Acyanotic Heart Disease
Discover everything about acyanotic heart disease, its causes, symptoms, diagnosis, and treatment options. Learn how timely intervention and modern advancements ensure a better quality of life for individuals with this condition.

Written by Dr Shreya Sarkar
Last updated on 3rd Jul, 2025
Congenital heart diseases (CHDs) structural defects in the heart present since the time of birth. They are one of the most common birth defects, affecting about 1 in 100 newborns worldwide. These defects can be small or serious and affect how blood flows through the body.
Some cases do not cause serious problems, but others need medical care to support a child’s healthy growth. Early diagnosis and modern treatments have significantly improved survival rates and quality of life for affected children.
Primarily, CHDs are grouped into two types: acyanotic and cyanotic.
Acyanotic heart diseases: Do not lower oxygen levels in the blood.
Cyanotic heart diseases: Cause low oxygen levels, often leading to blue-tinted skin.
Acyanotic defects are less urgent but still require treatment to avoid complications. However, cyanotic defects typically need immediate care.
Common Types of Acyanotic Heart Disease
Several types of acyanotic heart diseases are found in individuals. Here are the most commonly diagnosed:
Ventricular Septal Defect (VSD)
A ventricular septal defect (VSD) refers to a heart defect which constitutes a hole in the wall between the heart’s lower chambers. This allows extra blood to flow to the lungs, making the heart work harder.
Small VSDs often close on their own. However, larger defects may require surgery to prevent problems like heart failure or lung damage.
Atrial Septal Defect (ASD)
An atrial septal defect (ASD) refers to a defect where there is a hole in the wall between the heart’s upper chambers. This allows oxygen-rich and oxygen-poor blood to mix, which can strain the heart.
Untreated ASD can lead to irregular heartbeats or stroke. However, minimally invasive procedures now make repairs safer and recovery faster.
Patent Ductus Arteriosus (PDA)
The ductus arteriosus is a fetal blood vessel that closes after birth. If it stays open (PDA), it can send too much blood to the lungs and strain the heart.
Treatment can include medicine to close the vessel or surgery for more severe cases. Detecting PDA early helps avoid serious complications.
Atrioventricular Septal Defect (AVSD)
Atrioventricular septal defect (AVSD) stands as a heart defect which affects the heart’s walls and valves. It changes how blood flows and can lower oxygen delivery to the body.
AVSD is often linked to genetic conditions like Down syndrome. In order to fix this type of CHD, surgery during infancy is usually needed, which prevents other complications such as lung disease.
Causes and Risk Factors
When it comes to acyanotic heart disease, there are certain risk factors that play a key role.
Genetic risk factors
Certain genetic disorders, like Down syndrome, increase the risk of AHD. Heart defects can also run in families, showing a hereditary link.
Research is helping identify genetic mutations tied to AHDs, improving prenatal testing and creating possibilities for targeted treatments.
Environmental risk factors
Maternal health, exposure to harmful substances, and some medications during pregnancy can raise the risk of AHDs.
Good prenatal care, including proper nutrition and avoiding harmful exposures, helps reduce these risks. Pregnant individuals should work closely with healthcare providers to monitor their health and learn more about how to lead a healthy lifestyle.
Pathophysiology of Acyanotic Heart Disease
Acyanotic heart defects usually cause blood to flow from the left side of the heart to the right. This increases blood flow to the lungs and makes the heart work harder. If untreated, these changes can also lead to complications like lung congestion or heart enlargement.
In addition to this, a prolonged time period with untreated defects can weaken the heart and reduce its ability to pump blood effectively. Pulmonary hypertension is another possible complication which is often diagnosed in patients.
Understanding these effects has helped doctors create better treatments to manage symptoms and delay disease progression, leading to positive outcomes.
Symptoms and Signs
While being a commonly found defect since the time of birth, congenital heart defects can sometimes go unnoticed. Here are some of the signs and symptoms based on the age of individuals who potentially can be at risk of AHD.
Common symptoms in infants and children
Trouble breathing or feeding
Poor weight gain
Frequent lung infections
Recognising these signs early allows for prompt treatment, improving long-term health outcomes.
Symptoms in adults
Shortness of breath
Fatigue during normal activities
Irregular heartbeat
Adults with untreated defects may experience these symptoms. The best way to have them diagnosed is by getting regular heart checkups. These checkups are specifically essential if the family has a long history of heart issues.
Consult Top Cardiologists for Personalised Care
Diagnosis of Acyanotic Heart Disease
Acyanotic heart disease can be diagnosed in several ways. Doctors often notice heart murmurs during checkups, which can signal a defect. Under such conditions, gathering a full family and medical history provides important clues.
However, to get a better picture of the disease and its types, there are various tools that are used by medical professionals.
Echocardiograms
X-rays
MRIs
Cardiac catheterisation
New imaging tools like 3D echocardiography offer even more precise diagnoses, improving treatment planning.
Treatment Options
Medications like diuretics can help reduce symptoms, whereas beta-blockers may also be used to manage complications when treating AHD. Additionally, sometimes antibiotics are also given to prevent infections in diagnosed individuals.
Besides treatment options prescribed by medical professionals, lifestyle adjustments are significant to better tackle AHD. Healthy eating, exercise, routine checkups and a lifestyle that supports a healthy heart are some of the ways AHD can be managed better.
Surgical interventions
Surgery corrects structural defects and restores normal blood flow in AHD patients. Minimally invasive techniques are becoming more common, offering faster recovery and fewer risks. After the conclusion of surgery, ongoing follow-up care ensures long-term success, including regular monitoring and tailored rehab programs.
Complications and Long-Term Outlook
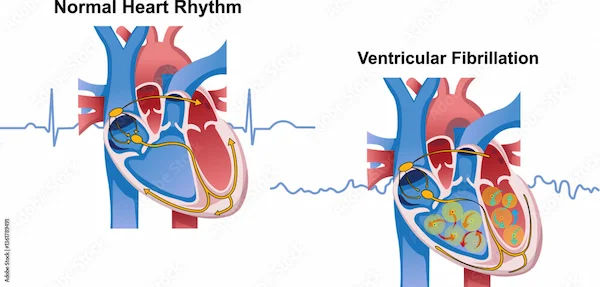
Since AHD is a serious condition, without treatment, acyanotic heart defects can lead to problems like heart failure or lung disease. Some people may develop arrhythmias (irregular heartbeat) or high blood pressure in the lungs. Therefore, general awareness of AHD, its symptoms and treatment is very important to successfully curb its potential harm.
With proper medical assistance, most individuals with acyanotic heart disease live full, active lives after treatment. Since new techniques and treatments are making recovery easier and outcomes better than ever, knowing all likely options is important to stay hopeful!
Living with Acyanotic Heart Disease
Living with acyanotic heart disease requires compliance with an array of health-favoured practices:
Balanced diet
Regular, moderate exercise
Avoiding tobacco and managing stress
In addition to this, regular checkups are also essential since they work as a tool to spot issues early. While medications and medical assistance are essential, people should also understand the significance of psychosocial support. Therefore, if you know someone who is suffering from AHD, undergoing its treatment, or has successfully tackled it, ensure providing moral support. Support groups also offer great assistance under such circumstances.
Conclusion
Acyanotic heart diseases are manageable with timely care since, fortunately, medical advances have greatly improved patients' outcomes and quality of life. While different types of AHD bring varying levels of defects to a human heart, evolved medical assistance today has the ability to heal it effectively.
The best way to manage AHD is early intervention, which prevents complications and supports healthy living. Thankfully, continued research is creating even better possibilities for the future, making sure that patients can successfully defeat it.
Consult Top Cardiologists
Consult Top Cardiologists for Personalised Care

Dr. Amit. A. Bharadiya
Cardiologist
12 Years • MBBS, MD General Medicine, DNB Cardiology, FSCAI
Maharashtra
Surabhi Hospital, Maharashtra, Maharashtra

Dr. S B Bhattacharyya
Cardiologist
22 Years • MBBS, MD(General Medicine),DM (Cardiology)
Kolkata
Gariaheart Clinic, Kolkata
Dr. Jayarajah Mariappan
Cardiologist
45 Years • MBBS, MD(GEN MEDICINE), DM(CARDIOLOGY)
Chennai
Sooriya Hospital, Chennai

Dr. Sumanta Chatterjee
Cardiologist
12 Years • MBBS,MD General Medicine,DM Cardiology
Kolkata
HealthYou Speciality Clinic & Diagnostics., Kolkata
(25+ Patients)

Dr. Mangesh Danej
Cardiologist
8 Years • MBBS, MD (General Medicine), DNB (Cardiology)
Pune
Dr Danej clinic, Pune
(375+ Patients)
Consult Top Cardiologists

Dr. Amit. A. Bharadiya
Cardiologist
12 Years • MBBS, MD General Medicine, DNB Cardiology, FSCAI
Maharashtra
Surabhi Hospital, Maharashtra, Maharashtra

Dr. S B Bhattacharyya
Cardiologist
22 Years • MBBS, MD(General Medicine),DM (Cardiology)
Kolkata
Gariaheart Clinic, Kolkata
Dr. Jayarajah Mariappan
Cardiologist
45 Years • MBBS, MD(GEN MEDICINE), DM(CARDIOLOGY)
Chennai
Sooriya Hospital, Chennai

Dr. Sumanta Chatterjee
Cardiologist
12 Years • MBBS,MD General Medicine,DM Cardiology
Kolkata
HealthYou Speciality Clinic & Diagnostics., Kolkata
(25+ Patients)

Dr. Mangesh Danej
Cardiologist
8 Years • MBBS, MD (General Medicine), DNB (Cardiology)
Pune
Dr Danej clinic, Pune
(375+ Patients)