Piles vs Fistula: Symptoms, Causes, and Key Differences
Piles vs fistula explained: symptoms, causes, diagnosis, and treatments—plus easy tips to protect anal health and when to see a doctor.


Introduction
Anal health is an important part of overall well-being, yet many people feel unsure about what’s normal and what needs care. Two conditions that often get mixed up are piles (hemorrhoids) and anal fistula. Understanding piles vs fistula can help you spot the signs early, know what to do next, and feel more confident discussing symptoms with your healthcare provider. This guide uses clear, up-to-date information to explain symptoms, causes, diagnosis, and treatments—plus practical tips to protect your anal health.
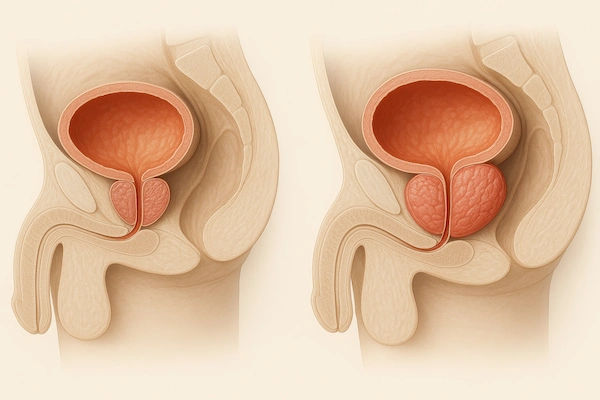
What are piles (hemorrhoids)?
Piles, also called hemorrhoids, are swollen veins in the lower rectum and anus. They’re similar to varicose veins and are very common. Hemorrhoids can be:
• Internal: inside the rectum. They usually aren’t painful but can bleed during a bowel movement. Some may prolapse (bulge) through the anus.
• External: under the skin around the anus. These can itch, hurt, or bleed. A clot can form (thrombosed external hemorrhoid), causing a sudden, very painful lump.
Common symptoms
• Bright red blood on toilet paper or in the bowl after a bowel movement
• Itching or irritation around the anus
• Discomfort or a feeling of fullness
• A tender lump near the anus (more typical with external hemorrhoids)
• Mucus and mild soiling if an internal hemorrhoid prolapses
What causes hemorrhoids?
• Anything that increases pressure in the lower rectum can contribute:
• Straining during bowel movements
• Chronic constipation or diarrhea
• Sitting on the toilet for long periods
• Pregnancy and childbirth
• Low-fiber diet and inadequate fluids
• Obesity or heavy lifting
• Aging (weakened supporting tissues)
Consult a Top General Physician
What is an anal fistula?
An anal fistula is an abnormal tunnel between the inside of the anal canal or rectum and the skin around the anus. Most anal fistulas start after an anal gland infection that forms an abscess. When the abscess drains (on its own or with treatment), a persistent tunnel can remain, connecting the gland to the skin surface.
Common symptoms
• Persistent drainage of pus or blood from a small opening near the anus
• Pain, swelling, or irritation around the anus
• A skin opening that repeatedly becomes tender or forms an abscess
• Fever or feeling unwell during active infection (abscess)
• Soiling or foul-smelling discharge
What causes an anal fistula?
• Most commonly: a previous anal gland abscess (cryptoglandular infection)
• Less commonly: inflammatory bowel disease (especially Crohn’s disease), prior surgery or trauma, radiation therapy, or rarely certain infections
• People with diabetes or weakened immunity may be at higher risk for infection-related complications
Piles vs fistula: key differences
Understanding piles vs fistula helps you identify what you might be dealing with:
Origin
• Piles: swollen veins (vascular problem)
• Fistula: abnormal tunnel from infection (tract connecting anal canal to skin)
Main symptoms
• Piles: bleeding with bowel movements, itching, discomfort; a painful lump if thrombosed
• Fistula: persistent drainage (pus or blood), recurrent abscesses, pain that may improve after drainage
Pain pattern
• Piles: often painless bleeding; external thrombosis can cause sudden sharp pain
• Fistula: ongoing soreness, swelling, and discharge; pain can spike with abscess
Visible signs
• Piles: swollen vein or prolapsing tissue
• Fistula: small opening on the skin that drains; sometimes a cord-like tract can be felt
Treatment approach
• Piles: often improve with lifestyle changes, fiber, and office procedures; surgery for severe cases
• Fistula: usually needs a surgical solution to heal (after managing any infection)
Complications
• Piles: anemia from chronic bleeding (uncommon), thrombosis, irritation
• Fistula: recurrent infections or abscesses; rarely, more complex tracts involving the sphincter muscles
Causes and risk factors
Risk factors for hemorrhoids
• Low-fiber diet and dehydration
• Straining or prolonged time on the toilet
• Chronic constipation or diarrhea
• Pregnancy and postpartum changes
• Obesity
• Aging and weakened pelvic support
Risk factors for anal fistula
• Prior anal abscess (most common)
• Crohn’s disease or other inflammatory bowel disease
• Trauma or prior anorectal surgery
• Diabetes or immunosuppression (higher risk of infection-related issues)
When to seek medical care?
Call a healthcare professional if you have:
• Heavy rectal bleeding, black or maroon stools, or symptoms of anemia (fatigue, dizziness)
• Severe pain, fever, chills, or a tender swelling near the anus (possible abscess)
• Persistent drainage or a nonhealing opening near the anus (possible fistula)
• Symptoms that don’t improve with home care after a week or two
• A history of inflammatory bowel disease or cancer, or if you’re pregnant or immunocompromised
Note: Rectal bleeding isn’t always from hemorrhoids—polyps, fissures, inflammatory bowel disease, or even colorectal cancer can cause bleeding. Get evaluated if you’re unsure.
How doctors diagnose piles vs fistula?
Medical history and symptom review: bleeding vs drainage, pain pattern, bowel habits, prior abscesses, underlying conditions.
Physical exam: visual inspection of the anal area; digital rectal exam.
Anoscopy or proctoscopy: to see internal hemorrhoids and other causes of bleeding.
For suspected fistula:
• Identification of the external opening and gentle probing by a specialist
• Imaging when needed: MRI pelvis or endoanal ultrasound can map complex tracts
• Exam under anesthesia (EUA) for detailed assessment and planning treatment
Treatment options
Hemorrhoids (piles)
Home care and lifestyle
• Fiber: Aim for about 25–35 grams daily from food (fruits, vegetables, whole grains, beans) and consider a fiber supplement if needed.
• Hydration: Plenty of water to keep stools soft.
• Toilet habits: Don’t strain; don’t sit on the toilet for long periods; respond to the urge promptly.
• Sitz baths: Warm water soaks for 10–15 minutes, 2–3 times daily, to ease discomfort.
• Topicals: Short-term use of over-the-counter creams or wipes with hydrocortisone, witch hazel, or protective ointments may relieve symptoms. Avoid long-term steroid use without guidance.
Office procedures (for persistent internal hemorrhoids)
• Rubber band ligation: Often first choice for internal hemorrhoids that bleed or prolapse mildly to moderately.
• Sclerotherapy: Injection that shrinks hemorrhoids.
• Infrared coagulation: Uses heat to scar and shrink internal hemorrhoids.
Surgery (for severe or recurrent cases)
• Hemorrhoidectomy: Surgical removal of hemorrhoids; effective for large or very symptomatic hemorrhoids.
• Stapled hemorrhoidopexy: A technique for selected prolapsing internal hemorrhoids; may have different risks and recurrence profiles. A colorectal surgeon can advise on suitability.
Anal fistula
Manage infection first
Abscesses are treated with incision and drainage. Antibiotics may be used for fever, surrounding skin infection, or in people with certain conditions (e.g., diabetes or immunosuppression), but antibiotics alone don’t cure a fistula.
Definitive procedures
• Fistulotomy: Opening the fistula tract to heal from the inside out; typically for simple, superficial tracts that don’t cross much of the sphincter muscle.
• Seton placement: A thread placed through the tract to promote drainage and protect the sphincter; used alone or staged before other treatments.
• LIFT procedure (ligation of intersphincteric fistula tract): Closes the tract in the intersphincteric space, aiming to preserve continence.
• Advancement flap: Uses healthy tissue to cover the internal opening, often for complex or high tracts.
• Other options: Fibrin glue or plugs may be considered in selected cases.
Special situations
Crohn’s disease–related fistulas may need combined care with a gastroenterologist (medical therapy such as biologics) and surgical strategies tailored to disease severity.
Follow-up
Healing takes time; you’ll need follow-up to monitor drainage, pain, and continence. Recurrence can happen, especially with complex tracts, so ongoing care is important.
Everyday tips to protect anal health
Small changes can make a big difference for comfort and prevention:
• Eat fiber-rich foods and drink enough water daily.
• Keep bowel movements regular; consider a stool softener if your doctor recommends it.
• Avoid straining and limit time on the toilet (use a footstool to improve alignment if helpful).
• Stay active; regular movement supports bowel function.
• Practice gentle hygiene: clean with water or alcohol-free wipes; pat dry; avoid harsh soaps.
• Manage diarrhea quickly (oral rehydration, simple diet, and medical advice if persistent).
• During pregnancy and postpartum, use fiber, fluids, and sitz baths to reduce hemorrhoid symptoms.
• Seek early care for any painful lump, fever, or persistent drainage near the anus.
Consult a Top General Physician
Consult a Top General Physician

Dr. Chethan T L
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD, DNB (General Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Rohit Basu
General Practitioner
8 Years • MBBS, DNB (General surgery)
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr Aakash Andgi
General Physician/ Internal Medicine Specialist
9 Years • MBBS MD
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Tanzeem Shajahan
General Physician/ Internal Medicine Specialist
7 Years • MBBS, MD (General Medicine)
Bengaluru
Medwin multispeciality clinic, Bengaluru
Consult a Top General Physician

Dr. Chethan T L
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD, DNB (General Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Rohit Basu
General Practitioner
8 Years • MBBS, DNB (General surgery)
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr Aakash Andgi
General Physician/ Internal Medicine Specialist
9 Years • MBBS MD
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Tanzeem Shajahan
General Physician/ Internal Medicine Specialist
7 Years • MBBS, MD (General Medicine)
Bengaluru
Medwin multispeciality clinic, Bengaluru
More articles from General Medical Consultation
Frequently Asked Questions
Q1: How can I tell if it’s piles or an anal fistula?
Piles usually cause bright red bleeding with bowel movements, itching, and sometimes a lump. A fistula often causes ongoing drainage of pus or blood from a small skin opening, sometimes with a history of an abscess. A clinician can examine and confirm the diagnosis.
Q2: Can hemorrhoids turn into a fistula?
No. They are different conditions. Hemorrhoids are swollen veins, while a fistula is a tract formed after infection. However, both can occur in the same person for different reasons.
Q3: Do hemorrhoids always need surgery?
No. Many improve with fiber, fluids, sitz baths, and better toilet habits. Office procedures like rubber band ligation help if symptoms persist. Surgery is reserved for severe or recurrent cases.
Q4: Will antibiotics cure an anal fistula?
Antibiotics can help control infection or treat surrounding skin infection, but they do not close the fistula. Most fistulas need a procedure (such as fistulotomy, seton, or LIFT) to heal.
Q5: Is rectal bleeding always from hemorrhoids?
No. Bleeding can come from fissures, polyps, inflammatory bowel disease, or colorectal cancer. If you have new, heavy, or persistent bleeding—or you’re over age 45–50 and not up to date on screening—see a healthcare professional.