Gynecomastia Causes, Treatment, and What to Do
Learn about gynecomastia, the benign enlargement of male breast tissue. Explore causes, symptoms, diagnosis, treatment options, lifestyle tips, and when to see a doctor.

Written by Dr. Siri Nallapu
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026
Introduction
If you’ve noticed breast enlargement or tenderness in one or both sides of your chest, you’re not alone. Gynecomastia—noncancerous enlargement of male breast tissue—affects boys and men at different ages and for many reasons. Sometimes it’s a normal part of puberty or ageing. Other times, it’s driven by medicines, hormone shifts, or health conditions. The good news: gynecomastia is common, usually harmless, and often treatable.
In this clear, comprehensive guide, we explain what gynecomastia is, how to tell it apart from simple fat gain (pseudogynecomastia), and what causes it. You’ll learn what symptoms to watch for, when to see a doctor, and how gynecomastia is diagnosed. We’ll cover treatment options—ranging from watchful waiting and lifestyle steps to medicines and surgery—plus practical advice for teens, athletes, and men on testosterone therapy. You’ll also find cost and access tips, visual explanations, and answers to the most searched questions.
Whether you want reassurance, a plan to reduce pain and swelling, or guidance about next steps, this article gives you the facts and the options to move forward with confidence.
Understanding Gynecomastia: What It Is and How Common
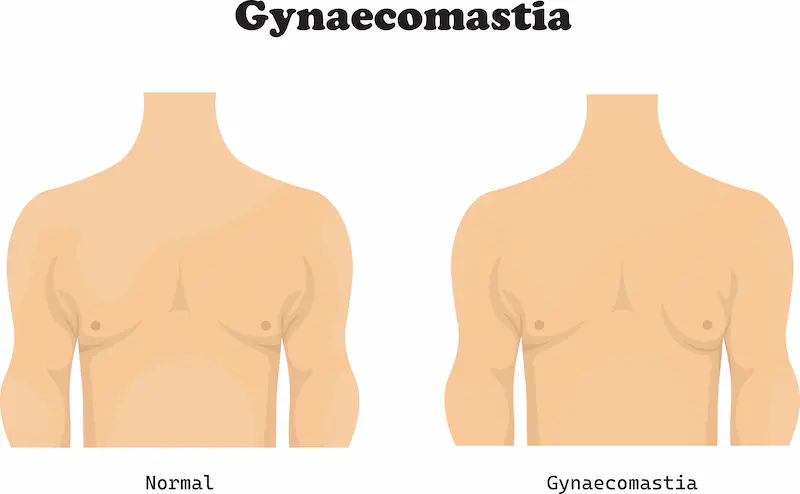
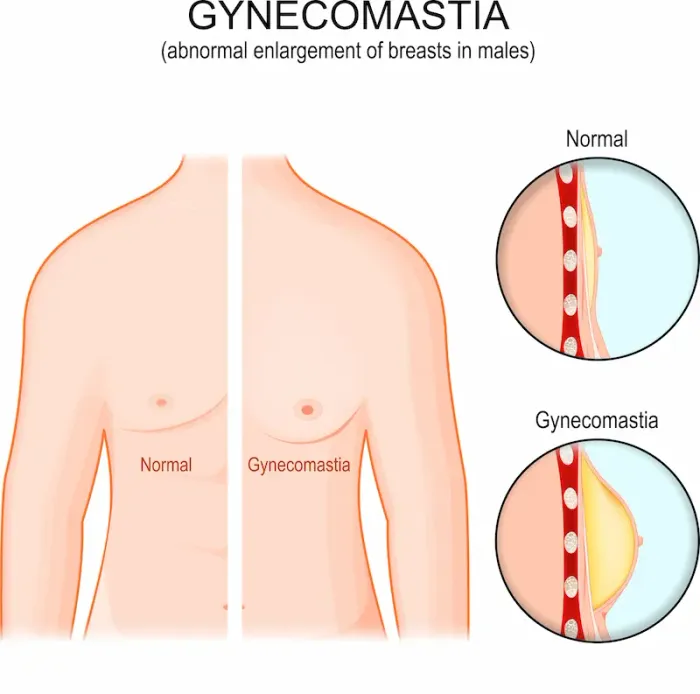
Gynecomastia is the benign growth of glandular breast tissue in males caused by an imbalance between estrogen (which stimulates breast tissue) and androgens like testosterone (which counteract that effect). It typically presents as a rubbery or firm disk of tissue directly under the nipple-areola complex and can affect one or both sides. The condition is different from fat accumulation and can be tender, especially early on.
How common is it? Transient gynecomastia is very common at certain ages. In newborns, maternal hormones can lead to temporary breast swelling that usually resolves within weeks. During puberty, up to half of boys experience gynecomastia, often appearing around ages 13–14 and resolving within 6–24 months in most cases. In older men, the prevalence increases again—studies suggest that more than a third of men develop some degree of gynecomastia with advancing age due to declining testosterone and increased conversion of androgens to estrogens in body fat.
The key concept is hormone balance: even normal estrogen levels can promote breast tissue if there’s relatively less testosterone effect. That’s why conditions that reduce testosterone or increase estrogen availability—certain medical conditions, medications, or increased body fat—can make gynecomastia more likely. Most cases are benign and self-limited, but recognising red flags and understanding your options can make a big difference.Consult Top Specialists Here
Gynecomastia vs. Pseudogynecomastia: Spot the Difference
Not all chest enlargement is gynecomastia. Pseudogynecomastia (lipomastia) is simply fat deposition in the chest without true glandular growth. Here’s how to tell them apart:
What you feel:
• Gynecomastia: a firm, disk-like rubbery tissue under the nipple and areola, often symmetric around the nipple; may be tender initially.
• Pseudogynecomastia: soft, diffuse fat without a discrete glandular “button” beneath the nipple; usually not tender.
What weight loss does:
• Gynecomastia: fat may reduce, but the central glandular tissue often persists.
• Pseudogynecomastia: chest size typically decreases with overall weight loss and improved body composition.
Imaging and exam:
• A trained clinician can often differentiate by physical exam. When unclear, breast ultrasound can help distinguish gland from fat.
Why it matters:
• Pseudogynecomastia responds best to weight loss, nutrition, and resistance training.
• True gynecomastia may need watchful waiting, medication review, or surgery if persistent or distressing.
Practical tip: If you can pinch a soft fold across the nipple without feeling a central firm disk, pseudogynecomastia is more likely. If you’re unsure, a brief exam can be definitive. If tenderness persists or a lump feels firm and fixed, seek medical advice promptly. If symptoms persist beyond two weeks or are rapidly worsening, consult a doctor online with Apollo 24|7 for further evaluation.
Unique insight: Post-weight-loss “stubborn chest” is often a mix—reduced fat reveals persistent gland. That’s why some men see a more prominent nipple-areola shape even after dropping body fat; the underlying gland becomes more noticeable.
Why It Happens: Hormones, Life Stages, and Triggers
Physiologic phases
• Newborns: Maternal estrogens can cause temporary gynecomastia, sometimes with small milk (“witch’s milk”). This resolves spontaneously within weeks.
• Puberty: Up to 50–60% of boys experience transient gynecomastia due to a temporary imbalance during hormonal surges. Most cases regress within 6–24 months.
• Aging: In older men, lower testosterone and higher aromatase activity in fat tissue increase the estrogen effect, making gynecomastia more common.
Medical conditions that tilt hormones
• Hypogonadism (low testosterone), including Klinefelter syndrome.
• Hyperthyroidism, liver disease (cirrhosis), chronic kidney disease, malnutrition/refeeding.
• Tumors that produce beta-hCG (e.g., certain testicular or germ-cell tumors) can stimulate estrogen production.Consult Top Specialists Here
Medications and substances linked to gynecomastia
• Antiandrogens (bicalutamide, flutamide), 5-alpha-reductase inhibitors (finasteride, dutasteride).
• Spironolactone, certain anti-ulcer drugs (cimetidine), some antipsychotics (notably risperidone), some antiretrovirals (efavirenz), ketoconazole, some calcium channel blockers.
• Anabolic-androgenic steroids (AAS) and improper post-cycle therapy can precipitate gynecomastia due to aromatisation of androgens to estrogens.
• Alcohol, opioids; cannabis association is debated and evidence is mixed.
Lifestyle and body fat’s role
• Increased body fat raises aromatase activity, converting more testosterone to estrogens in adipose tissue. Poor sleep, high stress, and heavy alcohol intake can also nudge hormones in the wrong direction.
If your condition does not improve after addressing potential triggers, book a physical visit to a doctor with Apollo 24|7 to review medications and underlying conditions. Apollo 24|7 also offers convenient home collection for tests like thyroid profile or testosterone when labs are indicated.
Unique insight: A “stack” of small contributors—modest weight gain, new medication, and short sleep—can add up. Fixing two of three may be enough to reverse early gynecomastia without further treatment.
Signs to Watch: Symptoms, Red Flags, and When to Worry
Typical symptoms
• A rubbery or firm disk of tissue centred under the nipple (one or both sides).
• Tenderness or sensitivity, more pronounced in early stages.
• Cosmetic changes: nipple puffiness or asymmetry.
Male breast cancer vs. gynecomastia
Male breast cancer is rare, but it happens. Red flags include:
• A hard, irregular, or immobile mass not centred under the nipple.
• Nipple retraction or inversion; skin dimpling.
• Nipple discharge (especially bloody).
• Enlarged, firm lymph nodes in the armpit; rapid growth; unilateral involvement.
Timeline and triggers to act on
• Puberty: If the enlargement is mild and not rapidly growing, monitoring for 6–12 months is reasonable. If it persists beyond 12–24 months, becomes painful, or grows quickly, seek medical review.
• Adults: If onset is recent, painful, or you started a new medication, discuss with your clinician. If a mass is hard, off-center, or associated with skin or nipple changes, seek evaluation promptly.
If symptoms persist beyond two weeks with concerning features, consult a doctor online with Apollo 24|7 for further evaluation. They can triage urgency and arrange an in-person assessment if needed.
Unique insight: Pain in early gynecomastia is common and often indicates active growth—which is exactly when reversible causes (medication changes, hormone issues) are most likely to help if addressed early.
How Doctors Diagnose Gynecomastia: Exams, Labs, and Imaging?
What to expect in the exam
• Your clinician will ask about timing, tenderness, medications, supplements (including bodybuilding agents), alcohol and substance use, weight changes, and sexual or fertility symptoms (libido, erectile function).
• Physical exam includes the breast tissue (checking symmetry, consistency, skin/nipple changes), testicular exam, thyroid exam, and signs of liver or kidney disease.
Lab tests (as needed)
• Not all patients need labs. If features suggest secondary causes or if gynecomastia is significant/persistent, common tests include:
• Total testosterone, LH, FSH (hypogonadism patterns)
• Estradiol
• Prolactin (if galactorrhea or pituitary concern)
• TSH/free T4 (thyroid)
• Liver function tests, creatinine
• Beta-hCG (if rapid progression or testicular tumour concern)
• Apollo 24|7 offers convenient home collection for many of these tests, which can speed up evaluation without extra clinic visits.
Imaging
• Breast ultrasound helps differentiate gland vs. fat and characterize masses when the exam is uncertain.
• Mammography may be used if cancer is suspected. Testicular ultrasound is ordered if a mass is suspected or if beta-hCG is elevated.
When genetic or testicular evaluation is needed
• Disproportionate breast growth with small, firm testes or infertility may suggest Klinefelter syndrome; genetic testing may be considered.
• Rapidly progressive gynecomastia with hormonal red flags warrants endocrinology or urology input.
Do You Need Treatment? From Watchful Waiting to Medication
Watchful waiting (when it’s reasonable)
• Pubertal gynecomastia often recedes within 6–24 months; reassurance plus periodic checks is appropriate if symptoms are mild and there are no red flags.
• Early adult cases linked to a new drug or weight gain may improve within months after addressing the trigger.
Treating underlying causes
• Review and adjust medications when possible (for example, alternatives to spironolactone or risperidone after a clinician’s assessment).
• Address thyroid, liver, kidney, or hormone disorders. Manage sleep, stress, and alcohol intake. Reduce body fat, which lowers aromatase activity.
Pain relief and mental health
• Short-term pain can be managed with simple analgesics if appropriate. Ice packs may help tenderness.
• Body image distress is common. Consider supportive clothing (compression undershirts), posture work, and counselling if self-esteem or social functioning is affected. Teens benefit from school accommodations for PE/swimming during sensitive periods.
Timelines for change
• If gynecomastia is improving over 3–6 months, continuing conservative measures is reasonable.
• If there’s no improvement, significant pain, or psychosocial impact after several months, discuss medical therapy or surgical options.
If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo 24|7 to review next-step treatments, including medication options or surgical referral.
Medicines for Gynecomastia: What Works and What Doesn’t
Selective estrogen receptor modulators (SERMs)
• Tamoxifen is the most studied option. Small randomised and observational studies suggest tamoxifen (often 10–20 mg/day) can reduce pain and breast size, particularly if started early (within 6–12 months of onset). It’s used off-label for this purpose; benefits often appear within weeks to a few months.
• Raloxifene (60 mg/day) has shown benefit in adolescents with persistent pubertal gynecomastia in small studies, improving size and symptoms.
Aromatase inhibitors and other agents
• Aromatase inhibitors (e.g., anastrozole) have mixed or limited benefit in gynecomastia; evidence is weaker than for SERMs, especially in pubertal cases.
• Danazol (a weak androgen) can shrink breast tissue but has more side effects and is used less commonly today.
Expectations and safety
• Medications work best for recent, tender gynecomastia. Long-standing fibrotic tissue is less responsive and may require surgery for optimal cosmetic results.
• Side effects of SERMs can include hot flashes, leg cramps, and rarely thromboembolic events; clinicians weigh risks vs benefits individually.
If gynecomastia is medication-induced, stopping the culprit drug (when safe) is often the most effective “treatment.”
If considering tamoxifen for gynecomastia, discuss timing, dosage, and duration with your clinician. If lab tests are needed before treatment (e.g., testosterone, estradiol, TSH), Apollo24|7 offers home collection to streamline your workup.
Unique insight: Think of SERMs as “window-of-opportunity” treatments—most helpful when tissue is still tender and active, less so once the gland becomes fibrous and stable.
Surgery for Gynecomastia: Techniques, Recovery, and Results
When surgery is considered
• Persistent gynecomastia >12 months with stable tissue, significant psychosocial distress, pain, or failure of medical therapy.
• Dense glandular tissue that won’t respond to weight loss or SERMs.
Techniques
• Liposuction removes excess fat via small incisions; useful for pseudogynecomastia and mixed cases with minimal gland.
• Subcutaneous gland excision removes firm breast tissue through an incision at the edge of the areola; often combined with liposuction for best contour.
• In more severe or skin-excess cases, skin tightening or staged procedures may be needed.
Recovery and outcomes
• Most men return to desk work in a few days and full activity in 2–4 weeks. Compression vests are common for 2–6 weeks to reduce swelling.
• Risks include hematoma, seroma, infection, contour irregularities, nipple sensation changes, and scarring; serious complications are uncommon in experienced hands.
• Satisfaction rates are high, especially when expectations are realistic and technique matches tissue type.
Choosing your surgeon
• Look for a board-certified plastic surgeon with specific experience in gynecomastia and a track record of before/after results.
• Ask about technique, scar placement, revision rates, and recovery timelines.
Related terms: gynecomastia surgery cost; male breast reduction recovery.
Unique insight: Technique matching matters. Dense gland under an otherwise lean chest often needs precise gland excision; relying on liposuction alone in such cases can under-treat the central prominence.
Living with Gynecomastia: Lifestyle, Teens, Athletes, and Mindset
Lifestyle steps that help
• Weight management: Reducing overall body fat can lessen chest fullness, decrease aromatase activity, and improve hormone balance. Focus on steady, sustainable loss (e.g., 0.25–0.5 kg/week) and protein-rich meals.
• Training: Prioritise full-body resistance training. Chest-focused workouts won’t “burn chest fat” but can improve posture and upper-body shape. Strengthen the back and shoulders to support a confident silhouette.
• Clothing hacks: Compression undershirts or structured fabrics can reduce visibility under shirts. Choose darker colours and avoid clingy thin materials if you feel self-conscious.
Pubertal gynecomastia: guidance for families
• Reassure teens that pubertal gynecomastia is common and usually temporary.
• Manage tenderness with simple measures; encourage posture and appropriate clothing choices during sports.
• If distress is severe, or if breast growth persists beyond two years, discuss medical options with a paediatrician or endocrinologist.
Steroids and testosterone therapy
• Anabolic steroid cycles and improper post-cycle therapy can trigger gynecomastia as androgens convert to estrogens. Prevention involves avoiding non-prescribed AAS and seeking medical guidance.
• On testosterone replacement therapy (TRT), aromatisation can lead to symptoms. Work with your clinician to optimise dosing, delivery method, and monitoring; do not self-medicate with anti-estrogens.
When to see a doctor (and what to ask)
• Rapid growth, pain, asymmetry, or red flags warrant evaluation. Ask about probable causes, needed tests, treatment options, and timelines. If scheduling is difficult, consult a doctor online with Apollo24|7 to get triaged and plan next steps.
Unique insight: Mindset upgrades—like reframing chest training goals from “spot reduction” to posture and strength—often yield faster visible wins and more confidence than chasing minor fat changes.
Costs, Access, and Finding Care You Trust
Costs and insurance basics
• Non-surgical care (evaluation, labs, medication trials) is typically covered in many systems. Surgery may be considered cosmetic by some insurers unless there’s documented pain, functional limitation, or psychological impact; policies vary by region.
• In India, costs for gynecomastia surgery vary widely based on city, surgeon experience, and facility level. Always request an itemised estimate covering surgeon’s fee, anaesthesia, facility, garments, and follow-ups.
How to choose evidence-based care
• Start with a primary clinician or endocrinologist to evaluate causes and reversible factors; a plastic surgeon can advise on procedure suitability if needed.
• Be cautious of aggressive marketing promises. Ask about evidence for medications, realistic outcomes, and complication rates.
If you’re unsure where to start, Apollo24|7 can help you book an online consultation, organise necessary labs via home collection, and coordinate referrals to qualified specialists.
Unique insight: A short period of structured evaluation (4–8 weeks) often yields clarity—whether it’s watchful waiting, a medication change, or a surgical consult—saving time and expense compared to going straight to the operating room.
Prevention, Outlook, and What Long-Term Health Looks Like
Prevention strategies
• Maintain a healthy weight and prioritise sleep (7–9 hours) to support hormone balance.
• Limit alcohol and avoid non-prescribed anabolic steroids or unverified supplements.
• Review medications with your clinician if you notice breast changes; ask if alternatives exist.
Outlook and recurrence
• Pubertal gynecomastia usually resolves. Adult cases related to reversible causes may improve once the trigger is addressed.
• After surgery, recurrence is uncommon if underlying hormonal issues are controlled; significant weight gain, medication changes, or steroid use can increase recurrence risk.
Long-term health
• Gynecomastia itself does not increase mortality risk. Focus on underlying health (metabolic, endocrine, liver, kidney) and mental well-being.
• If chronic distress persists, counselling can be as important as medical or surgical steps.
Unique insight: A “3-pillar” approach—optimise health habits, review meds, and set a clear timeline for re-evaluation—resolves uncertainty for most men within a few months.
Conclusion
Gynecomastia is more common than most people realise, and it’s usually a benign, manageable condition. Understanding the difference between true gynecomastia and pseudogynecomastia helps you choose the right path—whether that’s reassurance and lifestyle steps or a targeted medical/surgical plan. In teens, patience is often the best treatment, as pubertal gynecomastia typically fades within a year or two. In adults, reviewing medications, avoiding anabolic steroids, moderating alcohol, improving sleep, and reducing excess body fat can make a real difference. When needed, medications like tamoxifen for gynecomastia may ease pain and reduce size if started early. For persistent, fibrous tissue or significant distress, modern surgical techniques are safe, effective, and tailored to your anatomy and goals.Consult Top Specialists Here
Consult Top Specialists Here

Dr. Dhanraj K
General Physician/ Internal Medicine Specialist
25 Years • MBBS, MD Internal Medicine - Osmania Medical College, Hyderabad
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(400+ Patients)

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Bhargav Vuppumalla
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD GENERAL MEDICINE
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
Consult Top Specialists Here

Dr. Dhanraj K
General Physician/ Internal Medicine Specialist
25 Years • MBBS, MD Internal Medicine - Osmania Medical College, Hyderabad
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(400+ Patients)

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Bhargav Vuppumalla
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD GENERAL MEDICINE
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
Consult Top Specialists Here

Dr. Dhanraj K
General Physician/ Internal Medicine Specialist
25 Years • MBBS, MD Internal Medicine - Osmania Medical College, Hyderabad
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(400+ Patients)

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Bhargav Vuppumalla
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD GENERAL MEDICINE
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
More articles from gynaecomastia
Frequently Asked Questions
1. How long does pubertal gynecomastia last?
Most cases improve within 6–24 months. If it persists beyond two years or causes significant distress, ask about options like SERMs or a surgical consultation. Consider an online check-in with Apollo24|7 if you’re unsure.
2. Can I treat gynecomastia without surgery?
Yes, especially if it’s early. Address medications, reduce body fat, and consider SERMs like tamoxifen for gynecomastia when appropriate. Long-standing, firm tissue may need surgery for optimal cosmetic results.
3. Which drugs commonly cause gynecomastia?
Spironolactone, some antiandrogens, finasteride/dutasteride, certain antipsychotics (e.g., risperidone), cimetidine, ketoconazole, and some antiretrovirals (e.g., efavirenz). Review your list with a clinician.
4. How is male breast cancer different from gynecomastia?
Cancer often presents as a hard, irregular mass not centered under the nipple, with possible nipple retraction or discharge and enlarged armpit nodes. If you notice these, seek urgent evaluation.
5. What does gynecomastia surgery recovery look like?
Most return to light activity in a few days, full workouts in 2–4 weeks. You’ll likely wear a compression vest for several weeks. Swelling subsides over months; final results can take 3–6 months.