Endovascular Treatment Minimally Invasive Vascular Care
Explore endovascular treatment, a minimally invasive approach to vascular health. Learn how it works, benefits, and what to expect during recovery.

Introduction
Imagine fixing a complex problem within a delicate system without causing major disruption. That’s the core principle behind endovascular treatment, a revolutionary approach to healing conditions affecting your blood vessels. If you or a loved one is facing a vascular issue like a stroke, aneurysm, or blocked arteries in the legs, understanding this minimally invasive option is crucial. Unlike traditional open surgery that requires large incisions, endovascular procedures allow surgeons to repair problems from inside the blood vessels themselves. This article will serve as your comprehensive guide. We’ll break down what endovascular treatment is, how it compares to open surgery, the conditions it can treat, and what you can expect from the procedure itself. Our goal is to empower you with knowledge, so you can have informed conversations with your healthcare team about the best path forward for your vascular health.
Endovascular vs. Open Surgery: Why Choose a Minimally Invasive Path?
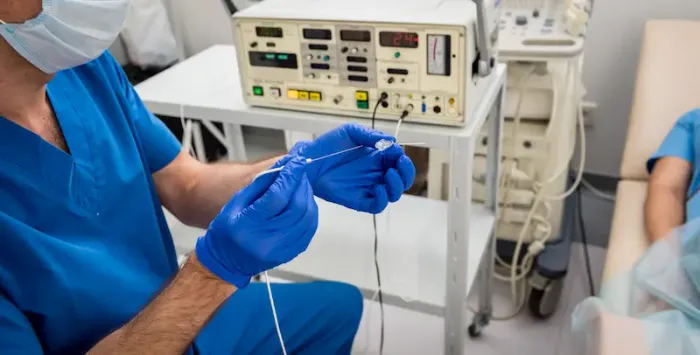
At its heart, endovascular treatment is a type of minimally invasive surgery. Instead of making a large cut to directly access the affected area, a specialist uses advanced imaging guidance to thread thin, flexible tubes called catheters through your blood vessels. These catheters, typically inserted through a small puncture in the groin or wrist, act as delivery systems for tiny instruments like stents, coils, or balloons.
Key Differences at a Glance
The fundamental difference lies in the approach:
• Open Surgery: Requires a significant incision to provide direct visual access to the organ or blood vessel. For example, open-heart surgery or open abdominal aortic aneurysm repair.
• Endovascular Surgery: Uses the body’s own vascular system as a highway to reach the problem area, requiring only a tiny entry point.
The Core Benefits of a Minimally Invasive Approach
This "inside-out" method translates into several significant patient benefits, which is why it's often the preferred option when medically appropriate.
• Smaller Incisions: This leads to less blood loss, reduced pain, and minimal scarring.
• Shorter Hospital Stays: Many endovascular procedures are outpatient or require only a 1-2 day hospital stay, compared to weeks for major open surgery.
• Faster Recovery: Patients can often return to their normal activities much more quickly.
• Lower Risk of Infection: Smaller wounds significantly reduce the chance of post-operative infections.
• Suitable for High-Risk Patients: Because it is less taxing on the body, endovascular treatment can be a life-saving option for older adults or those with other health conditions who might not tolerate open surgery well.
Consult a Vascular and Endovascular Surgeon for the best advice
Common Conditions Treated with Endovascular Techniques
Endovascular treatment is not a one-size-fits-all solution, but it has become the gold standard for managing a range of serious vascular conditions.
Ischaemic Stroke: A Race Against Time
An ischaemic stroke occurs when a blood clot blocks an artery supplying the brain. Endovascular thrombectomy is a highly effective procedure where a catheter is navigated to the brain to physically remove the clot. Studies show that this procedure can dramatically improve outcomes if performed within hours of stroke onset, often leading to remarkable recoveries. Recognising stroke symptoms (FAST: Face drooping, Arm weakness, Speech difficulty, Time to call emergency services) is critical for accessing this treatment quickly.
Brain Aneurysm: Preventing a Rupture
A brain aneurysm is a weak, bulging spot on a brain artery. If it ruptures, it causes a hemorrhagic stroke. Endovascular coiling is a common treatment where platinum coils are packed into the aneurysm through a catheter. These coils promote blood clotting, sealing off the aneurysm from the main artery and preventing a rupture. Another technique, flow diversion, uses a mesh stent to redirect blood flow away from the aneurysm.
Peripheral Artery Disease (PAD): Restoring Leg Circulation
PAD involves the narrowing of arteries in the legs, causing pain, numbness, and non-healing wounds. Endovascular treatment for PAD often involves angioplasty (inflating a tiny balloon to squish the plaque) and stent placement (inserting a mesh tube to hold the artery open). This restores blood flow, relieves symptoms, and can prevent amputation. If you experience persistent leg pain while walking, it’s important to consult a doctor. You can easily discuss these symptoms with a vascular specialist online through Apollo24|7 for an initial evaluation.
Other Vascular Conditions
This approach is also used for:
• Aortic Aneurysms: Repairing bulges in the body's main artery (aorta) with a stent-graft.
• Carotid Artery Disease: Opening blocked neck arteries that supply the brain to prevent stroke.
• Venous Thromboembolism: Treating blood clots in deep veins (DVT) or lungs (PE).
The Endovascular Procedure: A Step-by-Step Walkthrough
Knowing what to expect can alleviate anxiety. Here’s a general overview of the patient journey.
Before the Procedure: Preparation and Planning
Your medical team will conduct thorough assessments, which may include imaging tests like a CT angiogram or MRI. Apollo24|7 offers convenient home collection for pre-operative blood tests like a complete blood count (CBC) and coagulation profile. You’ll receive specific instructions about fasting and adjusting medications.
During the Procedure: The Journey from Within
You will be given sedation or general anaesthesia. The interventional radiologist or vascular surgeon will:
1. Access the Artery: Make a tiny puncture, usually in the femoral artery in the groin.
2. Insert the Guidewire and Catheter: Thread a guidewire into the artery, followed by a catheter over it.
3. Navigate with Live Imaging: Use real-time X-ray (fluoroscopy) to guide the catheter to the precise location of the problem.
4. Perform the Treatment: Deploy the necessary device (stent, coil, balloon, etc.).
5. Remove the Instruments and Close the Access Site: The catheter is removed, and pressure is applied to the small puncture site, which often requires no stitches.
After the Procedure: Recovery and Next Steps
You’ll spend a few hours in a recovery area to ensure the access site is stable. While recovery is faster than open surgery, you’ll still need to take it easy for a short period. Your doctor will provide specific guidelines on activity levels and follow-up care.
Get Your Health Assessed
Weighing the Options: Benefits and Potential Risks
Before opting for endovascular treatment, it’s important to understand both the potential benefits and the associated risks.
Significant Advantages of Endovascular Treatment
As discussed, the benefits are compelling: minimal scarring, reduced pain, shorter hospital stays, and a quicker return to normal life. For many, it offers a safe and effective alternative to the physical trauma of open surgery.
Understanding the Potential Complications
No procedure is without risk. Potential complications, though relatively rare, can include:
• Bleeding or infection at the puncture site.
• Damage to the blood vessel.
• Allergic reaction to the contrast dye.
• The small risk of the clot or blockage recurring.
Your doctor will discuss these risks in detail based on your specific health profile.
Who is a Candidate for Endovascular Treatment?
Not everyone is a suitable candidate. The decision depends on factors like the specific condition, its location and severity, the patient's overall health, and anatomy of the blood vessels. A multidisciplinary team of neurologists, vascular surgeons, and interventional radiologists will determine the best treatment plan for each individual.
The Future is Endovascular: Innovations on the Horizon
The field is rapidly evolving. Robotics are being integrated to enhance precision, and new bioactive stents that release medication to prevent re-narrowing are under development. These advancements promise even better outcomes and expanded applications for minimally invasive vascular surgery in the years to come.
Conclusion: Taking the Next Step for Your Vascular Health
Endovascular treatment represents a monumental leap forward in medical care, offering hope and healing with significantly less disruption to patients' lives. By understanding this procedure, you are better equipped to participate actively in your healthcare decisions. If you have concerns about symptoms like leg pain, chest discomfort, or a family history of aneurysms, do not hesitate to seek professional advice. Early diagnosis is key to accessing the full range of treatment options, including these advanced minimally invasive techniques. If you have questions about your vascular health, consulting a doctor online with Apollo24|7 is a convenient first step to determine if further investigation is needed.
Consult a Vascular and Endovascular Surgeon for the best advice
Consult a Vascular and Endovascular Surgeon for the best advice

Dr. Lal Daga
Cardiologist
20 Years • MBBS, DNB [MED], DNB [CARDIO], FESC [INT], MNAMS
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad

Dr. Jaisom Chopra
Vascular Surgeon
35 Years • MBBS, MS, FRCS
Delhi
Apollo Hospitals Indraprastha, Delhi
(50+ Patients)

Dr. Nikhila Pinjala
Vascular and Endovascular Surgeon
7 Years • MBBS, M.S(Gen),DNB (Vascular)
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(25+ Patients)
Dr Yashpal Singh
Vascular and Endovascular Surgeon
18 Years • MBBS, MS (Gen. Surgery), DNB ( Peripheral Vascular Surgery)
Lucknow
Apollomedics Super Speciality Hospital, Lucknow

Dr. Abhijit Das
Surgical Oncologist
10 Years • MBBS MS, MCh (Surgical Oncology), Fellowship in Thoracic Oncology (SNUK, Korea), Fellowship in Advance Esophageal Surgery (NCC, Japan)
Chennai
Apollo Proton Cancer Center, Chennai
Consult a Vascular and Endovascular Surgeon for the best advice

Dr. Lal Daga
Cardiologist
20 Years • MBBS, DNB [MED], DNB [CARDIO], FESC [INT], MNAMS
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad

Dr. Jaisom Chopra
Vascular Surgeon
35 Years • MBBS, MS, FRCS
Delhi
Apollo Hospitals Indraprastha, Delhi
(50+ Patients)

Dr. Nikhila Pinjala
Vascular and Endovascular Surgeon
7 Years • MBBS, M.S(Gen),DNB (Vascular)
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(25+ Patients)
Dr Yashpal Singh
Vascular and Endovascular Surgeon
18 Years • MBBS, MS (Gen. Surgery), DNB ( Peripheral Vascular Surgery)
Lucknow
Apollomedics Super Speciality Hospital, Lucknow

Dr. Abhijit Das
Surgical Oncologist
10 Years • MBBS MS, MCh (Surgical Oncology), Fellowship in Thoracic Oncology (SNUK, Korea), Fellowship in Advance Esophageal Surgery (NCC, Japan)
Chennai
Apollo Proton Cancer Center, Chennai
More articles from General Medical Consultation
Frequently Asked Questions
1. How long does an endovascular procedure typically take?
The duration varies widely based on complexity, ranging from 30 minutes for a simple angiogram to several hours for a complex aneurysm repair. Your doctor will give you a more specific time frame.
2. Is endovascular treatment considered major surgery?
While it is a significant medical procedure, it is categorised as 'minimally invasive surgery.' It is major in terms of its importance and the conditions it treats, but not in terms of the physical trauma associated with traditional open major surgery.
3. What is the recovery time after endovascular surgery?
Recovery is notably faster. Many patients return to light activities within a week, but it may take a few weeks to resume all normal activities, depending on the procedure and your overall health. Your doctor will provide a personalised timeline.
4. Are the results of endovascular treatment permanent?
Many treatments provide long-lasting results. However, some procedures, like angioplasty for PAD, may have a risk of the artery narrowing again (restenosis). Stents are designed to be permanent, and follow-up monitoring is essential to ensure long-term success.
5. What are the alternatives to endovascular treatment?
The primary alternative is often open surgery. In some cases, medication alone (such as blood thinners for clot-related issues) or lifestyle changes (for early-stage PAD) may be recommended. The best option depends entirely on your specific diagnosis.