapping sugary drinks for water, adding a daily walk, and filling your plate with colorful, nutrient-rich foods. Remember, your liver is a remarkably resilient organ. With consistent care and the guidance of healthcare professionals, you can reduce liver fat, lower inflammation, and significantly decrease your risk of long-term complications. Start your journey to a healthier liver today—it’s one of the most important investments you can make in your overall well-being.
Consult a Specialist for the best advice
Consult a Specialist for the best advice

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. Srinivasa Reddy
Hepatologist
12 Years • MBBS, MD (General Medicine), DM (Hepatology),ASGE
Hyderabad
Myra Liver & Gastro Care, Hyderabad

Dr. Rajeev Shandil
Gastroenterology/gi Medicine Specialist
15 Years • MBBS, DNB (Internal Medicine), DNB (Gastroenterology)
Delhi
Apollo Hospitals Indraprastha, Delhi
(150+ Patients)
Consult a Specialist for the best advice

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. Srinivasa Reddy
Hepatologist
12 Years • MBBS, MD (General Medicine), DM (Hepatology),ASGE
Hyderabad
Myra Liver & Gastro Care, Hyderabad

Dr. Rajeev Shandil
Gastroenterology/gi Medicine Specialist
15 Years • MBBS, DNB (Internal Medicine), DNB (Gastroenterology)
Delhi
Apollo Hospitals Indraprastha, Delhi
(150+ Patients)
More articles from Fatty Liver
Frequently Asked Questions
1. Can you die from fatty liver disease?
While simple fatty liver is often not life-threatening, its advanced form, NASH, can progress to cirrhosis and liver failure, which are serious conditions. However, early-stage disease is reversible, and progression can be halted with intervention.
2. What is the best diet for fatty liver disease?
A liver-friendly diet emphasises whole foods. Think of the Mediterranean diet: plenty of vegetables, fruits, whole grains, fish, and olive oil. Avoid sugary beverages, processed snacks, and excessive red meat.
3. What is the difference between NAFLD and NASH?
NAFLD is an umbrella term for fat in the liver not caused by alcohol. NASH is a specific, more severe subtype of NAFLD that includes both fat and inflammation, which can lead to scarring.
4. Is fatty liver disease reversible?
Yes, in its early stages, fatty liver disease is often completely reversible through sustained lifestyle changes, particularly weight loss and exercise. This is the most hopeful aspect of the condition.
5. How long does it take to reverse a fatty liver?
There's no fixed timeline, as it depends on the individual and the severity. However, studies show that losing 5-10% of body weight over 6-12 months can significantly reduce liver fat and inflammation.

.webp)


 (1).webp)