What Leads To Signs Of Pleural Effusion And Types
Understand pleural effusion, its causes, symptoms, types, diagnosis, treatments, and recovery. Learn when to seek medical help and how Apollo 24|7 can assist.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. M L Ezhilarasan MBBS
Last updated on 13th Jan, 2026
Introduction
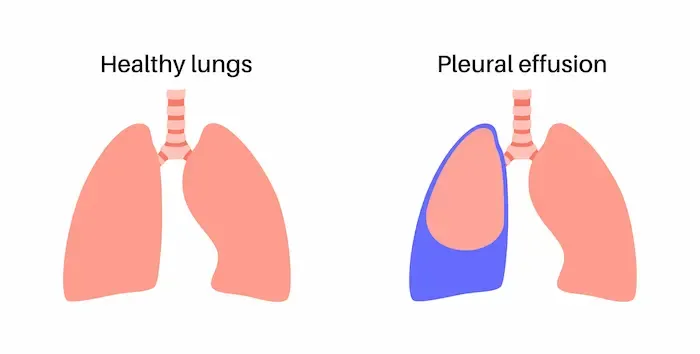
Breathing should feel effortless, but when fluid builds up around the lungs—a condition called pleural effusion—it can make each breath feel like a task. The pleura are thin membranes lining your lungs and chest wall; normally, only a small amount of fluid is present to help the lungs glide smoothly. When that balance is upset, excess fluid collects and causes symptoms like shortness of breath, chest discomfort, or cough. This guide explains what leads to pleural effusion, the different types you may hear about, and how doctors diagnose and treat it. We’ll walk through common causes such as heart failure, pneumonia, cancer, tuberculosis, and injury, and clarify terms like “transudate,” “exudate,” and “empyema.” You’ll also learn what imaging and tests show, how procedures like thoracentesis work, and what recovery looks like at home. If symptoms persist or worsen, timely medical advice matters—especially if breathing is difficult. Read on for a clear, practical overview designed for you and your family, with expert insights and real-world tips woven in.
Pleural Effusion in Plain Language
Pleural effusion means extra fluid collects in the pleural space—the thin, fluid-filled area between the lungs and the inside of the chest. The pleura have two layers: one sticks to the lung, the other to the chest wall. Normally, about a teaspoon or two of lubricating fluid stays in this space to help your lungs slide as you breathe.
How much fluid is normal—and when is it “too much”?
- Normal: A very thin layer of fluid, constantly produced and reabsorbed.
- Too much: Anything that causes more fluid to enter than leave the space can create a pleural effusion. Even small effusions can cause symptoms if you have underlying lung or heart problems; large effusions can compress the lung and make breathing hard.
How pleural effusion affects breathing
- The extra fluid takes up space, making it harder for the lung to expand.
- This can cause shortness of breath, especially during activity or when lying flat.
- If the pleural lining gets inflamed (like with infection), sharp pain with deep breath (pleuritic pain) can occur.
Unique insight: The amount of discomfort doesn’t always match the volume. A modest left-sided effusion in a person with asthma or COPD may feel worse than a larger effusion in someone with otherwise healthy lungs because their “reserve” is limited.
Why Pleural Effusions Happen: The Fluid Balance Explained
Three forces control pleural fluid levels: pressure in blood vessels, the protein content of blood, and how “leaky” (permeable) the pleura and nearby capillaries are.
- Pressure: High pressure in the lungs’ blood vessels (as in heart failure) pushes fluid out into the pleural space.
- Protein: Low blood protein (albumin), seen in liver disease or kidney syndromes, reduces the “pull” that keeps fluid inside vessels.
- Permeability: Inflammation or injury (infection, cancer, clots) makes vessels leakier, allowing protein-rich fluid and cells to enter.
Transudate vs exudate at a glance
- Transudate: Mostly water that seeps out due to pressure or protein imbalances. Common with heart failure or cirrhosis.
- Exudate: Protein-rich fluid from inflammation, infection, or malignancy. Common with pneumonia, cancer, tuberculosis (TB), or pulmonary embolism.
Common pathways to fluid build-up
- Increased hydrostatic pressure: Congestive heart failure.
- Decreased oncotic pressure: Nephrotic syndrome, severe malnutrition, liver disease.
- Increased capillary permeability: Pneumonia, TB, malignancy.
- Lymphatic obstruction: Cancer blocking drainage, chylothorax.
- Direct leak: Trauma or surgery (hemothorax), urine (urinothorax) from urinary tract obstruction.
Understanding these mechanisms helps clinicians choose tests and treatments that match the cause rather than just removing fluid.
Consult Top Specialists Here
Signs and Symptoms You Might Notice
Here are the signs and symptoms of pleural effusion:
Typical symptoms
- Shortness of breath (especially when exerting or lying down)
- Chest pain, often sharp and worse with deep breaths (pleuritic pain)
- Dry or occasionally productive cough
- Reduced exercise tolerance; fatigue
- Hiccups or shoulder pain if the diaphragm is irritated
Red flags needing urgent care
- Severe breathlessness at rest or bluish lips/fingertips
- High fever and chills with chest pain (possible empyema)
- Coughing up blood
- Sudden chest pain with fast heart rate (possible pulmonary embolism)
- Confusion, fainting, or very low oxygen readings
If you experience any of these, call emergency services or go to the nearest emergency department.
What doctors look for on examination
- Reduced breath sounds and dull percussion note over the effusion
- Decreased chest expansion on the affected side
- Reduced vocal vibrations (tactile fremitus)
- A pleural friction rub may be heard early in inflammation
Unique insight: Symptoms from pleural effusion often fluctuate during the day. Keeping a simple diary of breathlessness (e.g., how many stairs you can climb), position that feels best, and your temperature helps your clinician spot trends and complications early.
Main Types of Pleural Effusion
Here are the types of pleural effusion:
Transudative effusions
- Causes: Heart failure, cirrhosis with ascites (hepatic hydrothorax), nephrotic syndrome, dialysis-related fluid shifts
- Clues: Mild inflammation, clear/straw-colored fluid, low protein, low LDH
Exudative effusions
- Causes: Pneumonia (parapneumonic), cancer (malignant), TB, pulmonary embolism, pancreatitis, autoimmune disease
- Clues: Inflammatory features, higher protein and LDH, sometimes low glucose or low pH
Special types
- Parapneumonic effusion: Fluid from pneumonia; can progress to empyema
- Empyema: Thick, infected fluid; often needs chest tube and antibiotics
- Malignant pleural effusion: Due to cancer; often recurs, may need drainage, pleurodesis, or indwelling catheter
- Hemothorax: Blood in pleural space; pleural fluid hematocrit ≥50% of blood
- Chylothorax: Milky fluid rich in triglycerides from lymphatic leak
- TB effusion: Often exudative with high ADA
- Hepatic hydrothorax: Right-sided transudative effusion linked to cirrhosis
- Urinothorax: Rare; urine enters pleural space
- Pseudochylothorax: Long-standing effusion with high cholesterol crystals
- Trapped lung: Lung cannot re-expand due to fibrous peel
Unique insight: Left-sided isolated transudates are less typical for heart failure; clinicians often look for malignancy or pancreatitis.
How Pleural Effusion Is Diagnosed?
Here’s how pleural effusion is diagnosed:
Imaging
- Chest X-ray: First-line, shows blunted costophrenic angles; lateral decubitus helps detect small volumes
- Ultrasound: More sensitive; guides thoracentesis
- CT scan: Detects loculations, pleural thickening, malignancy, alternative diagnoses
Thoracentesis and Light’s criteria
- Needle procedure to remove fluid for testing
- Exudate if any:
- Pleural fluid protein/serum protein >0.5
- Pleural fluid LDH/serum LDH >0.6
- Pleural fluid LDH >2/3 upper limit of normal serum
- Additional tests: pH, glucose, cell counts, cytology, ADA, triglycerides, hematocrit
Unique insight: Bedside ultrasound can reveal septations within fluid; these often respond better to chest tube plus fibrinolytics or VATS.
Treatment: Matching the Cause to the Right Care
Here is the treatment for pleural effusion:
- Transudates: Diuretics, salt restriction, optimize heart failure; TIPS for hepatic hydrothorax
- Exudates from pneumonia: Antibiotics; drain if pH <7.20 or pus present
- Pulmonary embolism: Anticoagulation; drainage if symptomatic
- TB effusion: Anti-TB therapy
- Malignant: Thoracentesis, pleurodesis, or indwelling catheter
When to drain: Moderate-to-large effusion causing breathlessness or for diagnostic purposes; remove ≤1–1.5 L at a time to avoid re-expansion pulmonary edema.
Unique insight: Mixed causes (e.g., heart failure + pneumonia) may need combination therapy and early ultrasound reassessment.
Procedures You May Hear About
- Therapeutic thoracentesis: Minimally invasive, ultrasound-guided; risks include pain, bleeding, infection, pneumothorax
- Chest tubes + fibrinolytics: For empyema or loculated effusions
- VATS: Minimally invasive surgery for loculations, decortication, or biopsy
- Pleurodesis + indwelling catheters: Prevent recurrent malignant effusions; IPC allows home drainage
Unique insight: IPCs reduce hospital visits and improve home symptom control.
Living With and Recovering From a Pleural Effusion
- Breathing strategies: Sit upright, extra pillows, paced/pursed-lip breathing, incentive spirometry
- Tracking: Daily breathlessness, temperature, weight, oxygen saturation
- Follow-up: Imaging as advised; vaccines reduce pneumonia risk; maintain nutrition/protein
- Home tests: Apollo 24|7 offers home collection for blood tests
Unique insight: Night-to-night breathlessness can indicate effusion dynamics; note which side worsens for clinician guidance.
Special Situations and Populations
- Children: Parapneumonic effusions common; antibiotics + ultrasound-guided drainage
- Older adults: Diuretics cautiously used; frailty affects procedure choice
- Pregnancy: Causes include PE or preeclampsia; ultrasound is safe
Unique insight: ADA testing helps identify TB effusion when biopsy or CT is limited.
Complications to Know About
- Empyema and trapped lung: Early drainage + antibiotics prevent fibrous peel
- Re-expansion pulmonary edema: Rare; monitor symptoms during drainage
- Malignant effusion: Often recurs; focus on symptom relief and quality of life
Unique insight: Ambulatory IPC pathways reduce hospitalisation and empower home care.
When to Seek Help and Where to Get It
- Urgent symptoms: Severe breathlessness, chest pain with fever, confusion, bluish lips
- Online vs in-person: Mild/moderate symptoms can start with online consult; procedures require in-person care
- Apollo 24|7: Online doctor consults, home test collection, or physical visits as needed
Quick Takeaways
- Pleural effusion is excess fluid around the lungs causing breathlessness
- Classified as transudate or exudate via Light’s criteria
- Imaging + thoracentesis are core diagnostics
- Treat cause first; drain when infected, large, or symptomatic
- Special types require tailored care (empyema, malignant, chylothorax, hemothorax)
- Early attention prevents complications; monitor symptoms and follow-up
- Seek medical advice online via Apollo 24|7 or in-person if symptoms persist or worsen
Conclusion
Pleural effusion has diverse causes, including heart failure, pneumonia, TB, clots, and cancer. Early recognition and targeted care improve outcomes. Doctors use examination, imaging, and thoracentesis to classify effusions and guide treatment—diuretics, antibiotics, drainage, fibrinolytics, pleurodesis, or indwelling catheters. Many effusions improve with treatment of the underlying condition, while others require procedural interventions. Home monitoring of breathlessness, weight, and oxygen helps detect changes early. Persistent or severe symptoms should prompt an online consult with Apollo 24|7 or immediate in-person care. With timely evaluation and proper management, most people can breathe more easily and resume daily activities.
Consult Top Specialists Here
Consult Top Specialists Here

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Srujana Mulakalapalli
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD (GENERAL MEDICINE)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
(25+ Patients)

Dr. Harshendra Jaiswal
General Physician/ Internal Medicine Specialist
12 Years • MBBS , MD (General medicine)
Kolkata
108 DHANA DHANVANTARI Clinic, Kolkata
(25+ Patients)
Consult Top Specialists Here

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Srujana Mulakalapalli
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD (GENERAL MEDICINE)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
(25+ Patients)

Dr. Harshendra Jaiswal
General Physician/ Internal Medicine Specialist
12 Years • MBBS , MD (General medicine)
Kolkata
108 DHANA DHANVANTARI Clinic, Kolkata
(25+ Patients)
More articles from General Medical Consultation
Frequently Asked Questions
1) Is pleural effusion the same as pneumonia?
No. Pneumonia is an infection in lung tissue. Parapneumonic effusion is fluid accumulation around the lung during pneumonia; some progress to empyema, requiring drainage plus antibiotics.
2) What is the difference between transudate and exudate?
Transudate forms from pressure or protein imbalance (e.g., heart failure); exudate forms from inflammation or blockage (e.g., pneumonia, cancer, TB). Light’s criteria help differentiate.
3) Do all pleural effusions need drainage?
No. Small transudates may improve with diuretics alone. Drainage is for symptomatic, infected, or diagnostically unclear effusions.
4) Can pleural effusion recur?
Yes. Recurrence depends on the cause. Malignant effusions and hepatic hydrothorax often recur; pleurodesis or indwelling catheter can reduce repeat interventions.
5) Is thoracentesis painful or risky?
Usually well tolerated with local anaesthesia. Risks include discomfort, bleeding, infection, or