Guide to Hormonal Changes And Urological Health
Learn how hormonal changes across life stages affect urological health. Explore symptoms, causes, tests, treatments, and lifestyle strategies to support bladder, prostate, and kidney function.

Written by Dr. Mohammed Kamran
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 13th Jan, 2026

Introduction
Hormones quietly choreograph much of what happens in your body, including how often you urinate, whether you feel urgency, and how your bladder and prostate behave over time. When hormonal changes occur during puberty, pregnancy, perimenopause, menopause, or andropause, they can influence urological health in ways that are easy to overlook. This guide brings together what you need to know about hormonal changes and urological health, from common symptoms and conditions to testing, treatments, and prevention.
We explore how oestrogen, progesterone, testosterone, insulin, thyroid hormones, vasopressin, and others interact with the bladder, urethra, kidneys, and prostate. You will learn how life stages and endocrine conditions such as diabetes or hyperparathyroidism affect the urinary tract, as well as evidence-based steps you can take to feel better.
If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation. Hormonal changes are unavoidable; urological problems do not have to be.
How Do Hormones Shape the Urinary Tract?
Hormones act as the body’s messaging system, telling tissues when to grow, relax, contract, repair, or fight infection. The urinary tract, which includes the kidneys, ureters, bladder, urethra, and prostate, is packed with hormone receptors. Oestrogen and progesterone receptors are found in the bladder, urethra, vaginal mucosa, and pelvic floor, while androgen receptors are abundant in the prostate and lower urinary tract. Insulin, thyroid hormones, cortisol, vasopressin (antidiuretic hormone), and parathyroid hormone also influence fluid balance, smooth muscle tone, and stone formation.
Oestrogen supports healthy blood flow, collagen, and the microbiome of the vagina and distal urethra. When oestrogen declines, tissues become thinner and dryer, and urethral closure pressure may fall, raising the risk of urgency, frequency, stress incontinence, and recurrent urinary tract infections in midlife and beyond. Progesterone relaxes smooth muscle; during pregnancy, this helps the uterus expand but also slows ureteral flow and bladder emptying, increasing UTI risk.
In people with prostates, testosterone, converted locally to DHT, drives prostate growth over decades. Although benign prostatic hyperplasia (BPH) is not caused by high testosterone, DHT activation contributes to enlargement, which can pinch the urethra and cause lower urinary tract symptoms such as a weak stream, hesitancy, and nocturia.
Beyond sex steroids, insulin resistance is linked to inflammation and autonomic nerve dysfunction, mechanisms implicated in overactive bladder and nocturia. Vasopressin, which helps concentrate urine at night, often declines with age, leading to more nocturnal urine production and sleep disruption. Parathyroid hormone regulates calcium, and excess can cause hypercalcaemia and hypercalciuria, a key driver of kidney stones. Understanding your hormone landscape often clarifies urinary symptoms.
The endocrine–urogenital axis: a two-way street
Hormones affect urological tissues, while urinary symptoms influence stress hormones and sleep, creating feedback
loops. Inflammation and microbiome shifts mediate many hormone-driven changes.
Key hormones at a glance
Oestrogen, progesterone, testosterone/DHT, insulin, thyroid hormones, cortisol, vasopressin, and parathyroid hormone
all interact with receptors in the bladder, urethra, pelvic floor, prostate, and kidneys.
Consult Top Urologists
Life Stages and Hormonal Changes
Hormonal changes affect the urinary tract differently at each life stage.
Puberty
Rising sex steroids transform pelvic tissues. Sustained urinary issues are uncommon, though adolescents may experience transient frequency or urgency under stress as pelvic floor coordination continues to mature.
Pregnancy and Postpartum
Progesterone relaxes the ureters and bladder neck, while the enlarging uterus mechanically compresses the bladder. The
result is frequency, urgency, and increased UTI risk. Postpartum, temporary nerve and muscle stretch can lead to stress incontinence. Pelvic floor muscle training reduces postpartum urinary incontinence, both preventing and treating symptoms. If leakage persists beyond 6–12 weeks, consult a doctor online with Apollo 24|7.
Perimenopause and Menopause
Oestrogen decline alters urogenital tissues and the microbiome, contributing to urgency, frequency, dysuria, and recurrent UTIs. Vaginal oestrogen helps restore urethral and vaginal epithelium and is recommended to prevent recurrent UTIs in postmenopausal women with a history of infections. Overactive bladder also becomes more common, with behavioural therapy, pelvic floor muscle training, and medications often providing relief.
Ageing and Andropause
Testosterone levels gradually decline in many men with age. BPH prevalence rises steadily from midlife onward, as do lower urinary tract symptoms such as nocturia. The relationship between low testosterone and urinary symptoms is complex, and treatment of confirmed testosterone deficiency is individualised. Lifestyle changes to reduce metabolic
risk can ease LUTS across genders.
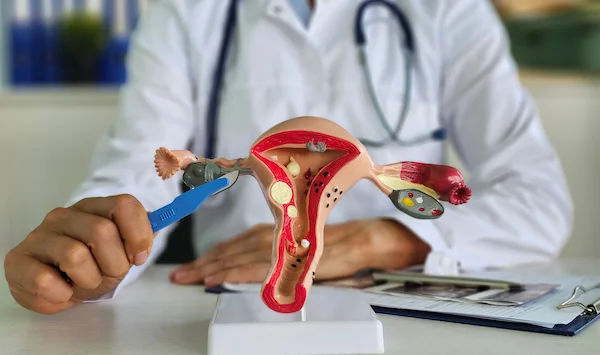
Women’s Urological Health Across Hormonal Milestones
Oestrogen is a major stabiliser of lower urinary tract health. When levels fall, the urethra loses some of its seal-and-support function, and the bladder may become more sensitive.
Oestrogen Decline and Recurrent UTIs
Guidelines recommend vaginal oestrogen for postmenopausal women with recurrent UTIs, as it reduces infection risk by improving local tissue integrity and microbiome balance. Unlike systemic HRT, vaginal oestrogen works locally with low systemic absorption. If you have two or more UTIs in six months or three or more in a year, ask your clinician about this option. Apollo 24|7 offers home collection for urine tests and cultures.
Overactive Bladder and Stress Incontinence
Overactive bladder affects 11–16% of adults, with urgency and frequency prominent around menopause. First-line therapy includes bladder training, limiting bladder irritants, and pelvic floor muscle training. For stress incontinence, pelvic floor exercises with a trained physiotherapist strengthen urethral support. In some cases, pessaries or minimally
invasive procedures are considered.
Vaginal Oestrogen and Pelvic Floor Therapy: A Synergistic Pair
Combining local oestrogen with pelvic floor training can amplify benefits. Estrogen enhances tissue responsiveness, while training adds muscular support. Scheduling pelvic floor exercises at the same time as applying vaginal oestrogen can improve adherence and outcomes.
Men’s Urological Health and Androgens
Androgens shape the prostate and lower urinary tract from puberty onwards. Over decades, DHT stimulates benign
proliferation of prostate tissue, narrowing the urethra.
BPH, LUTS, and DHT
BPH prevalence rises with age; by 60, many men have some prostate enlargement, and by 80, most do. Symptoms
include weak stream, hesitancy, incomplete emptying, frequency, and nocturia. Alpha-blockers relax the prostate and
bladder neck for rapid relief, while 5-alpha-reductase inhibitors shrink the prostate over months. Lifestyle strategies such as fluid timing and limiting caffeine and alcohol in the evening also help.
Testosterone Deficiency and Urinary Symptoms
Low testosterone can coexist with LUTS, but causation is nuanced. Guidelines advise confirming testosterone deficiency with two separate morning tests in symptomatic men before therapy. Testosterone therapy does not necessarily worsen LUTS and may improve metabolic parameters that contribute to urinary symptoms, but monitoring is essential.
PSA, Screening, and When to Treat
PSA helps risk-stratify for prostate cancer and reflects prostate volume. Decisions about BPH treatment consider
symptom burden, quality of life, prostate size, PSA, and complications. If symptoms persist or worsen, book a physical visit to a doctor with Apollo 24|7 for evaluation and tailored therapy.
Endocrine Disorders That Impact the Urinary System
The urinary tract reacts to sex steroids and the broader hormonal network.
Diabetes and Diabetic Bladder
Diabetes can injure autonomic nerves that control bladder sensation and emptying, producing frequency, urgency,
incontinence, or retention. Recurrent UTIs are more common, and wound healing may be slower. Glycaemic control, bladder training, scheduled voiding, and medications for overactive bladder can help.
Thyroid and Adrenal Disorders
Thyroid dysfunction can influence metabolism and fluid balance, affecting bladder behaviour. Severe hypothyroidism may contribute to urinary retention, while hyperthyroidism can be associated with frequency. Cortisol changes can affect fluid shifts, sleep, and nocturia.
Hyperparathyroidism and Kidney Stones
Primary hyperparathyroidism raises serum calcium and urinary calcium, increasing stone risk. Treating the parathyroid disorder reduces recurrence. Dietary review and 24-hour urine collection support prevention.
PCOS and Metabolic Links
PCOS features insulin resistance and hyperandrogenism. Metabolic inflammation and higher BMI can worsen overactive bladder and stress incontinence. Weight management and insulin-sensitising strategies improve urinary symptoms alongside overall cardiometabolic health.
Transgender and Gender-Diverse Care
Gender-affirming hormone therapy and surgeries intersect with urological health in unique ways.
Testosterone Therapy in Trans Men
Testosterone can cause vaginal atrophy and pH shifts, sometimes causing discomfort, spotting, or dysuria. Topical
vaginal oestrogen may restore tissue health and reduce urinary symptoms without interfering with masculinising
therapy.
Oestrogen/Antiandrogen in Trans Women
Trans women retain a prostate unless surgically removed. Feminising hormones may reduce prostate size and BPH risk,
but age-appropriate monitoring remains essential. PSA thresholds may need adjustment.
Post-Surgical Considerations
After vaginoplasty or phalloplasty, urinary stream changes, spraying, or transient retention can occur. Early follow-up
and gentle pelvic floor training improve voiding mechanics and reduce urgency.
Sleep, Stress, and Circadian Hormones
Nighttime urine production should fall due to vasopressin surges. Age or conditions that weaken these patterns cause nocturnal polyuria and nocturia. Elevated evening cortisol and stress can increase awakenings.
Nocturia and Vasopressin
Desmopressin can help select patients but requires sodium monitoring due to hyponatraemia risk. Simple changes
include finishing most fluids by early evening, elevating legs after dinner, and addressing sleep apnoea.
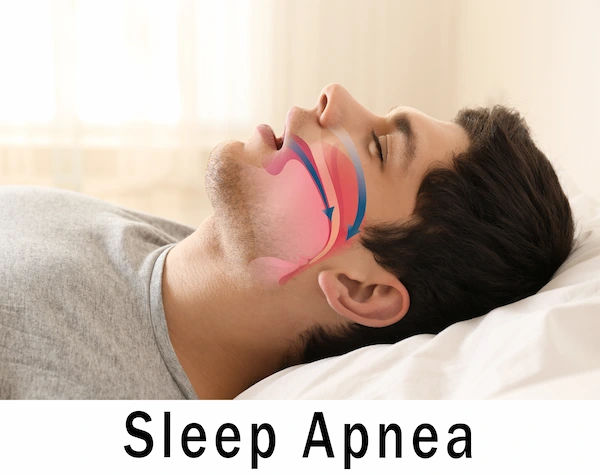
Cortisol, Sleep Apnoea, and Overactive Bladder
Obstructive sleep apnoea triggers natriuretic peptide release and nocturia; treating sleep apnoea often improves bladder stability. Stress-reduction techniques such as breathwork and short evening walks can ease urgency.
Practical Routines
Small, consistent changes in daily habits can significantly improve urinary comfort.
- Adopt a “front-loaded” hydration plan: 70% of fluids before mid-afternoon.
- Reduce caffeine after noon and alcohol in the evening.
- Add a 5-minute wind-down: elevate legs, slow breathing, and use the bathroom before bed.
Diagnosis: From Symptoms to Tests
A thorough evaluation connects symptoms to likely hormonal changes and rules out red flags.
What to Tell Your Clinician
Track frequency, urgency, leakage, nocturia, pain, haematuria, and triggers. Note life stage, medications, and endocrine
conditions such as diabetes or thyroid disorders.
Labs and Imaging
Common tests include urinalysis and culture, post-void residual, PSA, fasting glucose/HbA1c, electrolytes,
calcium/PTH, thyroid panel, and sex hormones when clinically indicated. Apollo 24|7 offers home collection for many
of these tests.
Uroflow, Urodynamics, and Imaging
Uroflowmetry and ultrasound assess stream and anatomy. Urodynamics characterises overactive bladder, stress
incontinence, and retention, especially before surgery. Pelvic or prostate exams can reveal tissue changes related to hormonal shifts.
If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7. Book a physical visit for pelvic or
prostate exam, imaging, or procedures.
Treatment Options: Hormonal and Non-Hormonal
Effective plans blend behaviour, pelvic floor care, and targeted medications.
Local Oestrogen and Systemic HRT
Vaginal oestrogen improves dryness, urgency, and recurrent UTIs in postmenopausal women. Systemic HRT is
individualised and not primarily used for bladder issues; discuss risks and benefits with your clinician.
Alpha-Blockers, 5-ARIs, Antimuscarinics, Beta-3 Agonists
Targeted medications provide relief for common urinary symptoms. Understanding how each works, their benefits, and
potential side effects helps you make informed decisions alongside your healthcare provider.
- BPH/LUTS: Alpha-blockers provide quick relief; 5-ARIs shrink the prostate over months.
- Overactive bladder: Antimuscarinics reduce urgency but may cause dry mouth and constipation; beta-3 agonists offer
similar benefits with fewer cognitive risks. - Refractory OAB: OnabotulinumtoxinA injections or tibial/sacral neuromodulation are options.
Testosterone Therapy: Who Benefits
Treat confirmed testosterone deficiency in symptomatic men, monitoring PSA and haematocrit. Lower urinary tract
symptoms are not an absolute contraindication.
Lifestyle and Pelvic Floor Training
Pelvic floor muscle training is foundational across stress incontinence and postpartum care. Weight loss and metabolic
improvements can reduce LUTS. Dietary adjustments help prevent recurrent stones.
Nutrition and Lifestyle for Hormone–Uro Health
Diet, weight management, and exercise influence both hormonal balance and urinary health. Simple adjustments can
prevent stones, reduce bladder irritation, and support long-term comfort.
Diet and Stones
For calcium oxalate stones, normalise dietary calcium to bind oxalate in the gut, reduce sodium and excessive animal
protein, and increase citrate from fruits and vegetables.
Weight, Insulin Resistance, and LUTS
Higher BMI and insulin resistance correlate with LUTS and overactive bladder. A 5–10% weight loss can improve
symptoms, reduce nocturia, and enhance continence.
Hydration Habits
Aim for pale yellow urine by mid-afternoon, then taper intake. Avoid frequent “just in case” voiding; train the bladder
with planned intervals. Pair daily behaviours with bladder-friendly habits for consistency.
Myths vs Facts
Misconceptions about hormones and urinary health are common. Separating fact from fiction empowers you to make
choices based on science rather than hearsay.
Common Misconceptions
Popular beliefs often misrepresent urinary health. Clarifying these misconceptions helps avoid ineffective or harmful
strategies.
- Drinking less water will cure overactive bladder. Underhydration concentrates urine and irritates the bladder.
- Testosterone therapy always worsens BPH. Evidence is mixed; monitoring is key.
- All oestrogen is the same. Vaginal oestrogen acts locally and is recommended for recurrent UTIs in postmenopausal
women.
Evidence-Backed Truths
Research and clinical guidelines reveal what truly works for managing urinary symptoms. Following evidence-based
advice can improve outcomes and quality of life.
- Pelvic floor muscle training works for stress incontinence and postpartum prevention.
- Beta-3 agonists are a good alternative to anticholinergics for overactive bladder in older adults.
- Treating sleep apnoea often reduces nocturia.
Conclusion
Hormones may be invisible, but their impact on urological health is substantial. Oestrogen maintains urethral integrity
and urinary microbiome balance, while testosterone and DHT shape the prostate. Metabolic hormones such as insulin and vasopressin link lifestyle and sleep to urinary comfort. The best outcomes come from combining smarter routines, such as fluid timing, pelvic floor training, and sleep optimisation, with targeted therapies, including vaginal oestrogen for recurrent UTIs, alpha-blockers or 5-ARIs for BPH, beta-3 agonists for overactive bladder, and, when appropriate, hormone therapy guided by careful testing and monitoring. Persistent or worsening symptoms deserve professional attention. Book a physical visit with Apollo 24|7 for tailored evaluation and treatment. With the right plan, hormonal changes need not dictate your urological well-being.
Consult Top Urologists
Consult Top Urologists

Dr. Dhruv B. Patel
Urologist
12 Years • MBBS, MS, DrNB (Urology - IKDRC, Ahmedabad)
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad
(25+ Patients)

Dr Anupam Sharma
Urologist
18 Years • MBBS, MS(Gen Surgery), DNB (Urology)
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr. Rohit Bhattar
Uro Oncologist
14 Years • MBBS, MS, MCh (Urology), Fellowship in Uro-oncology and Robotic Urology (United Kingdom)
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad
(100+ Patients)

Dr. Adittya K Sharma
Urologist
16 Years • MBBS MS MCH
Lucknow
Dr A K SHARMA, Lucknow
Dr. J Chaithanya
Urologist
6 Years • MBBS MS GENERAL SURGERY MCH UROLOGY
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
Consult Top Urologists

Dr. Dhruv B. Patel
Urologist
12 Years • MBBS, MS, DrNB (Urology - IKDRC, Ahmedabad)
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad
(25+ Patients)

Dr Anupam Sharma
Urologist
18 Years • MBBS, MS(Gen Surgery), DNB (Urology)
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr. Rohit Bhattar
Uro Oncologist
14 Years • MBBS, MS, MCh (Urology), Fellowship in Uro-oncology and Robotic Urology (United Kingdom)
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad
(100+ Patients)

Dr. Adittya K Sharma
Urologist
16 Years • MBBS MS MCH
Lucknow
Dr A K SHARMA, Lucknow
Dr. J Chaithanya
Urologist
6 Years • MBBS MS GENERAL SURGERY MCH UROLOGY
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
More articles from General Medical Consultation
Frequently Asked Questions
Q1. Do hormonal changes cause overactive bladder?
Hormonal changes can contribute to overactive bladder by altering bladder sensitivity and pelvic tissues, especially around menopause. Behavioural therapy plus medications such as a beta-3 agonist often help.
Q2. Can vaginal oestrogen prevent recurrent UTIs?
Yes. In postmenopausal women with recurrent UTIs, guideline panels recommend vaginal oestrogen to reduce infection risk by restoring healthy urogenital tissue and microbiome balance.
Q3. Does testosterone therapy worsen prostate enlargement?
Not necessarily. In appropriately selected men with confirmed low testosterone, therapy does not consistently worsen urinary tract symptoms. Monitoring PSA and symptoms is essential.
Q4. Why do I urinate more at night as I get older?
Ageing blunts nighttime vasopressin, increasing nocturnal urine production. Fluid timing, leg elevation, addressing sleep apnoea, and targeted therapies can reduce nocturia.
Q5. Which lab tests help when urinary symptoms change?
Urinalysis/culture, PSA, HbA1c, electrolytes, calcium/PTH, thyroid tests, and, when indicated, morning testosterone or estradiol/FSH. Apollo 24|7 offers home collection for many of these labs.