Guide to Acute Encephalitis Syndrome Aes
A comprehensive guide to Acute Encephalitis Syndrome (AES), covering its causes, symptoms, diagnosis, treatment, and prevention. Learn how to protect yourself and your loved ones from this serious public health concern.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026
Introduction
Imagine a sudden, high fever in a child, followed by confusion, a severe headache, or even a seizure. This medical emergency could be Acute Encephalitis Syndrome (AES), a serious condition characterized by rapid onset inflammation of the brain. Often dubbed "brain fever," AES primarily affects children and young adults and is a major public health concern in many parts of the world, including East Asia and India. Its causes can be varied, from common viruses to environmental toxins, making it a complex syndrome to understand and manage. This guide will demystify AES, breaking down everything you need to know—from its primary causes and telltale symptoms to modern diagnostic methods, treatment options, and crucial prevention strategies. Our goal is to equip you with knowledge that could help in early recognition and timely medical intervention, potentially saving a life.
Consult a General Physician for the best advice
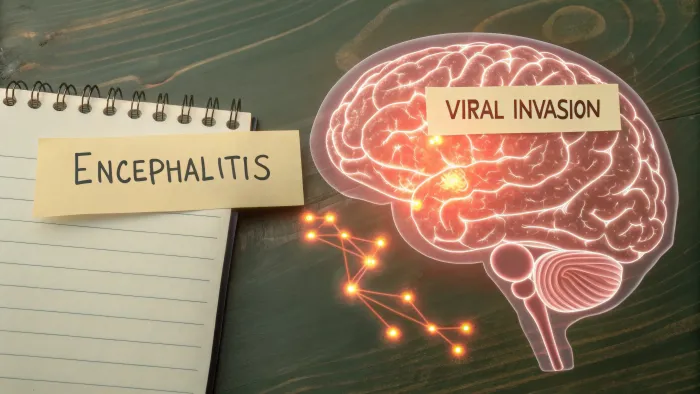
What is Acute Encephalitis Syndrome (AES)?
Acute Encephalitis Syndrome is not a single disease but a clinical umbrella term used by healthcare professionals. It refers to a group of similar neurological disorders characterized by an acute onset of fever and a change in mental status (including confusion, disorientation, coma, or inability to talk) and/or new onset seizures in a person of any age at any time of the year. The defining feature is inflammation of the brain parenchyma, which is the functional tissue of the brain.
The term "syndrome" is used because initially, the exact cause—whether it's a virus, bacteria, or something else—is often unknown. Physicians use this term to trigger a specific set of immediate diagnostic and treatment protocols while they work to identify the specific pathogen responsible.
AES vs. Encephalitis: Understanding the Difference
This is a key distinction. Encephalitis specifically means inflammation of the brain, usually due to a viral infection. Acute Encephalitis Syndrome (AES) is a broader term used for surveillance purposes. It includes all cases of encephalitis but also encompasses other conditions that present with similar symptoms, such as meningitis (inflammation of the brain's lining), cerebral malaria, and toxin induced brain disorders. In essence, all encephalitis cases can be classified as AES, but not all AES cases are solely encephalitis.
Primary Causes and Common Pathogens of AES
Pinpointing the cause of AES is critical for determining the correct course of treatment. The causes can be broadly categorized into infectious and noninfectious.
Viral Causes of Encephalitis
Viruses are the most common infectious cause of AES globally.
Japanese Encephalitis Virus (JEV)
This is a flavivirus spread through the bite of infected Culex mosquitoes. It is the leading cause of vaccine preventable AES in Asia, including India, and is particularly prevalent in rural and agricultural areas where rice farming and pig rearing create a breeding ground for mosquitoes.
Herpes Simplex Virus (HSV)
HSV1 (the virus that causes cold sores) is the most common cause of severe sporadic viral encephalitis in Western countries. It can occur in anyone, regardless of age or health, and requires rapid treatment with antiviral drugs to prevent severe brain damage.
Other Viral Culprits
Other viruses include:
Enteroviruses: Common in children, often spread through fecaloral route.
Nipah Virus: A zoonotic virus that has caused outbreaks with high mortality rates.
Dengue Virus: Can sometimes lead to neurological complications including encephalitis.
Chandipura Virus: Associated with outbreaks in India, affecting children.
NonViral and Unknown Causes
A significant proportion of AES cases, sometimes over 50% in certain outbreaks, have no identifiable cause. Other non viral factors include:
Bacteria: Like Mycobacterium tuberculosis or Rickettsia.
Parasites: Such as those causing cerebral malaria.
Fungi: Though less common.
Autoimmune Conditions: Where the body's immune system attacks the brain.
Toxins: For example, from consuming unripe lychee fruit on an empty stomach (linked to hypoglycemic encephalopathy in malnourished children).
Recognizing the Symptoms: Early and Severe Signs
Early recognition of encephalitis symptoms is vital. The initial signs often resemble the flu but can deteriorate rapidly.
Symptoms in Adults and Older Children
High fever
Severe headache that doesn't respond to painkillers
Confusion, agitation, or hallucinations
Drowsiness and lethargy
Sensitivity to light (photophobia)
Seizures
Stiff neck
Speech or hearing problems
Symptoms in Infants and Young Children
Bulging in the soft spots (fontanels) of an infant's skull
Nausea and vomiting
Body stiffness
Constant, inconsolable crying
Poor feeding or waking from sleep
If you or someone you know experiences a sudden high fever coupled with any of these neurological symptoms, it is a medical emergency. You should consult a doctor online with Apollo24|7 immediately for initial guidance or proceed to the nearest emergency room.
How is AES Diagnosed?
Diagnosing AES involves a combination of clinical assessment and laboratory tests to confirm brain inflammation and identify the cause.
Clinical Evaluation and History
A doctor will conduct a thorough physical and neurological exam, checking for reflexes, coordination, and sensory function. They will ask about recent travel, insect bites, sick contacts, and vaccination history.
Key Diagnostic Tests
Neuroimaging (MRI or CT Scan): An MRI is the preferred imaging test to look for inflammation and swelling in the brain.
Lumbar Puncture (Spinal Tap): This is crucial. Cerebrospinal fluid (CSF) is collected and analyzed for white blood cell count, protein, glucose, and presence of pathogens.
Electroencephalogram (EEG): This test detects abnormal brain electrical activity, which is common in encephalitis.
Blood and Serology Tests: Blood tests can identify antibodies against specific viruses or detect the virus itself through PCR testing. Apollo24|7 offers convenient home collection for tests like these to aid in the diagnostic process.
PCR Tests: Polymerase Chain Reaction (PCR) tests on CSF can directly detect the genetic material of viruses like HSV or JEV.
Treatment Options for Acute Encephalitis Syndrome
Treatment for AES has two main goals: to support the patient's bodily functions and to treat the underlying cause if known.
Immediate and Supportive Medical Care
This is the cornerstone of AES management protocol. Patients often require hospitalization, sometimes in an Intensive Care Unit (ICU). Supportive care includes:
Intravenous fluids to maintain hydration and correct electrolyte imbalances.
Medications to control fever and reduce brain swelling.
Antiseizure medications to prevent or stop seizures.
Assisted breathing with a ventilator if needed.
Antiviral and Specific Medications
If herpes simplex virus (HSV) is suspected, doctors will immediately start intravenous acyclovir, an antiviral drug. Early treatment significantly improves outcomes. For other specific causes, like bacterial infections or parasites, appropriate antibiotics or antiparasitic drugs are used. However, for many viruses like JE, there are no specific antiviral drugs, making supportive care and prevention even more critical.
Potential Complications and LongTerm Outlook
The long-term effects of encephalitis can be significant, especially if treatment is delayed. Complications include:
Persistent fatigue and weakness
Personality and behavioral changes
Memory problems and cognitive deficits
Speech and language impairments
Epilepsy
Physical disabilities
The outlook varies dramatically. Some people make a nearcomplete recovery, while others are left with permanent neurological damage. The prognosis depends on the cause, the severity of the inflammation, the patient's age, and how quickly treatment was initiated.
Prevention: How to Protect Yourself and Your Family
Prevention is undoubtedly the best strategy against AES, especially for vaccinepreventable forms.
Vaccination: The First Line of Defense
The Japanese encephalitis vaccine is highly effective and is included in the routine immunization schedule in many endemic countries. Ensuring your children receive this vaccine is the single most important step to prevent JErelated AES.
Mosquito Control and Bite Prevention
Since many AES causes are mosquito borne, preventing bites is crucial:
Use insect repellent containing DEET, picaridin, or oil of lemon eucalyptus.
Wear long sleeve shirts and long pants, especially during dusk and dawn when mosquitoes are most active.
Use mosquito nets and screens on windows and doors.
Eliminate standing water around your home where mosquitoes breed.
General Hygiene and Food Safety
Wash hands frequently to reduce the spread of enteroviruses.
Ensure food and water are from safe, clean sources.
Avoid consuming raw fruits that may have been contaminated or that have known associations with illness in malnourished individuals.
High Risk Groups and Geographical Areas
AES can affect anyone, but some groups are at higher risk:
Children and the Elderly: Their immune systems are often weaker.
People in Endemic Areas: Those living in or traveling to parts of Asia (like the Terai region of Nepal and states like Bihar, UP, and Assam in India) are at higher risk for JE.
Individuals with Compromised Immune Systems: Such as those with HIV/AIDS or people taking immunosuppressant drugs.
Conclusion
Acute Encephalitis Syndrome is a daunting and complex condition, but knowledge is power. Understanding its causes, recognizing its early warning signs, and knowing the importance of immediate medical care can dramatically alter the outcome for a patient. While research continues to uncover more about the unknown causes of AES, our best tools remain prevention through vaccination and public health measures, and vigilance in seeking care at the first sign of trouble. If you live in or are traveling to a high-risk area, talk to your doctor about preventive strategies, including vaccination.
If you suspect someone is showing symptoms of AES, do not wait—seek emergency medical care immediately or consult a doctor online with Apollo24|7 for urgent advice.
Consult a General Physician for the best advice
Consult a General Physician for the best advice

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Harshendra Jaiswal
General Physician/ Internal Medicine Specialist
12 Years • MBBS , MD (General medicine)
Kolkata
108 DHANA DHANVANTARI Clinic, Kolkata
(25+ Patients)
More articles from General Medical Consultation
Frequently Asked Questions
1. Can adults get Acute Encephalitis Syndrome, or is it only a children's disease?
While children are more commonly affected in large outbreaks (like JE), adults can absolutely contract AES. Herpes simplex encephalitis, for example, is equally common in adults. Age is a risk factor, but not an exclusive one.
2. Is Acute Encephalitis Syndrome contagious?
The syndrome itself is not contagious. However, some of the viruses that cause AES (like enteroviruses or HSV) can be spread from person to person. Mosquitoborne viruses like JE are not directly transmitted between people.
3. How long does it take to recover from encephalitis?
Recovery time varies widely. A mild case may resolve in a few weeks. Severe cases can require months of rehabilitation and may result in permanent disabilities. The recovery process is often slow and requires patience and extensive support.
4. What is the difference between encephalitis and meningitis?
This is a common point of confusion. Encephalitis is inflammation of the brain tissue itself. Meningitis is inflammation of the protective membranes (meninges) covering the brain and spinal cord. They can have similar symptoms (like headache and fever), but encephalitis more prominently features brain dysfunction (altered mental state, seizures). A condition called meningoencephalitis involves both.
5. Are there any specific foods to avoid for AES patients during recovery?
There's no specific 'AES diet,' but a brain healthy diet rich in antioxidants, omega3 fatty acids, and vitamins is beneficial. During recovery, a speech or occupational therapist might recommend texture modified foods if the patient has swallowing difficulties. Always follow the specific dietary advice of the treating neurologist or dietitian.