Guide to Podiatry/foot Care Tips
Know about foot care, why it's important, most common issues, who is at risk, 60 60-second foot scan, preventing and managing foot care problems and more.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
Your feet carry you through roughly 8,000–10,000 steps a day—and yet they’re often the most neglected part of a self-care routine. Good foot care isn’t complicated, but it does take a few consistent habits: the right hygiene, properly fitting footwear, and quick responses to small issues before they turn into big problems. Whether you’re dealing with heel pain, athlete’s foot, or simply want to avoid blisters and toenail troubles, a little knowledge goes a long way.
In this guide, you’ll learn evidence-informed podiatry/foot care basics you can use right away: a daily routine that takes minutes, how to choose shoes and insoles that actually fit, prevention strategies for common conditions, and special tips for people with diabetes, athletes, kids, and older adults. If you’ve ever wondered whether orthotics are worth it, how to trim nails to avoid ingrown toenails, or which socks to buy to prevent athlete’s foot, this guide has you covered.
Why Foot Health Matters
The foot health includes:
Your feet by the numbers: anatomy and daily load
Each foot contains 26 bones, 33 joints, and more than 100 muscles, tendons, and ligaments. Together, your feet absorb
and return force with every step—multiplying your body weight several times over when you run or climb stairs. That
workload makes your feet uniquely vulnerable to overuse injuries and skin problems, especially if shoes don’t fit or you
increase activity too quickly. Good podiatry/foot care helps keep that complex system working smoothly by protecting
skin integrity, optimising load through proper footwear, and catching problems early.
Consult a Top General Practitioner for Personalised Advice
The most common foot issues and who’s at risk
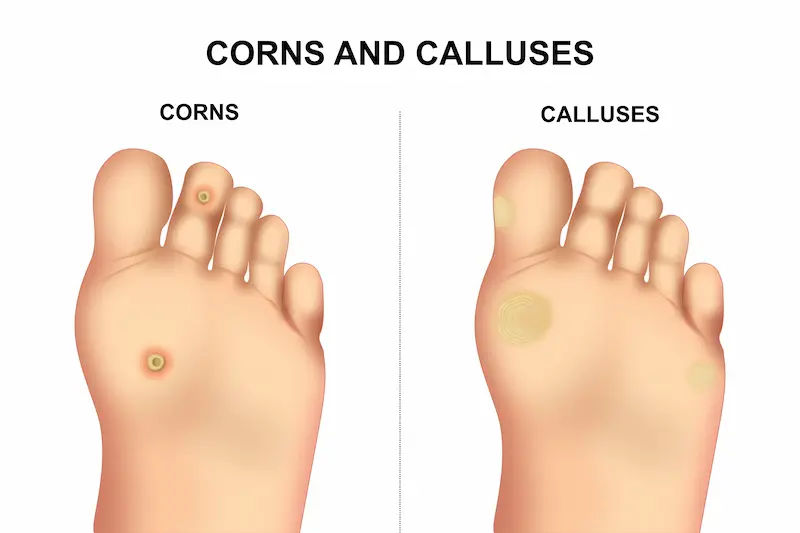
Common problems include athlete’s foot (fungal infection), plantar fasciitis (heel pain), bunions, corns and calluses,
ingrown toenails, cracked heels, and nail fungus. Risks rise with diabetes, high activity levels, prolonged standing, poor-
fitting shoes, obesity, and ageing. Evidence-based sources such as the APMA, AAD, and Cleveland Clinic highlight
prevention through hygiene, footwear, and early treatment, especially for people who notice persistent pain, swelling, or
changes in skin/nails.
How podiatry/foot care prevents bigger problems
Preventive routines washing and drying thoroughly, moisturising heels, trimming nails straight across, wearing
moisture-wicking socks, and choosing properly fitted shoes, reduce infection and injury risk. Early treatment of blisters,
calluses, or nail problems can prevent cellulitis or chronic pain. For people with diabetes, daily checks and prompt care
reduce the risk of ulcers and amputation. If symptoms persist beyond two weeks, consult a doctor online with Apollo24
|7 for further evaluation.
A Daily Foot Care Routine You’ll Actually Keep
This includes:
Hygiene fundamentals: wash, dry, moisturise, inspect
- Wash daily with warm water and mild soap; rinse thoroughly.
- Dry carefully—especially between toes—to prevent fungal overgrowth.
- Moisturise heels and soles (not between toes) to prevent cracks that can invite infection.
- Inspect for redness, swelling, blisters, cracks, or nail changes; catching problems early is a cornerstone of podiatry/foot
care [2][6]. Long-tail keyword: foot hygiene routine for athletes.
Nail care essentials: trim right, avoid ingrown toenails
- Trim nails straight across, not curved; don’t cut too short.
- Use clean clippers; file sharp edges.
- If a nail becomes ingrown, avoid digging; consider a warm soak and see a podiatrist if painful or infected. For recurring
issues, professional care is safer than aggressive home techniques.
Socks and materials: moisture-wicking vs cotton
Socks made of synthetic blends or merino wool wick moisture better than cotton, reducing friction and fungal risk.
Seamless or cushioned socks help prevent blisters if you walk or run a lot. Change socks after workouts; rotating pairs
and airing shoes reduces humidity—a key prevention step for athlete’s foot
The 60-second “foot scan” habit
Once daily, glance at soles, sides, and between toes; check nails and heels; wiggle toes; note any tenderness. Consider
taking a quick smartphone photo if you spot swelling or a new lesion helpful for tracking changes. People with diabetes
should do this every day and seek prompt care if they see redness, drainage, warmth, or a wound.
Footwear, Insoles, and Orthotics: What Really Matters
This includes:
Shoe fit and features that protect your feet
- Fit: Aim for a thumb’s width of space in front of your longest toe. Feet swell during the day; shop in the afternoon.
Width matters—don’t “size up” to get more width; choose the correct width instead. - Features: Look for a supportive heel counter, adequate arch contour, and a flexible forefoot that bends where your toes
bend. A wide toe box reduces pressure on bunions and hammertoes. - Purpose: Match the shoe to your activity (running, walking, hiking, or work safety). Replace shoes every 500–800 km of
running or when the tread is worn. Long-tail keyword: wide toe box shoes benefits. Insights from podiatry/foot care
resources emphasise structure and fit over brand hype.
Insoles vs custom orthotics: who needs what
- Insoles: Off-the-shelf inserts can add cushioning, heel cupping, or mild arch support at low cost. Try them for general
comfort or mild plantar fasciitis. - Custom orthotics: Consider if you have chronic pain, significant biomechanical issues (e.g., severe flatfoot), or recurrent
overuse injuries—fitted by a podiatrist after assessment.
Lacing patterns and small tweaks with big payoffs
- Runner’s loop/heel lock: Reduces heel slippage.
- Skip-eyelet technique: Relieves pressure over the top of the foot.
- Asymmetric lacing: Offloads bunions or high insteps.
- These small adjustments can be a game-changer for comfort without buying new shoes.
Preventing and Managing Common Foot Problems
The prevention and management include:
Athlete’s foot and fungal nails: hygiene and treatment
Athlete’s foot thrives in warm, moist environments. Prevention hinges on dry feet, flip-flops in public showers, rotating
shoes, and moisture-wicking socks. For mild infections, over-the-counter topical antifungals (e.g., terbinafine,
clotrimazole) are effective; treat for 1–2 weeks after symptoms clear to prevent recurrence. Fungal nails may require
longer treatment; see a clinician if nails are thick, painful, or discoloured. If your condition does not improve after trying
these methods, book a physical visit to a doctor with Apollo24|7.
Plantar fasciitis and heel pain: load management and stretches
Heel pain often stems from plantar fasciitis irritation of the tissue connecting the heel to the toes. Evidence-based self-
care includes relative rest, ice massage, supportive shoes, cushioned insoles or heel cups, and calf and plantar fascia
stretches (e.g., towel stretch, wall calf stretch). Morning pain is common; a night splint can help by preventing overnight
tightening. Gradually returning to activity and addressing training errors (sudden mileage increases, hard surfaces) are
key. If pain lasts beyond two weeks despite self-care, consult a doctor online with Apollo24|7.
Ingrown toenails, bunions, corns, and calluses: what helps
- Ingrown toenails: Trim nails straight; avoid tight shoes. Soaking can ease discomfort; infection or severe pain needs
clinical care. Recurrent cases may benefit from partial nail procedures. - Bunions: Wide toe box shoes, toe spacers, and pads can reduce pain; orthotics may help alignment symptoms. Surgery is reserved for significant pain or deformity affecting function.
- Corns/calluses: Address friction/pressure with better-fitting shoes and pads; moisturise skin. Avoid bathroom “surgery”—see a clinician for safe debridement if painful.
Home remedies: what’s safe, what to skip
- Generally safe: Epsom salt soaks for soreness; urea-based creams for thick heels; silicone pads for friction areas.
- Skip: Bathroom razors on calluses, tight bandaging on infected ingrown nails, and prolonged barefoot walking on hard floors when in pain.
Diabetic Foot Care Essentials
The essentials include:
Daily checks, protective habits, and foot exams
People with diabetes have a higher risk of neuropathy, ulcers, and infections. A daily podiatry/foot care routine is non-
negotiable: wash and dry carefully, moisturise soles (not between toes), inspect with a mirror, and wear protective socks
and shoes even indoors if sensation is reduced. Get regular foot exams by a clinician; they’ll check sensation, pulses, and skin.
Identifying neuropathy and poor circulation
Watch for numbness, tingling, burning pain, temperature changes, or wounds that heal slowly. Pale, cool feet or calf
pain when walking may indicate circulation issues. Early identification leads to better outcomes.
When to call a doctor and which tests to consider
Call promptly for any blister, ulcer, redness, drainage, or ingrown nail. Keep blood sugar targets on track; if due, review
HbA1c or vitamin D with your clinician. Apollo24|7 offers convenient home collection for tests like HbA1c and vitamin D, which can support your broader care plan.
Strength, Mobility, and Recovery for Resilient Feet
This includes:
Stretches and strengthening: evidence-informed basics
- Daily calf stretch (knee straight and bent) 2–3 sets x 30 seconds.
- Plantar fascia stretch: Cross one leg, pull toes back, and massage the arch.
- Toe yoga: Lift big toe while keeping others down, then reverse—3 sets of 10 to improve intrinsic foot strength and
balance. - Short foot exercise: Gently draw the ball of the foot toward the heel without curling toes.
- These build capacity to handle daily loads and support arches—core elements of podiatry/foot care.
Recovery tools: ice, massage, footwear rotation
Ice massage (frozen water bottle) for 5–10 minutes after activity can reduce heel soreness. A lacrosse ball or foam roller
under the arch and calf releases tension. Rotating footwear day-to-day changes pressure patterns and allows shoes to
dry fully, reducing fungus risk.
Training errors that spark foot pain
Rapid mileage jumps, back-to-back hard workouts, new terrain, or old shoes are common culprits. Follow the 10% rule
for weekly increases, and add one variable at a time (distance, speed, or hills) to pinpoint what’s aggravating symptoms.
Special Situations: Kids, Athletes, and Older Adults
The special situations include:
Children’s foot development and shoe choices
Kids’ feet grow quickly; check size every 2–3 months in younger children. Shoes should be flexible at the forefoot with a
secure heel and enough toe room. Flat feet can be normal in toddlers; seek evaluation if pain, tripping, or asymmetry
occurs. Prioritise play-appropriate shoes that stay on securely (e.g., Velcro or laces over loose slip-ons). Long-tail keyword: kids’ foot development and shoe size tips.
Athletes and gym-goers: prevention at scale
- Hygiene: Flip-flops in locker rooms; change socks post-workout; rotate shoes.
- Load management: Gradual program progression; strength and mobility routine 2–3x/week.
- Anti-blister tactics: Lubricants or powders for hot spots; tape before long runs; choose socks with minimal seams. Long-
tail keyword: foot hygiene routine for athletes.
Ageing feet: balance, skin care, and fall prevention
With age, fat pads thin and joints stiffen, increasing pain and fall risk. Use supportive, slip-resistant shoes indoors.
Moisturise to prevent skin cracks; trim nails straight across; consider a podiatry visit for thick nails or calluses. Balance
exercises (e.g., single-leg stands near support) are simple but powerful. If you notice sudden swelling, colour change, or a wound, seek care promptly.
When to Seek Podiatry Care
Seek medical care when:
Red flags that need prompt assessment
- Spreading redness, warmth, or drainage
- Severe, persistent pain or sudden swelling
- A wound, ulcer, or blackened skin
- Numbness, new foot drop, or intense night pain
- Recurrent ingrown toenails or deformity worsening
If symptoms persist beyond two weeks, consult a doctor online with Apollo24|7 for further evaluation, or book an in-
person orthopaedic visit.
What a podiatry visit includes
Your clinician may review footwear, activity, and medical history; examine skin and nails; assess alignment, flexibility,
and gait; and recommend imaging if needed. You’ll leave with a tailored plan: footwear changes, exercises, orthotics, or procedures.
Conservative vs surgical care: timeline and expectations
Most issues improve with conservative care (2–12 weeks): load management, footwear changes, targeted exercises, and
medication when appropriate. Surgery is considered when pain, function, or deformity doesn’t improve with well-
executed conservative treatment—your clinician will outline risks and recovery timelines.
Conclusion
Your feet are remarkably strong, but they’re not indestructible. A consistent podiatry/foot care routine protects the skin barrier, keeps nails healthy, and helps you catch small problems before they escalate. Thoughtful footwear choices and smart training prevent many issues, while simple habits like moisture-wicking socks, rotating shoes, and a daily one-minute foot scan create a safer, healthier foundation for everything you do.
If you’re dealing with athlete’s foot, heel pain, or bothersome calluses, use the strategies in this guide to start improving today. For persistent or severe problems, or if you live with diabetes or circulation changes, don’t wait to get help. And if you’re due for blood work like HbA1c or vitamin D, Apollo24|7 offers convenient home collection to support your broader health plan.
Consult a Top General Practitioner for Personalised Advice
Consult a Top General Practitioner for Personalised Advice

Dr. Arif Ahmed
General Physician/ Internal Medicine Specialist
9 Years • MBBS, MD (Genl. Med.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Mainak Baksi
General Practitioner
13 Years • MBBS , MD (MPH)
Howrah
Mainak Baksi Clinic, Howrah
(50+ Patients)

Dr. Anamika Krishnan
General Practitioner
11 Years • MBBS, DNB (Paediatrics) ,Diploma in child Health
Bengaluru
UMC (United Medical Center), Bengaluru

Dr. Minakshi Dutta
General Practitioner
37 Years • MBBS
Bengaluru
Trini Healthcare Pvt Ltd, Bengaluru

Dr. S A Mallick
General Physician/ Internal Medicine Specialist
25 Years • MBBS , MD
Kolkata
Dr. S A Mallick's Chamber, Kolkata
(25+ Patients)
Consult a Top General Practitioner for Personalised Advice

Dr. Arif Ahmed
General Physician/ Internal Medicine Specialist
9 Years • MBBS, MD (Genl. Med.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Mainak Baksi
General Practitioner
13 Years • MBBS , MD (MPH)
Howrah
Mainak Baksi Clinic, Howrah
(50+ Patients)

Dr. Anamika Krishnan
General Practitioner
11 Years • MBBS, DNB (Paediatrics) ,Diploma in child Health
Bengaluru
UMC (United Medical Center), Bengaluru

Dr. Minakshi Dutta
General Practitioner
37 Years • MBBS
Bengaluru
Trini Healthcare Pvt Ltd, Bengaluru

Dr. S A Mallick
General Physician/ Internal Medicine Specialist
25 Years • MBBS , MD
Kolkata
Dr. S A Mallick's Chamber, Kolkata
(25+ Patients)
More articles from Foot Care
Frequently Asked Questions
1) How should I trim toenails to avoid ingrown nails?
Trim straight across and don’t cut too short. File sharp corners rather than rounding deeply. If the skin is red, swollen, or draining, see a clinician. Long-tail keyword: how to trim toenails to avoid ingrown nails.
2) What are the best socks to prevent athlete’s foot?
Choose moisture-wicking materials like merino wool or synthetic blends and change socks after workouts. Rotate shoes to let them dry fully. Long-tail keyword: athlete’s foot prevention in gym showers.
3) Do I need custom orthotics, or will off-the-shelf insoles work?
Many people do well with quality insoles for cushioning or mild support. Custom orthotics are most helpful for chronic pain, significant flatfoot, or recurring overuse injuries. Long-tail keyword: orthotics vs insoles difference.
4) Which plantar fasciitis stretches help most?
Daily calf stretches (knee straight and bent) and plantar fascia stretches (pulling toes back) are well-supported. Pair with supportive shoes and a gradual return to activity. Long-tail keyword: plantar fasciitis stretches that work.
5) When should I see a podiatrist for foot pain?
If pain lasts more than two weeks, or you notice redness, swelling, drainage, deformity, or numbness, seek care. If symptoms persist beyond two weeks, consult a doctor online with Apollo24|7.