Lung Fibrosis Guide: Symptoms, Tests, Treatment
Discover the essential facts about lung fibrosis—what it is, early signs, and how it is diagnosed and treated. Understand available medications, oxygen therapy, lifestyle strategies, and travel/work considerations.

Written by Dr. M L Ezhilarasan
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026

Introduction
Breathing is something we rarely think about — until it becomes difficult. Lung fibrosis is a condition where the lung tissue gradually scars and stiffens, making each breath require more effort. In the early stages, symptoms can be subtle: a mild dry cough, breathlessness while climbing stairs, or tiring faster than expected. Over time, as more lung tissue becomes scarred, the lungs struggle to pass oxygen into the bloodstream efficiently. This can affect everyday activities, work, social life and emotional wellbeing.
Because the scarring cannot be reversed, early recognition and treatment are essential to slow progression. Modern antifibrotic medicines, oxygen therapy and pulmonary rehabilitation help people remain active and preserve independence. Understanding symptoms, diagnosis and available care empowers individuals and families to make informed decisions. If symptoms persist or worsen, you can consult a respiratory specialist online with Apollo 24|7 for timely assessment and guidance.
Consult a Top Pulmonologist for Personalised Advice
What Is Lung Fibrosis?
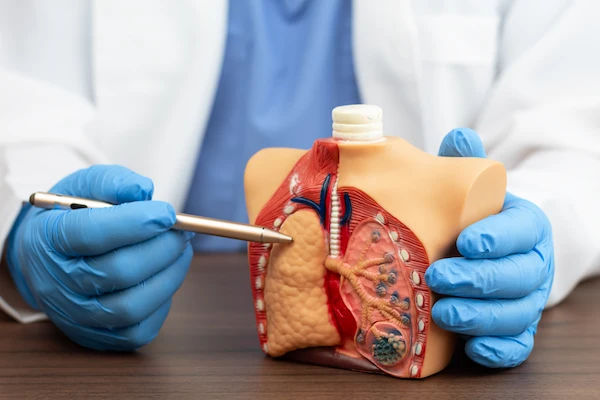
Lung fibrosis describes scarring in the lung’s interstitium—the thin, lace-like tissue around air sacs (alveoli). Healthy alveoli stretch like balloons, allowing oxygen to move into blood and carbon dioxide out, but scar tissue stiffens the walls, meaning each breath takes more effort and less oxygen is transferred.
Pulmonary Fibrosis vs. Interstitial Lung Disease (ILD)
Pulmonary fibrosis falls under the umbrella of interstitial lung disease (ILD). Not all ILDs are fibrotic; some are inflammatory and reversible if caught early. Others evolve into fibrosis over time. Knowing where your condition sits on the inflammation-to-fibrosis spectrum guides treatment choices.
How Scarring Disrupts Oxygen Exchange
Think of fibrosis as replacing springy bubble wrap with dense foam. The foam won’t stretch and gas can’t slip through as easily—that’s why people with lung fibrosis often develop exertional breathlessness and lower oxygen with activity.
Idiopathic Pulmonary Fibrosis (IPF) vs. Secondary Causes
• IPF: A distinct diagnosis with no known cause, usually in adults over 60, often showing a “usual interstitial pneumonia” pattern on high-resolution CT (HRCT).
• Secondary pulmonary fibrosis: Triggered by autoimmune disease, occupational exposures (silica, asbestos, wood dust), certain medications, chronic hypersensitivity pneumonitis, prior infections or genetic predisposition.
Symptoms and When to See a Doctor
Early identification improves outcomes and quality of life.
Early Signs You Might Miss
• Breathlessness on exertion (e.g., climbing stairs, carrying groceries)
• Persistent dry cough
• Fatigue and decreased exercise tolerance
• Fine “Velcro-like” crackles heard on a stethoscope
• Unintended weight loss or diminished appetite (in later stages)
Many people attribute early breathlessness to ageing or deconditioning; this can delay diagnosis.
Red Flags Requiring Urgent Care
• Rapid worsening of breathlessness over days (“acute exacerbation”)
• Blue lips or fingertips, or resting oxygen saturation persistently under about 88–90%
• Chest pain, fever with cough, or coughing up blood
• Severe dizziness, fainting or inability to keep up with normal activities
If your symptoms persist beyond two weeks or your condition does not improve with home management, consult a doctor online with Apollo 24|7 for further evaluation.
How Symptoms Progress Over Time
Symptoms may progress gradually or in step-wise drops. A key concept is “breathlessness at a lower workload”: tasks that were fine last month now require pauses. Tracking stairs, walking distance, and recovery time is helpful.
Causes and Risk Factors
Knowing the triggers can help prevent or manage disease progression.
Environmental and Occupational Exposures
Chronic inhalation of silica, asbestos, coal/metal dusts, wood dust, farm dust or chemical fumes can injure lung tissue and trigger scarring. Chronic hypersensitivity pneumonitis (from bird proteins or mould) is another recognised cause.
Autoimmune and Connective Tissue-Related Fibrosis
Autoimmune conditions such as rheumatoid arthritis, systemic sclerosis, polymyositis/dermatomyositis and Sjögren’s syndrome can cause ILD. These may respond to immunomodulating therapy and often have a different prognosis than IPF.
Medications, Infections and Genetic Factors
Some drugs (amiodarone, bleomycin, nitrofurantoin) and prior radiation exposure can lead to fibrosis. Recurrent aspiration from uncontrolled acid reflux and certain viral infections are additional contributors. Genetic variants affecting telomerase and surfactant proteins increase risk, especially when the disease appears early or in family clusters.
Who Is Most at Risk?
• Age over 60, male gender and a history of smoking (for IPF)
• Long-term exposure to harmful dusts or fumes
• Autoimmune disease
• Family history of pulmonary fibrosis
Recognising risk factors helps prompt earlier testing.
How Lung Fibrosis Is Diagnosed
Diagnosis uses a combination of history, examination, lung function, imaging and sometimes tissue sampling.
Pulmonary Function Tests and 6-Minute Walk
Pulmonary function tests typically show a “restrictive” pattern (reduced forced vital capacity, FVC) and impaired gas transfer (low DLCO). A six-minute walk test (6MWT) tracks how far you can walk and whether oxygen falls during exercise. Some programmes use home spirometry to monitor trends.
High-Resolution CT Chest and the UIP Pattern
High-resolution CT (HRCT) is essential. A “usual interstitial pneumonia” (UIP) pattern—basal/subpleural reticulation, honeycombing and traction bronchiectasis—supports the diagnosis of IPF when no other cause is identified. Other patterns (NSIP, etc.) suggest different diagnoses or treatments.
Blood Tests and Biopsy Considerations
Blood tests should screen for autoimmune causes (ANA, rheumatoid factor, anti-CCP). When results are unclear and treatment would change, bronchoscopy or surgical lung biopsy may be considered—but not everyone needs this. You may arrange home sample collection via Apollo 24|7 for routine blood work.
Multidisciplinary Discussion (MDD)
An MDD of a pulmonologist, thoracic radiologist and pathologist integrates findings into a clear diagnosis and treatment plan—recognised as best practice in ILD centres.
Treatments That Slow Fibrosis
While no cure exists yet, several treatments slow progression and improve quality of life.
Antifibrotic Drugs: Nintedanib and Pirfenidone
Two antifibrotics (nintedanib, pirfenidone) can slow decline of lung function in IPF by about 50% on average. Nintedanib is also used in other progressive fibrosing ILDs. Start early for greatest benefit.
Side-Effect Management and Monitoring
• Nintedanib: Diarrhoea is common; dose adjustment, diet and antidiarrhoeals help. Monitor liver enzymes.
• Pirfenidone: Nausea and photosensitivity rash are typical—take with food and use sun protection.
Patients must maintain updated medication lists and review potential interactions.
Managing Contributing Conditions
• Treat acid reflux to reduce micro-aspiration
• Screen for and manage sleep apnoea to prevent overnight oxygen dips
• Manage chronic cough with humidified air, lozenges and, in some cases, neuromodulators
Small improvements in these areas can significantly improve daily function.
Supportive Care That Improves Daily Life
Good supportive care ensures you do more with the breaths you have.
Oxygen Therapy: When and How
Oxygen is prescribed when resting or exertional saturation is low (often ≤88-89%). It doesn’t cure fibrosis but reduces heart and brain strain, improves exercise tolerance and quality of life. Use portable units, plan backup power and follow your oxygen plan.
Pulmonary Rehabilitation and Breathing Techniques
Pulmonary rehab combines exercise training, education and breathing strategies to improve walking distance and confidence. Typical gains are 30-50 m on the 6MWT. Techniques include pursed-lip breathing, interval pacing and upper-body conditioning.
Nutrition, Vaccination and Energy Conservation
• Vaccinate: influenza, COVID-19, pneumococcal
• Nutrition: aim for adequate protein in small, frequent meals to avoid breathlessness post-meal
• Energy conservation: sit to complete tasks, avoid repeated trips, use rolling carts
Good nutrition and activity pacing can reduce symptom spikes.
Complications, Flares and Advanced Options
Being prepared for potential complications is key to long-term management.
Acute Exacerbations
An acute exacerbation of IPF is a sudden worsening in days to weeks with new lung infiltrates. It carries high short-term risk; early recognition and hospital treatment matter. Seek urgent care if breathlessness escalates or oxygen needs suddenly rise.
Pulmonary Hypertension in ILD
Scarring can raise pressure in lung vessels (pulmonary hypertension–ILD), worsening breathlessness and risking right-heart strain. Signs include disproportionate dyspnoea, reduced DLCO and leg swelling. Echocardiography screens; confirmed by right-heart catheterisation. Management combines oxygen, rehab and selected medications.
Lung Transplant and Clinical Trials
For advanced disease, lung transplant may extend life; early referral helps. Clinical trials are testing new antifibrotic and anti-inflammatory therapies—ask your clinician. Advance-care planning allows for your values to guide treatment decisions.
Living Well With Lung Fibrosis
Life adaptation helps you live better, not just longer.
Exercise, Pacing and Mental Health
• Exercise: aim for regular moderate activity tailored to your ability; even chair-based activity helps
• Pacing: break tasks into smaller parts, rest before being exhausted, coordinate movement with breathing
• Mental health: anxiety and low mood are common. Counselling, mindfulness and peer support help. Caregivers also need support.
Air Quality, Travel and Work Accommodations
• Air quality: check local AQI; in high-pollution days, use N95/FFP2 masks; run HEPA filters at home
• Travel: consult clinician before flying; some need in-flight oxygen; plan rest, airport support, carry device documentation
• Work: ask for reduced dust exposure, flexible schedule, remote options
Caregiver Support and Advance Planning
• Caregivers help with symptom tracking, coordinating appointments and managing oxygen/medications
• Early discussion of care preferences reduces stress for everyone
Conclusion
Lung fibrosis changes how your lungs move air and absorb oxygen, but it does not remove your ability to act. Understanding what’s happening inside—scarring in the interstitium—helps you recognise early signs, prompt investigations, and start proven therapies sooner. Antifibrotic medications, oxygen therapy, rehabilitation and lifestyle changes all combine to improve quality and length of life.
If your breathlessness or cough has persisted beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation; if your condition does not improve after these steps, book a physical visit with Apollo 24|7 or arrange home blood test collection. Keep the long view: discuss transplant and trial options early, make plans aligned with your priorities, and track your progress with your clinical team. With the right mix of medical treatment, thoughtful habits and support, many people with lung fibrosis maintain independence, continue doing what matters and face the future with clarity.
Consult a Top Pulmonologist for Personalised Advice
Consult a Top Pulmonologist for Personalised Advice

Dr Vishwa Vijeth K.
Pulmonology Respiratory Medicine Specialist
8 Years • MBBS, MD ( Respiratory Medicine)
Bangalore
Apollo Clinic Bellandur, Bangalore

Dr Rakesh Bilagi
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS MD PULMONOLOGIST
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
Dr. Preeti Kathail
General Physician/ Internal Medicine Specialist
17 Years • MBBS, PGDHHM
Bangalore
Apollo Clinic Bellandur, Bangalore

Santoshkumar P Hammigi
Pulmonology Respiratory Medicine Specialist
4 Years • MBBS,MD, (Respiratory Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
(25+ Patients)

Dr. Krishna Ramanathan
Ent Specialist
10 Years • MBBS DNB
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
Consult a Top Pulmonologist for Personalised Advice

Dr Vishwa Vijeth K.
Pulmonology Respiratory Medicine Specialist
8 Years • MBBS, MD ( Respiratory Medicine)
Bangalore
Apollo Clinic Bellandur, Bangalore

Dr Rakesh Bilagi
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS MD PULMONOLOGIST
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
Dr. Preeti Kathail
General Physician/ Internal Medicine Specialist
17 Years • MBBS, PGDHHM
Bangalore
Apollo Clinic Bellandur, Bangalore

Santoshkumar P Hammigi
Pulmonology Respiratory Medicine Specialist
4 Years • MBBS,MD, (Respiratory Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
(25+ Patients)

Dr. Krishna Ramanathan
Ent Specialist
10 Years • MBBS DNB
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
More articles from Fibrosis Of Lung
Frequently Asked Questions
1) Is lung fibrosis the same as COPD or asthma?
.No. COPD and asthma primarily involve airway obstruction; lung fibrosis scars the lung tissue around air sacs (interstitium), making the lungs stiff and reducing gas transfer.
2) Can lung fibrosis be cured?
Currently, there is no cure. However, antifibrotic drugs like nintedanib and pirfenidone slow progression. Supportive therapies (oxygen, rehabilitation) improve daily life.
3) What are the early signs of pulmonary fibrosis?
Common early signs include breathlessness on exertion and a persistent dry cough. If symptoms last more than two weeks, consult a doctor online with Apollo 24|7 for evaluation.
4) How is lung fibrosis diagnosed?
A.Diagnosis uses pulmonary function tests (FVC and DLCO), high-resolution CT scan, and sometimes biopsy. A team of specialists discusses the findings to reach a diagnosis.
5) Who should consider a lung transplant or join clinical trials?
Those with advanced disease, rapidly declining lung function or high oxygen needs should be referred for assessment at a transplant centre early. Clinical trials may be available through specialised centres.