Guide to IVF
Understand IVF from start to finish with a clear step-by-step guide to the process, success rates, risks, costs, medications, and ways to improve outcomes. Discover who IVF can help and how to select the right clinic for your specific goals. Evidence-based insights, FAQs, and practical tips included.

Written by Dr. M L Ezhilarasan
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
If you are exploring IVF, you are not alone, and you likely have many questions. IVF (in vitro fertilisation) is the most well-known assisted reproduction method, helping people with a range of fertility challenges build their families. Yet understanding the process, success rates, costs, risks, and choices, such as ICSI or PGT, can feel overwhelming.
This guide walks you through IVF step by step, explaining what affects success, how to interpret clinic statistics, and which options are truly evidence-based. You will also find practical tips for managing side effects, questions to ask your clinic, and support for making informed, confident decisions.
Consult a Top Gynaecologist for Personalised Advice
IVF at a glance: What it is and who it helps
This section explains the fundamentals of IVF and when it is recommended.
IVF is a process where eggs are retrieved from the ovaries, combined with sperm in a laboratory (through conventional insemination or ICSI), cultured for several days, and then transferred to the uterus. Any remaining good-quality embryos can be frozen for future use.
IVF can help in cases of blocked fallopian tubes, male factor infertility, endometriosis, ovulation disorders, unexplained infertility, or when preventing genetic disease through embryo testing. It also supports single parents and LGBTQ+ couples building families.
Brief history and advances
The first IVF birth occurred in 1978. Major advancements since then include safer stimulation protocols, vitrification (fast freezing) that improved frozen embryo success, ICSI for severe male factor infertility, and PGT to help select healthier embryos. Single embryo transfer is now common to reduce the risks linked to multiple pregnancies.
Who might consider IVF?
People who have been trying for a year (or six months if they are 35 or older) may be advised to consider IVF. It is also recommended when issues such as tubal damage, low ovarian reserve, severe sperm abnormalities, or prior failed IUI are known. People preserving fertility may undergo related processes like egg or embryo freezing.
Unique insight: IVF is both diagnostic and therapeutic. How eggs and sperm behave in the lab can help identify where challenges lie, even if pregnancy does not occur in the first cycle.
The IVF process and timeline (step by step)
Here is what typically happens in each phase of an IVF journey.
A standard IVF cycle takes around 6–8 weeks from consultation to pregnancy test. If a frozen embryo transfer is planned later, expect an additional 4–6 weeks.
Ovarian stimulation
Daily hormone injections stimulate the development of multiple follicles. Clinic monitoring helps adjust doses and time the trigger injection that matures the eggs and reduces the risk of overstimulation.
Egg retrieval and sperm preparation
Eggs are collected in a short, sedated procedure using ultrasound guidance. A semen sample is processed on the same day, or donor sperm is prepared if needed.
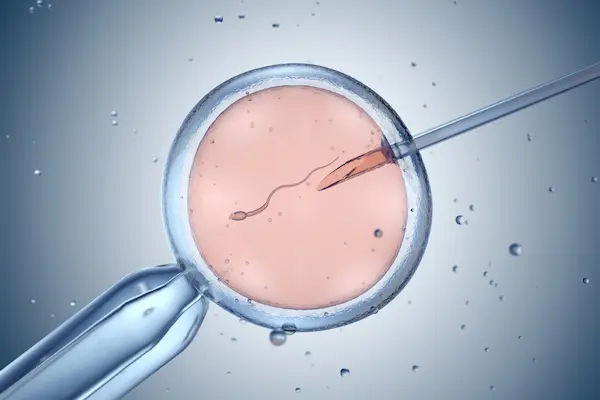
Fertilisation: IVF vs ICSI
With conventional IVF, many sperm are placed around each egg. With ICSI (intracytoplasmic sperm injection), a single sperm is directly injected into each mature egg, often recommended for male factor infertility.
Embryo culture, grading, PGT, and transfer
Embryos remain in the lab from day 3 to day 5–6. Many clinics transfer blastocyst-stage embryos because they are more developed and easier to evaluate. Genetic testing may be recommended in specific situations. Some clinics freeze all embryos and perform a later frozen transfer to optimise results.
The two-week wait and testing
A blood test about 9–12 days after transfer confirms pregnancy. If positive, follow-up scans check early development. If negative, a review helps refine the strategy for a future attempt.
Unique insight: Ask for a personalised cycle calendar with medication and monitoring dates to reduce stress and support planning.
Medications, monitoring, and side effects
Understanding your medication plan helps you stay confident and prepared.
An IVF cycle usually includes:
• Stimulation medication (FSH or hMG)
• Drugs to prevent premature ovulation
• A trigger injection
• Progesterone for luteal support
Common side effects include bloating, breast tenderness, mood shifts, and mild pelvic discomfort. Most people return to regular activity within a day or two after egg retrieval.
OHSS: What to watch for
Modern protocols have reduced the risk of ovarian hyperstimulation syndrome, but symptoms like rapid weight gain, severe bloating, persistent vomiting, and shortness of breath require prompt medical advice.
Managing discomfort
Ice packs, rotating injection sites, hydration, gentle movement, and proper technique for progesterone-in-oil injections can provide relief.
Unique insight: Keeping a symptoms and medication log helps your team fine-tune treatment and detect concerns early.
Success rates: What really affects outcomes
This section explains what influences IVF success, based on current evidence.
Age is the strongest predictor of success because egg quality declines over time. Donor eggs can reset age-related limitations and significantly improve results.
Other key factors
• Embryo quality and stage at transfer
• Use of single embryo transfer to reduce multiple pregnancy risks
• Underlying diagnosis and sperm quality
• Uterine and hormonal conditions
• Laboratory expertise and standards
How to interpret clinic success results
Look for:
• Live birth rate per transfer for your age group
• Cumulative success across multiple transfers from one egg collection
Unique insight: Ask for a personalised cumulative success estimate over two to three transfers, not just one.
Risks, safety, and ethical considerations
Understanding risks allows early recognition and timely support.
Procedure and medical risks
Complications like infection or bleeding after retrieval are rare. OHSS monitoring is essential. IVF has a slightly higher chance of ectopic pregnancy, especially with tubal disease.
Multiple pregnancy and miscarriage
Transferring more than one embryo increases risks for both parents and babies. Miscarriage risk rises with age due to genetic abnormalities in eggs.
Ethics and decision-making
Consent forms cover the number of embryos to transfer, storage duration, and decisions about unused embryos. Planning ahead reduces stress later.
Unique insight: Keep a written record of your values on transfer choices, donor gametes, and embryo storage to revisit when emotions run high.
Costs, insurance, and choosing a clinic
Knowing financial and practical considerations supports smart planning.
What drives cost
Expenses may include:
• Medications
• Egg retrieval and lab work
• ICSI or PGT if required
• Frozen embryo transfer
• Storage fees
• Anaesthesia and facility fees
How to choose a clinic
Consider:
• Transparent reporting of success rates
• Personalised medical protocols
• Embryology lab qualifications
• Patient support services
• Convenience for frequent monitoring
Unique insight: Ask to meet both a nurse and an embryologist before deciding, as you will work closely with them throughout the cycle.
Evidence-based ways to improve success
Small changes can add up to meaningful improvements.
Lifestyle factors
Maintaining a healthy BMI, avoiding smoking, and moderating alcohol and caffeine intake are supported by evidence. A balanced diet and regular moderate exercise also help.
Supplements and sperm health
Prenatal vitamins are essential. Ask your doctor before starting supplements like CoQ10 or DHEA. For sperm: avoid tobacco and overheating, and address health conditions such as diabetes.
Beware unproven add-ons
Some clinic extras have limited evidence. Always ask what benefit is expected in your specific case.
Unique insight: Focus on health habits 8–12 weeks before stimulation, which aligns with the growth period of sperm and developing follicles.
Alternatives and additions to IVF
Options can be tailored to diagnosis, age, and personal preference.
Non-IVF alternatives
• Expectant management
• Ovulation induction with timed intercourse
• IUI for mild male factor or unexplained infertility
IVF variations
• ICSI for male factor infertility
• PGT for certain genetic conditions
• Mild or natural-cycle IVF for low responders
• Donor eggs, sperm, or embryos
• Gestational carriers when pregnancy is not medically advisable
Unique insight: Create a pathway map with your doctor showing next steps depending on fertilisation, embryo development, and test outcomes.
Conclusion
Starting IVF can feel complex, but understanding the journey makes it far more manageable. Age and embryo quality influence success, yet your everyday habits, consistent medication use, and communication with your care team play a major role too.
Approach IVF as a process that may involve multiple transfers. Plan financially and emotionally around cumulative success rather than a single attempt. Ask questions, learn what is truly evidence-based, and choose a clinic aligned with your needs and values.
With the right information, support, and planning, you can move through IVF with confidence and clarity.
Consult a Top Gynaecologist for Personalised Advice
Consult a Top Gynaecologist for Personalised Advice

Dr. Mona Yadav
Obstetrician and Gynaecologist
19 Years • MBBS, MD (Obstetrics & Gynaecology)
Dombivli
Nulife multispeciality, Dombivli

Dr. Debajyoti Goswami
Obstetrician and Gynaecologist
10 Years • MBBS,D.G.O(DNB),Adv. Infertility Tech.(AIIMS),Fellowship in Diabetes(U.K),Comprehensive Abortion Care(Govt. Of W.B), Certificate in Clinical Embryology(AIIMS, BHUBANESWAR)
Bankura
D.G Clinic, Bankura
(25+ Patients)

Dr. Parul Sharma
Obstetrician and Gynaecologist
8 Years • MBBS, MS (Obstetrics & Gynaecology)
New Delhi
THE DOCTORS NESST, New Delhi

Dr. Asha Rani Singh
Obstetrician and Gynaecologist
24 Years • MBBS DGO
Delhi
Dr Asha Rani Singh Clinic, Delhi

Dr. Shyamala Devi
Obstetrician and Gynaecologist
38 Years • MBBS, MS Obstetrics & Gynaecology
Vijayawada
Sri Shivshakti Nilayam, Vijayawada
Consult a Top Gynaecologist for Personalised Advice

Dr. Mona Yadav
Obstetrician and Gynaecologist
19 Years • MBBS, MD (Obstetrics & Gynaecology)
Dombivli
Nulife multispeciality, Dombivli

Dr. Debajyoti Goswami
Obstetrician and Gynaecologist
10 Years • MBBS,D.G.O(DNB),Adv. Infertility Tech.(AIIMS),Fellowship in Diabetes(U.K),Comprehensive Abortion Care(Govt. Of W.B), Certificate in Clinical Embryology(AIIMS, BHUBANESWAR)
Bankura
D.G Clinic, Bankura
(25+ Patients)

Dr. Parul Sharma
Obstetrician and Gynaecologist
8 Years • MBBS, MS (Obstetrics & Gynaecology)
New Delhi
THE DOCTORS NESST, New Delhi

Dr. Asha Rani Singh
Obstetrician and Gynaecologist
24 Years • MBBS DGO
Delhi
Dr Asha Rani Singh Clinic, Delhi

Dr. Shyamala Devi
Obstetrician and Gynaecologist
38 Years • MBBS, MS Obstetrics & Gynaecology
Vijayawada
Sri Shivshakti Nilayam, Vijayawada
More articles from Infertility
Frequently Asked Questions
How long does an IVF cycle take?
From starting stimulation to pregnancy test is typically 4–6 weeks. A later frozen embryo transfer adds another 4–6 weeks.
Do I need ICSI if the sperm looks normal?
Not always. ICSI is mainly for male factor infertility or limited egg numbers. Many patients do well with conventional IVF.
What is the benefit of single embryo transfer?
SET reduces risks linked to multiple pregnancy while maintaining strong cumulative success if additional embryos are available.
What affects IVF cost?
Medication, ICSI, PGT, freezing, storage fees, and monitoring schedules all influence the final price.
Can I boost IVF success naturally?
Yes. A healthy BMI, avoiding smoking, good sleep, and managing medical conditions like thyroid disorders support success.