Gynecomastia Explained: Causes, Symptoms, Treatment
Discover everything about gynecomastia, including its causes, symptoms, diagnosis, and treatment options such as medications and surgery. Learn how to differentiate it from chest fat and when to consult a doctor.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026
Introduction
Gynecomastia—often described as male breast enlargement—can be confusing and stressful, whether it appears during the teen years, after starting a new medication, or later in life. The good news is that most cases are benign, manageable, and sometimes reversible. This guide explains what gynecomastia is, why it happens, how it’s diagnosed, and the full range of treatment options—from watchful waiting to medications and surgery. You’ll also learn how to differentiate gynecomastia from chest fat, when to seek medical advice, and how lifestyle changes can help.
If you notice a new lump, one-sided swelling, pain, or nipple discharge, don’t ignore it. If symptoms persist beyond two weeks or you’re unsure what you’re dealing with, consult a doctor online with Apollo 24|7 for further evaluation.
What is Gynecomastia?
Here's what you need to know:
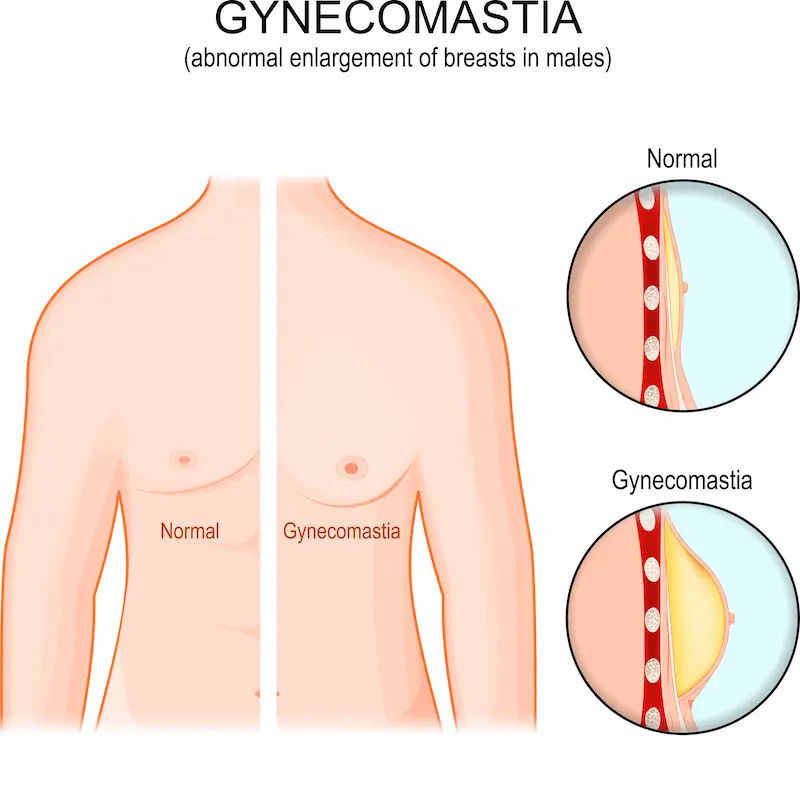
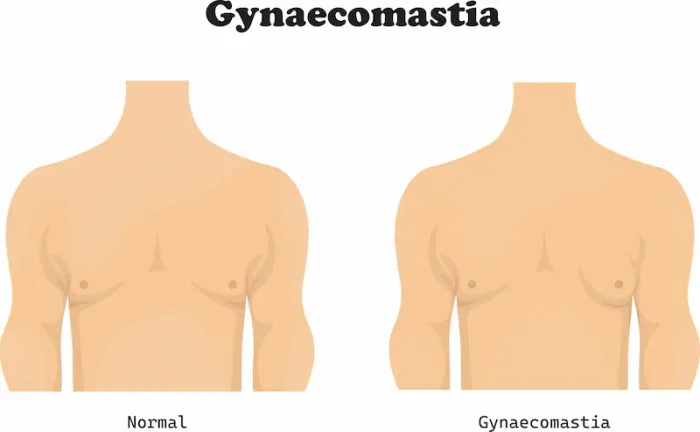
Gynecomastia is the benign enlargement of male breast gland tissue, usually caused by a shift in the balance between oestrogen and testosterone. It appears as a rubbery or firm mound of tissue beneath the nipple-areola, affecting one or both sides, and sometimes causing tenderness. Importantly, gynecomastia differs from excess chest fat, as it involves true gland tissue growth. Most cases are not dangerous, and many are temporary, especially during puberty or after a medication change.
Gynecomastia vs Pseudogynecomastia
Pseudogynecomastia refers to increased fat in the chest without gland tissue growth. Pinch the area around the nipple: firm, disc-like tissue behind the areola suggests gynecomastia, while a diffuse, soft feel suggests fat. Ultrasound can help distinguish the two if necessary. Weight loss improves fat-related fullness but does not reliably reduce gland tissue.
What Normal Male Breast Tissue Feels Like
Normal male breast tissue is a thin, flat layer under the nipple. Gynecomastia is more prominent and often tender early on. Any hard, irregular, non-movable lump, especially if one-sided, requires prompt medical evaluation to rule out male breast cancer.
How Common Is It—and Who Gets It?
Here's a breakdown by life stage:
Gynecomastia is common across the lifespan. Newborn boys may have temporary breast swelling from maternal hormones, which usually resolves within weeks. During puberty, up to half of boys experience some degree of gynecomastia, typically peaking at ages 13–14, and most cases resolve within 6–24 months without treatment. In older adults, prevalence increases as testosterone levels decline and medications or comorbidities accumulate; estimates range from about one-third to over half in older men.Consult Top Specialists
Life Stages: Newborns, Puberty, and Older Adults
• Newborns: Transient swelling from maternal oestrogens, usually self-limiting
• Puberty: Common, usually self-limited; reassurance and observation are often sufficient
• Older adults: Persistent cases linked to age-related hormonal shifts, medications such as antiandrogens or finasteride, liver or kidney disease, and thyroid disorders
Prevalence and Natural Course
Most pubertal cases resolve within 1–2 years. Persistent gynecomastia beyond that timeframe, rapidly enlarging breasts, or significant pain merits a medical review. Persistent or progressive adult gynecomastia is less likely to regress spontaneously and may require treatment. If symptoms persist beyond two weeks or worsen, consult a doctor online with Apollo 24|7.
Why Gynecomastia Happens: The Root Causes
Here's why it happens:
Gynecomastia occurs due to a change in the oestrogen-to-androgen balance at the breast tissue level. Increased oestrogen stimulation or decreased androgen effect encourages gland growth. Causes include puberty, aging, obesity, liver disease, hyperthyroidism, kidney disease, testicular disorders, or tumours affecting hormones.
Hormone Balance: Oestrogen-androgen Ratio
Even minor increases in oestrogen action or decreases in testosterone can promote breast tissue growth. Conditions such as primary hypogonadism, Klinefelter syndrome, or pituitary/testicular disorders reduce testosterone. Obesity increases aromatisation, raising oestrogen exposure to the breast.
Medications and Substances That Trigger Gynecomastia
Common culprits include antiandrogens, 5-alpha-reductase inhibitors, spironolactone, certain antipsychotics and antidepressants, HIV medications, anabolic steroids, alcohol, and some chemotherapy drugs. Review any new or recently changed medications if breast enlargement appears.
Health Conditions Linked to Gynecomastia
• Endocrine: Hypogonadism, hyperthyroidism
• Systemic: Cirrhosis, chronic kidney disease
• Tumours: Testicular, adrenal, or hCG-secreting tumours
• Genetic: Klinefelter syndrome
Supplements, Essential Oils, and SARMs
Topical lavender or tea tree oils have been linked to prepubertal gynecomastia. Some unregulated testosterone boosters and selective androgen receptor modulators (SARMs) may disrupt hormones, causing gynecomastia. Marijuana may pose a risk, though evidence is mixed.
Symptoms, Red Flags, and When to Worry
Here's what to look for:
Typical gynecomastia presents as a symmetrical, rubbery or firm mound beneath the nipple, often with early tenderness. It may be unilateral or bilateral. Painful gynecomastia is common initially and often decreases over months.
Male Breast Cancer vs Gynecomastia
• Gynecomastia: Subareolar, rubbery, often tender, may involve both sides
• Suspicious for cancer: Hard, irregular, fixed mass, often off-centre; skin dimpling, nipple retraction, bloody discharge; enlarged armpit nodes; age over 40; strong family history. Seek urgent evaluation if these are present
When to See a Doctor
See a doctor promptly for one-sided firm lumps, nipple discharge, skin changes, or rapidly enlarging tissue. Mild, painless pubertal gynecomastia can be monitored for 12–24 months. Adults with persistent, progressive, or painful gynecomastia should seek evaluation. If clinic access is difficult, consult a doctor online with Apollo 24|7.
Diagnosis: What to Expect at the Clinic
Here's the diagnostic approach:
History and Physical Exam
Clinicians ask about timing, pain, sexual function, weight changes, medications/supplements, alcohol/drug use, and family history. The exam evaluates breast tissue, testicular size/masses, thyroid, liver signs, and lymph nodes.
Lab Tests and Imaging
Not everyone needs tests. Adults with persistent or unexplained gynecomastia may have:
• Blood tests: Total and free testosterone, estradiol, LH/FSH, hCG, prolactin, TSH, liver and kidney function
• Imaging: Testicular ultrasound if a mass is suspected or hCG elevated; breast imaging (mammogram/ultrasound) if atypical features or cancer concernConsult Top Specialists
At-Home Test Collection
Home sample collection can accelerate diagnosis. Coordinate collection when well-rested and fasting if required.
Treatment Options That Work
Here's how treatment works:
Watchful Waiting and Treating the Cause
• Puberty: Observation is first-line; most cases regress in 6–24 months
• Medications: Discuss alternatives with your doctor; do not stop prescriptions independently
• Underlying conditions: Treat thyroid, liver, kidney, or hormone disorders
Medications (SERMs, Aromatase Inhibitors)
In recent-onset, tender gynecomastia (<12 months):
• SERMs (tamoxifen, raloxifene) reduce pain and gland size in some patients
• Aromatase inhibitors show mixed results and are generally less effective than SERMs
• Best results occur in the early, active phase; chronic tissue is less responsive
Discuss benefits and risks with your clinician
Surgery: Techniques, Recovery, and Results
Surgery is used for long-standing or significant gynecomastia. Techniques include subcutaneous mastectomy and liposuction, often combined. Recovery usually takes days to weeks with compression garments. Complications are uncommon but may include bleeding, contour irregularities, or altered nipple sensation. Results are typically durable, especially when the underlying cause is addressed.
Lifestyle, Self-Care, and Prevention
Here's what helps:
Diet, Exercise, and Weight Management
• Sustainable calorie deficit and strength training reduce body fat and improve chest appearance
• Compound lifts enhance muscle base and posture
• Limit alcohol; maintain sleep and manage stress
Clothing, Posture, and Confidence Tips
• Compression tops can smooth chest contours
• Improve posture to prevent the chest from appearing more prominent
Mental Health
Gynecomastia can affect mood and confidence. Cognitive-behavioural strategies, peer support, or counselling can help.
Special Situations
Here's how it varies by group:
Puberty-Related Gynecomastia
Usually painless and resolves in 1–2 years. Red flags warrant evaluation. Compression shirts may help with comfort. Consult Apollo 24|7 if symptoms persist.
Athletes and Bodybuilders
Steroids and SARMs can lead to gynecomastia. Avoid these substances and seek early medical advice if breast tissue enlarges.
Older Men
Medication reviews are essential. Common contributors include antiandrogens, finasteride/dutasteride, spironolactone, and other drugs. Manage comorbidities and discuss ongoing medication use.
Conclusion
Gynecomastia is common, often temporary, and usually manageable. Confirm it is true gland enlargement, address reversible causes, and match treatment to severity. Early, painful gynecomastia may respond to medications, while long-standing cases often benefit from surgery. Lifestyle choices—healthy weight, strength training, reduced alcohol, and better sleep—support hormone balance and confidence. If your condition does not improve, book a physical visit to a doctor with Apollo 24|7 for targeted treatment. Evidence-based options can help you feel and look better safely.Consult Top Specialists
Consult Top Specialists

Dr. Ramesh H
Urologist
16 Years • MBBS, MS , Mch( Urology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Sudhakar G V
Urologist
25 Years • MBBS, MS(Gen.Surgery), DNB Urology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Pavan Kumar S K
Urologist
11 Years • MBBS, MS , Mch( Urology) DNB (Urology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Samiran Das Adhikary
Urologist
26 Years • MBBS; MS(General Surgery); Mch(Urology). Senior Consultant - Urology & Renal Transplant Surgery
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr Anupam Sharma
Urologist
18 Years • MBBS, MS(Gen Surgery), DNB (Urology)
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)
Consult Top Specialists

Dr. Ramesh H
Urologist
16 Years • MBBS, MS , Mch( Urology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Sudhakar G V
Urologist
25 Years • MBBS, MS(Gen.Surgery), DNB Urology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Pavan Kumar S K
Urologist
11 Years • MBBS, MS , Mch( Urology) DNB (Urology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Samiran Das Adhikary
Urologist
26 Years • MBBS; MS(General Surgery); Mch(Urology). Senior Consultant - Urology & Renal Transplant Surgery
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr Anupam Sharma
Urologist
18 Years • MBBS, MS(Gen Surgery), DNB (Urology)
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)
Consult Top Specialists

Dr. Ramesh H
Urologist
16 Years • MBBS, MS , Mch( Urology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Sudhakar G V
Urologist
25 Years • MBBS, MS(Gen.Surgery), DNB Urology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Pavan Kumar S K
Urologist
11 Years • MBBS, MS , Mch( Urology) DNB (Urology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Samiran Das Adhikary
Urologist
26 Years • MBBS; MS(General Surgery); Mch(Urology). Senior Consultant - Urology & Renal Transplant Surgery
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr Anupam Sharma
Urologist
18 Years • MBBS, MS(Gen Surgery), DNB (Urology)
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)
More articles from gynaecomastia
Frequently Asked Questions
1) Can gynecomastia go away naturally?
Yes. Pubertal gynecomastia often resolves within 6–24 months. Adult-onset cases are less likely to fully regress without addressing the cause.
2) How do I tell gynecomastia from fat (pseudogynecomastia)?
Gynecomastia feels like a firm, disc-like mound beneath the nipple; fat is softer and more diffuse. Ultrasound can help if the exam is unclear. Weight loss improves fat-related fullness more than gland tissue.
3) What’s the best medication for early, painful gynecomastia?
Tamoxifen has the strongest evidence for reducing pain and size in recent-onset cases. Discuss risks and benefits with your clinician.
4) Do marijuana or essential oils cause gynecomastia?
Evidence for marijuana is mixed. Lavender and tea tree oils have been linked to prepubertal gynecomastia; symptoms resolved after stopping exposure.
5) How much does gynecomastia surgery cost and what is recovery like?
Costs vary by location and extent of surgery. Recovery typically involves a few days off normal activities and several weeks of compression garments. Most patients are satisfied with contour improvements; discuss expectations and risks with a surgeon.