Subdural Hematoma Causes, Symptoms, Treatment
Know about the subdural haematoma, causes, symptoms, treatment and diagnosis and more.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 22nd Aug, 2025
Subdural Hematoma: Causes, Symptoms, Treatment
Introduction
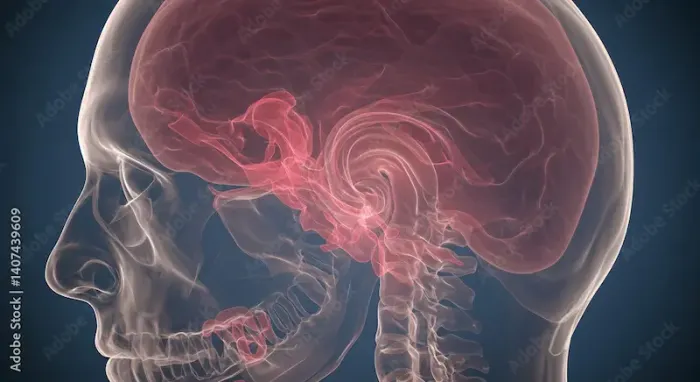
A subdural hematoma (SDH) is a serious medical condition where blood collects between the brain and its outermost protective layer (the dura mater). This buildup of blood can put pressure on the brain, leading to severe complications if not treated promptly.
Understanding the causes, symptoms, and treatment options can help you recognise warning signs early and seek timely medical care.
What Causes a Subdural Hematoma?
A subdural hematoma usually occurs due to a head injury, which can be mild or severe. Common causes include:
• Head Trauma – Falls, car accidents, sports injuries, or any impact to the head can tear blood vessels, leading to bleeding.
• Age-Related Risks – Older adults are more vulnerable because brain shrinkage (a natural part of ageing) stretches blood vessels, making them more likely to tear even from minor bumps.
• Blood Thinners – Medications like warfarin, aspirin, or clopidogrel increase bleeding risks.
• Alcohol Abuse – Chronic alcohol use can weaken blood vessels and increase fall risks.
• Medical Conditions – Conditions like liver disease or blood clotting disorders may contribute.
Consult a Neurologist for Personalised Advice
Symptoms to Watch For
Symptoms vary depending on how quickly the blood accumulates:
Acute Subdural Hematoma (develops rapidly, within hours or days)
• Severe headache
• Confusion or drowsiness
• Nausea and vomiting
• Slurred speech
• Weakness or numbness (often on one side of the body)
• Seizures
• Loss of consciousness
Chronic Subdural Hematoma (develops slowly, over weeks or months)
• Mild but persistent headaches
• Memory problems or confusion
• Personality changes (irritability, mood swings)
• Difficulty walking or balancing
• Gradual weakness in limbs
Note: In some cases, symptoms may appear mild at first but worsen over time. Immediate medical attention is crucial.
How Is It Diagnosed?
If a doctor suspects a subdural hematoma, they may recommend:
• CT Scan – The most common test to detect bleeding in the brain.
• MRI – Provides detailed images if the CT scan is unclear.
• Neurological Exam – Checks reflexes, coordination, and mental alertness.
Treatment Options
Treatment depends on the severity:
1. Observation (for small, slow-growing hematomas)
1. If symptoms are mild, doctors may monitor the condition with regular scans.
2. Medications (like steroids or anti-seizure drugs) may be prescribed.
2. Surgery (for larger or life-threatening hematomas)
1. Burr Hole Drainage – A small hole is drilled in the skull to drain the blood.
2. Craniotomy – A portion of the skull is temporarily removed to relieve pressure and remove the clot.
3. Recovery & Rehabilitation
• Rest and gradual return to normal activities.
• Physical or occupational therapy if movement or speech is affected.
• Avoid alcohol and blood-thinning medications unless approved by a doctor.
How Can You Prevent a Subdural Hematoma?
While not all head injuries can be avoided, you can reduce risks by:
1. Wearing Helmets – While biking, riding motorcycles, or playing contact sports.
2. Fall Prevention – Using handrails, non-slip mats, and proper lighting at home (especially for older adults).
• Managing Medications – If on blood thinners, regular check-ups with your doctor are essential.
• Limiting Alcohol reduces the risk of falls and vessel damage.
When to Seek Emergency Help?
If you or a loved one experiences:
• Sudden, severe headache
• Confusion or loss of consciousness
• Weakness or difficulty speaking
• Repeated vomiting
• Do not wait—rush to the nearest emergency room.
Final Thoughts
A subdural hematoma is a serious condition, but early detection and treatment can save lives. If you or someone around you has had a head injury, even a minor one, then stay alert for symptoms and seek medical help without delay.
Consult a Neurologist for Personalised Advice
Consult a Neurologist for Personalised Advice

Dr. Aditendraditya Singh Bhati
Neurosurgeon
18 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Neuroendoscopy
Delhi
Apollo Hospitals Indraprastha, Delhi
(100+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Sarthak Mehta
Neurologist
6 Years • MBBS , MS Mch ( Neuro )
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr Rajashekar Mummadi
Neurologist
3 Years • MBBS, DNB General Medicine, DRNB Neurology
Hyderabad
Dr Ram's Neuro Clinic, Hyderabad

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(125+ Patients)
Consult a Neurologist for Personalised Advice

Dr. Aditendraditya Singh Bhati
Neurosurgeon
18 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Neuroendoscopy
Delhi
Apollo Hospitals Indraprastha, Delhi
(100+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Sarthak Mehta
Neurologist
6 Years • MBBS , MS Mch ( Neuro )
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr Rajashekar Mummadi
Neurologist
3 Years • MBBS, DNB General Medicine, DRNB Neurology
Hyderabad
Dr Ram's Neuro Clinic, Hyderabad

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(125+ Patients)




.webp)