Myths of Hepatitis
Debunk common myths about hepatitis and learn the facts about its causes, transmission, symptoms, prevention, and treatment. Stay informed to protect yourself and others from this global health concern.

Written by Dr.Sonia Bhatt
Last updated on 13th Jan, 2026
.webp?tr=q-80,f-webp,w-350,dpr-2,c-at_max 700w)
Hepatitis refers to inflammation of the liver, most commonly caused by a viral infection or excessive alcohol consumption. It can also result from exposure to toxins, the use of certain drugs, or underlying conditions, such as autoimmune diseases. There are five primary types of hepatitis: A, B, C, D, and E, with hepatitis B and C being the most prevalent ones. Without timely treatment, hepatitis can lead to complications such as liver fibrosis (scarring), cirrhosis, or even liver cancer.
The term "hepatitis" is derived from the Greek word "hepar," meaning liver, combined with the suffix "-itis," which signifies inflammation. The first documented case of infectious hepatitis dates back to the 19th century when outbreaks were linked to contaminated water supplies. Advances in medical science over the years have led to the development of antiviral treatments, significantly improving survival rates and quality of life for those with chronic hepatitis.
Common Myths and Misconceptions linked with hepatitis
Dispelling myths about hepatitis is essential to improve public understanding and promote its prevention and management. Misunderstandings about the condition often fuel stigma and discrimination against those affected.
1. Myth: Hepatitis Is Always Caused by Alcohol
While heavy alcohol consumption can contribute to chronic liver disease, it is not the sole cause of hepatitis. The condition can also result from viral infections, such as hepatitis A, B, C, D, and E, which are spread through contaminated food, water, blood, or bodily fluids.
For those with hepatitis, it is generally advisable to limit alcohol intake to protect the liver. In some cases, small amounts may be safe, depending on the level of liver damage, but reducing alcohol consumption is recommended even if the liver is unaffected. Understanding the various causes of hepatitis is vital for effective prevention and management.
2. Myth: Vaccination Is Not Necessary
Vaccination is a vital tool in preventing certain types of hepatitis and curbing the spread of these infections. Effective vaccines are available for hepatitis A and B and are strongly recommended for individuals at higher risk, such as healthcare professionals, travellers to high-risk areas, and those with specific medical conditions.
Hepatitis A: A safe and effective vaccine is available and It is advised for people at greater risk, including travellers to regions with high infection rates and those with certain health conditions.
Hepatitis B: The hepatitis B vaccine, introduced in the 1980s, is routinely administered to newborns and recommended for adults at risk of exposure.
Hepatitis C: Unfortunately, there is currently no vaccine for hepatitis C, although research is ongoing.
Hepatitis D: As hepatitis D only occurs in individuals already infected with hepatitis B, vaccinating against hepatitis B can prevent co-infection.
Hepatitis E: While no widely available vaccine exists for hepatitis E, practising good hygiene and consuming safe food and water can help minimise the risk.
Although there is no single vaccine to protect against all forms of hepatitis, the vaccines for hepatitis A and B are highly effective and have significantly reduced infection rates in many populations.
3. Myth: Only Drug Users Get Hepatitis
While high-risk behaviours, such as intravenous drug use and unprotected sex, can increase the risk of contracting hepatitis B and C, the disease is not limited to drug users. Hepatitis can affect anyone, as different types are transmitted in various ways.
Hepatitis A and E: These are typically spread through consuming contaminated food or water, meaning they can be contracted by anyone, particularly in areas with poor sanitation or limited access to clean water.
Hepatitis B and D: These are primarily transmitted through blood-to-blood contact, unprotected sex, sharing needles, or from an infected mother to her baby during childbirth.
Hepatitis C: The most common transmission route for hepatitis C is blood-to-blood contact, often through sharing needles or unsterilised medical equipment.
While certain behaviours may increase the risk of hepatitis, the infection can occur through other routes as well. Understanding these diverse transmission methods is important in reducing stigma and improving prevention efforts.
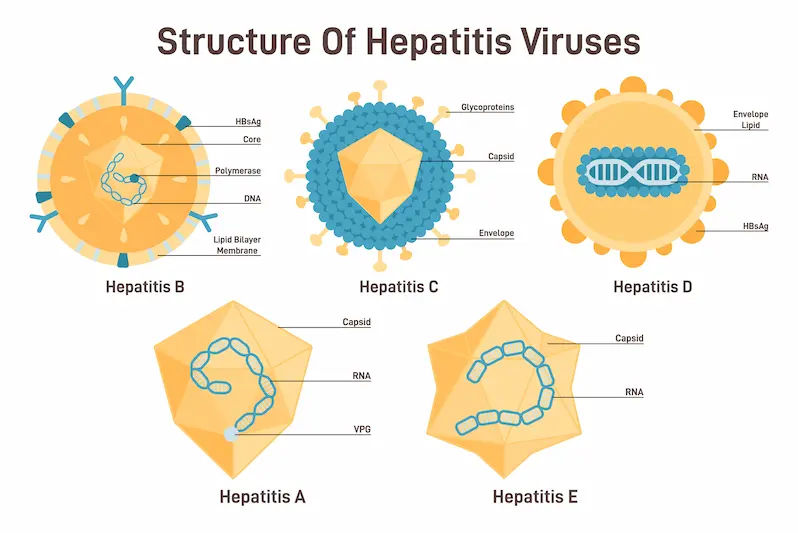
Types of Hepatitis
There are five primary types of hepatitis viruses: A, B, C, D, and E. Each type has different modes of transmission, symptoms, and potential long-term effects.
Hepatitis A: Usually transmitted through contaminated food or water, hepatitis A causes a short-term infection that typically does not result in chronic liver disease.
Hepatitis B: Unlike hepatitis A, hepatitis B can lead to both acute and chronic infections. If left untreated, it can cause severe liver damage. It is primarily spread through contact with infected blood or bodily fluids.
Hepatitis C: Hepatitis C is most commonly spread through blood-to-blood contact, such as sharing needles or receiving contaminated blood transfusions. It can cause chronic liver disease and, if untreated, may lead to cirrhosis or liver cancer.
Hepatitis D: This type only affects individuals already infected with hepatitis B. It can exacerbate the symptoms and increase the risk of serious liver complications.
Hepatitis E: Hepatitis E is transmitted through contaminated food or water, much like hepatitis A. It usually resolves on its own but can be particularly dangerous for pregnant women.
While hepatitis A and E tend to cause temporary infections, hepatitis B, C, and D can lead to chronic liver conditions, with hepatitis D being the most severe form.
Symptoms of Hepatitis
Hepatitis can cause a range of symptoms, varying in severity depending on the type of hepatitis and the extent of liver damage. Common symptoms include:
Malaise
Abdominal tenderness, especially in the upper right side
Fatigue
Jaundice
Dark-coloured urine
Pale or light-coloured stools
Abdominal pain
Nausea, with or without vomiting
Abdominal swelling due to fluid retention
Diagnosis of Hepatitis
To diagnose hepatitis, your doctor will start by asking questions to assess your risk for the various types of viral hepatitis. These questions may include whether you:
Work in a healthcare setting, such as a medical laboratory or dialysis unit
Have a family member (parent, sibling, or child) with hepatitis
Engage in unprotected sex or have a sexual partner with hepatitis B or C
Use intravenous drugs
Live in or are exposed to unsanitary conditions
Consume potentially contaminated food or water
Handle or eat raw shellfish
Your doctor will then conduct a physical examination, paying close attention to your abdomen to check for any enlargement or tenderness in the liver or spleen. Blood tests will be carried out to assess liver function and to detect antibodies specific to the various hepatitis viruses. A urine test may also be performed.
If chronic hepatitis is suspected, particularly with hepatitis C, a liver biopsy may be required. This procedure, which is performed under general anaesthesia, helps to assess the degree of liver damage, which can occur even in the absence of symptoms.
Get Tested for Hepatitis
Treatment and Management of Hepatitis
Treatment and management of hepatitis depend on the type and severity of the condition.
1. Acute Hepatitis
The main objectives for treating acute viral hepatitis include:
Ensuring adequate nutrition and hydration
Preventing further liver damage by avoiding alcohol and following other preventive measures
Reducing the risk of spreading the virus to others
There are no specific antiviral medications for treating acute hepatitis, though your doctor may recommend medications to relieve certain symptoms. Most cases of acute hepatitis are mild, and hospitalisation is generally only required for individuals at higher risk of complications, such as pregnant women, the elderly, those with serious underlying health conditions, or people who become dehydrated due to nausea and vomiting. In very rare instances, acute hepatitis can lead to liver failure (fulminant acute hepatitis), which may require a liver transplant.
2. Chronic Hepatitis
The goals of treating chronic viral hepatitis are:
Preserving liver function and preventing further liver damage
Enhancing the immune system to help control the virus
Your doctor may prescribe various medications to manage chronic hepatitis. Many people also use complementary and alternative medicine (CAM) therapies to strengthen their immune system and alleviate fatigue, such as herbal supplements, vitamins, homoeopathy, acupuncture, and massage therapy. It is important to inform all your healthcare providers about your hepatitis diagnosis so they can take the necessary precautions to prevent transmission of the virus.
Measures to Prevent Hepatitis
Taking proper precautions is essential to prevent the transmission of hepatitis and protect both yourself and others. By following these simple guidelines, you can significantly reduce the risk of infection.
Wash clothes in hot water and disinfect surfaces to prevent transmission.
Use condoms and avoid sharing personal items.
Handle blood-contaminated items with care.
Avoid contaminated food and water.
Wash hands after using the toilet, changing diapers, or preparing food.
Clean thoroughly after contact with bodily fluids from an infected individual.
Individuals with hepatitis should not prepare food for others.
At-risk individuals should receive the appropriate hepatitis vaccine.
Avoid contact with blood and blood products.
Do not use intravenous drugs or share needles.
Limit sexual partners and practise safe sex.
Ensure sterile needles are used in tattoo and piercing parlours.
Healthcare workers should follow universal precautions.
Children should receive the appropriate hepatitis vaccine.
Avoid sharing personal items like razors or toothbrushes.
Immunisation
Hepatitis A: Recommended for individuals in high-risk areas, frequent travellers, healthcare workers, men who have sex with men, and those in close contact with infected individuals.
Hepatitis B: Vaccination is advised for high-risk groups, including healthcare workers, individuals with multiple sexual partners, travellers to high-risk regions, and those with weakened immune systems.
Hepatitis C: Currently, there is no effective vaccine for hepatitis C, and the most reliable way to prevent the disease is to avoid exposure to the virus. Special precautions should be taken in healthcare environments and for individuals who are at greater risk of hepatitis C infection including people who inject drugs, men who have sex with men, and individuals living with HIV.
Global Impact of Hepatitis
Viral hepatitis affects more than 300 million people globally, causing over 1 million deaths annually. Despite the availability of vaccines, prevention measures, and treatments, the number of hepatitis-related deaths continues to rise worldwide.
The World Health Organization (WHO), the CDC, and other international bodies recognise World Hepatitis Day (WHD) on 28 July to raise awareness about viral hepatitis. This day draws attention to the difficulties faced by those living with hepatitis, ongoing efforts to tackle the disease, and preventive actions to reduce its transmission. Furthermore, the CDC collaborates with global partners to support countries with high infection rates in their efforts to prevent, control, and ultimately eliminate viral hepatitis.
Conclusion
Misinformation surrounding hepatitis can fuel stigma and discrimination, discouraging individuals from getting diagnosed and treated. This not only compromises personal health but also increases the risk of spreading the virus within communities. Public health campaigns must prioritise educating the public, encouraging vaccination, and promoting regular health check-ups.
Clearing up common misconceptions about hepatitis is vital to ensure an accurate understanding of the virus. It is important for people to be aware of the different types of hepatitis, how they spread, and the available prevention methods in order to effectively address this global health concern.
Consult Top Hepatologists
Consult Top Hepatologists

Dr. Swapnil Mujawdiya
Gastroenterology/gi Medicine Specialist
7 Years • MBBS, MD (Medicine), DM, Gastroenterology, SGPGI (Lucknow).
Indore
Apollo Hospitals Vijay Nagar, Indore

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr U V U Vamsidhar Reddy
Hepatologist
10 Years • MBBS, MD (JIPMER), DM (Hepatology, PGIMER)
Chennai
Apollo Hospitals Greams Road, Chennai
(75+ Patients)

Dr. Kumaragurubaran. S
Hepatologist
0 Years • MBBS.,MD.,FPIC.,DM.,
Tiruchirappalli
Apollo Speciality Hospitals Old Palpannai, Tiruchirappalli
(50+ Patients)

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar