What Leads To Signs Of Hernia Definition Treatment
Learn everything about hernias — their definition, causes, symptoms, and treatment options. Understand when to seek help, how surgery compares to watchful waiting, and practical recovery tips.

Written by Dr. M L Ezhilarasan
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Introduction
A hernia can be both worrying and confusing: you might notice a small lump that comes and goes, feel a pulling or burning sensation when you lift something, or develop heartburn and chest discomfort after meals. But what exactly is a hernia, what leads to the signs you’re noticing, and how is it treated? In this comprehensive guide, we break down the hernia definition in simple terms, explain how and why hernias form, outline the most common types, and show you how to spot red flags that require urgent care. We also walk through proven treatment options—from watchful waiting to modern surgical repair—plus recovery, prevention, and special situations for women, children, and those who’ve had prior surgeries. Whether you’re worried about a new lump, wondering if your symptoms match a hiatal hernia, or planning a return to sport after repair, this article gives you evidence-based answers and practical next steps. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation.
What is a hernia?
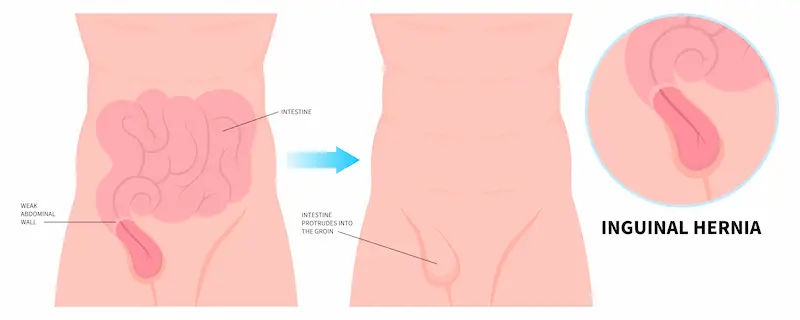
A hernia is a bulge that occurs when an internal organ or tissue pushes through a weak spot or opening in the muscle or connective tissue that normally holds it in place. In the abdomen, this is typically a section of intestine or fatty tissue pushing through the abdominal wall or groin. Think of the abdominal wall like a layered net: if one area becomes thin or stretched, pressure from inside can push tissue outward, creating a lump you may see or feel—especially when standing, coughing, or lifting.
Common places hernias occur
- Groin (inguinal and femoral): the most common, especially in men for inguinal hernias and in women for femoral hernias.
- Navel (umbilical): often seen in infants and in adults who are overweight or post-pregnancy.
- Upper midline (epigastric): small defects along the midline above the navel.
- Incisional: along a previous surgical scar where healing created a weaker spot.
- Hiatal: the stomach pushes up through the diaphragm into the chest, often causing reflux-like symptoms rather than a visible bulge.
Consult Top Specialists Here
How and Why a Hernia Forms
Here’s how and why hernias develop:
Abdominal wall anatomy and weak points
The abdominal wall is built from muscle layers, fascia (tough connective tissue), and natural passageways (like the inguinal canal). Weak points can be congenital (present at birth) or acquired over time due to stretching or injury. Prior incisions create scars with altered collagen, which can be less resilient than unscarred tissue—one reason incisional hernias occur months to years after surgery.
Triggers that raise pressure
Hernias form and enlarge when internal pressure repeatedly pushes on a vulnerable area:
- Heavy lifting or sudden exertion
- Chronic coughing (e.g., from smoking or asthma)
- Constipation or straining during bowel movements or urination (e.g., prostate enlargement)
- Pregnancy and rapid weight gain
- Persistent vomiting or abdominal bloating
Over time, these forces can convert a tiny defect into a noticeable protrusion. Addressing these pressure sources is key to both prevention and recovery.
Types of Hernia and What They Mean
Here’s what different types of hernia mean:
Inguinal vs femoral
- Inguinal hernias account for the majority of groin hernias, more common in people assigned male at birth due to the pathway the testicles take before birth. They present as a groin lump that may extend into the scrotum, often tender with coughing or lifting.
- Femoral hernias appear just below the groin crease, more common in women, and have a higher risk of becoming trapped (incarcerated) or strangulated due to the narrow femoral canal.
Umbilical and epigastric
- Umbilical hernias occur at or near the navel. In infants they often close spontaneously by age 4–5; in adults, they’re associated with obesity and pregnancy.
- Epigastric hernias occur along the midline above the navel, typically small but can be tender.
Hiatal and paraesophageal
- Sliding hiatal hernia is common and often accompanies gastroesophageal reflux disease (GERD), causing heartburn, regurgitation, and chest discomfort.
- Paraesophageal hernia is less common but more concerning—part of the stomach sits next to the oesophagus and can twist or get trapped, requiring closer monitoring or surgery.
Incisional and other less common types
- Incisional hernias arise along prior abdominal incisions.
- Less common types include Spigelian (lateral abdominal wall) and obturator hernias (inner thigh pain).
Sports hernia (athletic pubalgia): a special case
Despite the name, a sports hernia isn’t a true hernia. It’s a strain or tear of soft tissues in the lower abdomen/groin from high-intensity sports. It causes groin pain without a visible lump. Treatment is usually rest, physiotherapy, and sometimes surgery, and it’s best evaluated by a sports medicine or general surgeon familiar with athletic injuries.
Signs and Symptoms: What to Watch For
Here’s how to recognise hernia symptoms:
Typical hernia symptoms by type
- Groin/abdominal wall hernias: a soft lump that enlarges when standing, coughing, or straining and flattens when lying down; aching or burning at the site; a “dragging” sensation. Inguinal hernias can cause scrotal swelling; femoral hernias may present as a small tender bump below the crease.
- Umbilical/epigastric: bulge at or above the navel, tenderness with exertion or after meals.
- Hiatal: heartburn, regurgitation, difficulty swallowing, chest or upper abdominal pain, anaemia from small bleeds; less often a visible sign.
Red flags and emergencies
Seek urgent care if you notice:
- Sudden, constant pain at the hernia site
- A bulge that becomes firm, tender, and cannot be pushed back in (incarceration)
- Nausea, vomiting, abdominal distension, or inability to pass gas or stool (possible bowel obstruction)
- Fever or skin redness over the bulge
These can indicate strangulation—compromised blood flow to trapped tissue—which is a surgical emergency. If these symptoms appear, go to the nearest emergency department immediately.
What does a hernia feel like day-to-day?
Many people describe a tugging, heavy, or burning sensation that worsens late in the day, with lifting, or after prolonged standing. Pain is often intermittent early on and may improve with rest or lying down. Over months to years, symptoms can slowly progress as the opening widens.
If your hernia-related discomfort or lump persists beyond two weeks or interferes with work or exercise, consult a doctor online with Apollo 24|7 to discuss evaluation and next steps.
Causes and Risk Factors You Can Change
Here’s what increases your hernia risk and what you can control:
Lifestyle and occupational risks
- Repetitive heavy lifting, especially without proper technique
- Chronic cough (smoking, COPD), sneezing (allergies), or throat clearing
- Straining due to constipation; low-fibre diets
- Obesity (increases abdominal pressure and impairs tissue quality)
- Intense core or high-impact sports without balanced conditioning
Addressing these improves comfort whether you choose watchful waiting or surgery.
Medical conditions and family history
- Connective tissue disorders and family history may predispose to hernias.
- Prostate enlargement can cause straining; treating it can reduce groin pressure.
- Poorly controlled diabetes can impair healing after repair.
Pregnancy and postpartum considerations
Pregnancy stretches the abdominal wall and can reveal or worsen umbilical or inguinal hernias. Many remain small and painless; timing of repair depends on symptoms and family planning. Pelvic floor and core rehab postpartum can help function and symptom control—discuss with your clinician.
When to See a Doctor and How Hernias Are Diagnosed
Here’s how doctors confirm a hernia diagnosis:
The physical exam and “reducible” vs “incarcerated”
A clinician looks and palpates the area while you cough or strain, assesses size, tenderness, and whether the bulge can be gently pushed back in (reduced). A reducible hernia is often managed electively; a non-reducible, painful hernia raises concern for incarceration or strangulation and needs urgent assessment.
Imaging: ultrasound, CT, and MRI—when they help
- Ultrasound is often first-line for groin hernias and can show dynamic protrusion with Valsalva; it’s helpful when the exam is inconclusive, especially in women and athletes.
- CT scans are useful for complex or incisional hernias, or when bowel obstruction is suspected.
- MRI can clarify occult or sports-related groin pain when ultrasound is negative.
Hiatal hernias are often diagnosed with endoscopy or imaging if reflux symptoms persist.
Lab tests and pre-op fitness
While hernias are diagnosed clinically, preoperative labs (blood count, glucose/HbA1c, kidney function) assess fitness for anaesthesia and healing. Apollo 24|7 offers convenient home collection for tests like HbA1c and vitamin D if your clinician recommends optimising these before elective surgery.
Treatment Options: From Watchful Waiting to Surgery
Here’s how hernias are treated:
Who can safely watch and wait? What the evidence says
For some minimally symptomatic inguinal hernias, watchful waiting is reasonable. A landmark randomised trial found that watchful waiting was safe over several years, with a low annual risk of acute incarceration; many participants eventually chose surgery as symptoms progressed, but emergency events were uncommon.
Open, laparoscopic, and robotic repair—pros and cons
- Open mesh repair: a small incision over the hernia; durable and widely available, often with local or regional anaesthesia.
- Laparoscopic repair: several tiny incisions, mesh placed from the inside; typically less early pain and quicker return to activities, with similar long-term recurrence when done by experienced surgeons.
- Robotic repair: similar to laparoscopic, may offer technical advantages for complex or incisional hernias; outcomes depend more on surgeon expertise than the robot itself.
For hiatal hernias causing refractory reflux or paraesophageal hernias, surgical options repair the hiatus and may include anti-reflux procedures after thorough evaluation.
Mesh vs no mesh: safety, recurrence, and myths
Modern mesh-based repairs reduce recurrence compared with tissue-only repairs in many hernia types, especially larger defects. Mesh complications (chronic pain, infection) are uncommon overall, and careful technique and patient selection reduce risks. Tissue-only repairs may be considered for small hernias, certain athletes, or when mesh is contraindicated. Discuss your goals and concerns openly with your surgeon.
Non-surgical relief tips that can help symptoms
- Activity modification: avoid heavy lifting or learn safe techniques.
- Manage cough, allergies, and constipation (fibre 25–35 g/day, fluids).
- A properly fitted support garment (truss) can reduce discomfort temporarily for some groin hernias, but it’s not a cure and should be supervised by a clinician to avoid harm.
- For hiatal hernias/GERD: smaller meals, avoid late-night eating, elevate the head of the bed, and consider physician-guided acid suppression.
If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo 24|7.
Recovery, Complications, and Long-Term Outlook
Here’s what to expect after hernia repair:
Recovery timeline and activity guidelines
After uncomplicated groin hernia repair, many return to desk work within 3–7 days and light exercise in 1–2 weeks; heavier lifting may resume in 4–6 weeks, guided by your surgeon. Laparoscopic approaches often allow faster early recovery. Pain control often relies on non-opioid strategies (paracetamol, NSAIDs if appropriate), ice, and early walking.
Recurrence and chronic pain: what to expect
Recurrence rates vary by hernia type, size, and technique; mesh repairs generally reduce recurrence compared with non-mesh in many cases. A small percentage develop chronic groin pain after repair; risk is minimised with nerve-sparing techniques, careful mesh placement, and tailored procedures. If persistent pain affects daily life, consider a surgeon experienced in chronic post-hernia pain for evaluation.
When things go wrong: incarceration and strangulation
Complications include incarceration (stuck hernia) and strangulation (compromised blood flow). These present with a tender, irreducible bulge, often with nausea or vomiting and systemic symptoms. Prompt surgical care is critical to prevent bowel damage.
Prevention: Protecting Your Core for the Long Run
Here’s how to prevent hernias and maintain core health:
Safe lifting and core conditioning
- Use hip and leg power; keep loads close to the body; exhale during exertion.
- Build a resilient core with training that balances strength and pressure control (diaphragmatic breathing, pelvic floor engagement, and gradual load).
Weight, cough, and constipation control
- Achieve and maintain a healthy weight to reduce abdominal pressure.
- Treat chronic cough; stop smoking to improve tissue quality and healing.
- Prevent straining with a fibre-rich diet, hydration, and, if needed, stool softeners.
Workplace and sport adjustments
Use mechanical aids, rotate tasks, and space high-intensity training to allow recovery. Athletes should integrate cross-training and mobility to reduce groin strain risk—especially in sports with rapid change of direction.
Special Situations
Here’s what to know about hernias in unique cases:
Hernias in women—why they’re often missed
Women are more likely to have femoral hernias, which can be subtle but carry a higher risk of complications. Groin pain without a clear bulge, especially below the inguinal ligament, deserves careful evaluation with ultrasound or MRI if needed.
Children and infants—most common types and timing
- Umbilical hernias often close on their own by age 4–5; surgery is considered if they persist, enlarge, or cause symptoms.
- Inguinal hernias in children don’t resolve spontaneously and are usually repaired to avoid incarceration. If your child has a persistent bulge or discomfort, seek paediatric evaluation promptly.
After abdominal surgery—incisional hernias
These can appear months to years later. Weight management, control of diabetes, and avoiding smoking reduce risk. For large or complex incisional hernias, specialised abdominal wall reconstruction techniques can restore function; surgeon experience is especially important.
Myths, Facts, and Frequently Misunderstood Points
Here’s the truth about common hernia myths:
Can a hernia heal itself?
Abdominal wall hernias in adults rarely, if ever, heal on their own. Symptoms may fluctuate, but the defect generally persists. Hiatal hernia symptoms can improve with lifestyle and medication, but the anatomical hernia usually remains.
Belts and trusses: do they work?
A well-fitted truss can temporarily reduce symptoms in selected groin hernias when surgery is delayed or contraindicated, but it doesn’t fix the hernia and can cause skin problems or pressure injury if misused. Always get fitted under clinical guidance.
Is every hernia an emergency?
No. Many hernias are managed electively based on symptoms and risk. However, a painful, irreducible bulge, vomiting, or bowel obstruction symptoms require immediate care to prevent strangulation.
Conclusion
Hernias are common and, for many people, manageable when you understand what they are and what leads to the signs you notice—whether that’s a groin lump after lifting, a navel bulge after pregnancy, or heartburn from a hiatal hernia. Most hernias are not emergencies, but knowing the red flags can protect you from serious complications. Effective treatment is highly individualised: some people do well with watchful waiting and lifestyle changes, while others benefit from timely surgical repair to relieve pain and prevent progression. Modern techniques—especially when matched to the right hernia type and surgeon experience—offer excellent outcomes and quick returns to normal life. If you’re unsure whether your symptoms need attention, or if you’re weighing surgery versus conservative measures, don’t wait. Start with an online consult through Apollo 24|7 to get personalised advice, arrange imaging or lab tests if needed, and plan next steps with confidence. Your core health is central to daily comfort—take the next step today.
Consult Top Specialists Here
Consult Top Specialists Here

Dr. Kunal Kumar Mehar
Urologist
10 Years • Mbbs, Ms, Mch
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr Sriharsha Ajjur
Urologist
10 Years • MBBS,MS,Mch
Bengaluru
Apollo Hospitals Jayanagar, Bengaluru

Dr. Duraisamy S
Urologist
38 Years • MBBS, MS (General Surgery), Mch (Urology)
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)
Dr. Mohamad Ali
Urologist
1 Years • MBBS, MS General Surgery, M Ch Urology
Pune
Apollo Hospitals Pune, Pune

Dr Karthik Maripeddi
Urologist
13 Years • MBBS MS FMAS MCh URO(OSM)
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda
Consult Top Specialists Here

Dr. Kunal Kumar Mehar
Urologist
10 Years • Mbbs, Ms, Mch
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr Sriharsha Ajjur
Urologist
10 Years • MBBS,MS,Mch
Bengaluru
Apollo Hospitals Jayanagar, Bengaluru

Dr. Duraisamy S
Urologist
38 Years • MBBS, MS (General Surgery), Mch (Urology)
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)
Dr. Mohamad Ali
Urologist
1 Years • MBBS, MS General Surgery, M Ch Urology
Pune
Apollo Hospitals Pune, Pune

Dr Karthik Maripeddi
Urologist
13 Years • MBBS MS FMAS MCh URO(OSM)
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda
More articles from Hernia
Frequently Asked Questions
Can a hernia go away on its own?
In adults, abdominal wall hernias generally do not heal on their own. Symptoms may fluctuate, but the opening persists. Hiatal hernia symptoms can improve with medication and lifestyle changes, but the hernia anatomy usually remains.
How do I know if my hernia is serious?
Seek emergency care if the bulge becomes painful and cannot be pushed back in, or if you develop nausea, vomiting, fever, or can’t pass stool/gas. These could indicate incarceration or strangulation.
What’s the recovery time after laparoscopic hernia repair?
Most people return to desk work in 3–7 days and light exercise by 1–2 weeks, with heavier lifting after 4–6 weeks depending on your surgeon’s advice and the hernia type.
Are hernia belts or trusses safe?
They may temporarily reduce discomfort for some groin hernias but don’t fix the problem. Use only under clinical guidance to avoid skin or pressure injury, and monitor for any red flags.
What lifestyle changes help reduce hernia symptoms?
Avoid heavy lifting or learn safe techniques, treat cough and constipation, reach a healthy weight, and for hiatal hernias, use reflux strategies like smaller meals and not lying down soon after eating. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7.
.webp)