PCOS and Infertility: A Guide for Successful Conception
Explore how PCOS affects fertility and discover strategies to improve your chances of successful conception.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
Polycystic Ovary Syndrome (PCOS) is one of the most common, yet often misunderstood, causes of female infertility. If you're on this journey, you're not alone; PCOS affects approximately 1 in 10 women of childbearing age. The dream of starting a family can feel daunting when faced with irregular periods, unpredictable ovulation, and a confusing diagnosis. But here's the most important thing to know: a PCOS diagnosis is not a synonym for infertility. It means the path to pregnancy may require a more tailored and proactive approach. This comprehensive guide is designed to demystify the connection between PCOS and infertility, offering evidence-based information on everything from the underlying hormonal mechanisms to the latest treatment options. We'll explore how lifestyle changes, medications, and assisted reproductive technologies can help you overcome these challenges and move closer to your goal of parenthood.
Understanding the PCOS-Infertility Connection
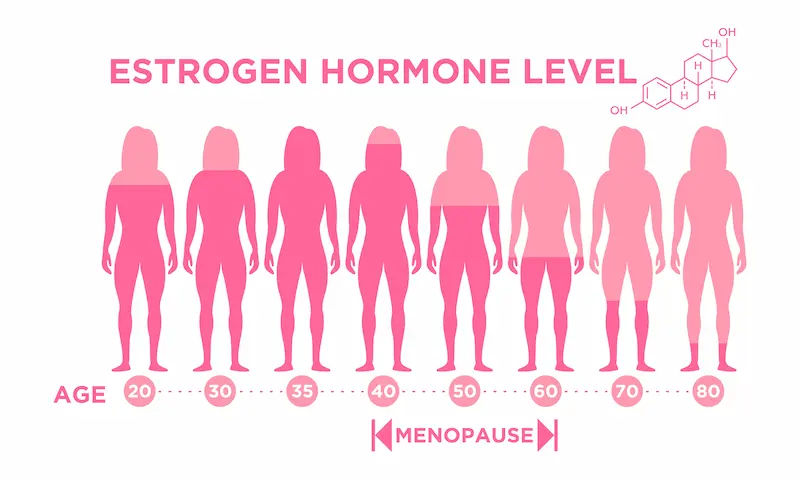
At its core, the link between PCOS and infertility is hormonal. PCOS is characterised by a group of symptoms stemming from hormonal imbalances, primarily involving insulin and androgens ("male" hormones like testosterone).
The Hormonal Rollercoaster: Androgens and Insulin Resistance
Many women with PCOS have insulin resistance. This means their body's cells don't respond effectively to insulin, causing the pancreas to produce even more insulin to compensate. High levels of insulin, in turn, trigger the ovaries to produce excess androgens. This surge in androgens disrupts the delicate hormonal conversation between the brain (pituitary gland) and the ovaries. Normally, the pituitary gland releases Follicle-Stimulating Hormone (FSH) and Luteinising Hormone (LH) in a specific rhythm to stimulate follicle growth and ovulation. In PCOS, the high androgen environment interferes with this process, leading to the development of multiple small follicles that fail to mature and release an egg. This is the classic "polycystic" appearance on an ultrasound, not actual cysts, but stalled follicles.
Why Ovulation Becomes Irregular or Stops
The direct consequence of this hormonal disruption is anovulation (the absence of ovulation) or oligo-ovulation (infrequent ovulation). Without a mature egg being released, sperm has nothing to fertilise, making conception impossible. This is why women with PCOS often experience irregular or absent menstrual periods. The period you might get is often a "withdrawal bleed" from a buildup of the uterine lining, not a true menstrual cycle following ovulation. Understanding your ovulation signs with PCOS is crucial, as standard ovulation predictor kits can be unreliable due to consistently elevated LH levels.
Consult a Gynaecologist for the best advice
Getting a Formal PCOS Diagnosis
A proper diagnosis is the first step toward an effective treatment plan. Doctors use the Rotterdam Criteria, which requires that you meet at least two of the following three conditions:
The Rotterdam Criteria: The Gold Standard for Diagnosis
1. Irregular or Absent Periods: This is the primary indicator of ovulatory dysfunction.
2. Clinical or Biochemical Signs of High Androgens: This can include physical symptoms like hirsutism (excess facial or body hair), severe acne, or male-pattern baldness, or it can be confirmed by a blood test showing elevated testosterone levels.
3. Polycystic Ovaries on Ultrasound: An ultrasound revealing 20 or more follicles on one or both ovaries.
Essential Tests: Blood Work and Ultrasound
Your doctor will likely order a series of blood tests to check hormone levels (e.g., testosterone, LH, FSH, AMH) and screen for insulin resistance (fasting glucose and insulin). A transvaginal ultrasound provides a clear view of the ovaries. It's important to rule out other conditions that can mimic PCOS, such as thyroid disorders. If you suspect you have PCOS, consulting a gynaecologist or endocrinologist online with Apollo24|7 can be a convenient first step to discuss your symptoms and necessary tests. Apollo24|7 offers a convenient home collection for essential hormone panels.
Get Your Health Assessed
Your Fertility Treatment Roadmap: From Lifestyle to ART
Treatment is not one-size-fits-all; it's a ladder, often starting with the least invasive options.
Foundation First: The Power of Lifestyle Modifications
This is the cornerstone of managing PCOS and improving fertility. Even a 5-10% reduction in body weight can restart ovulation in overweight women.
Nutrition for PCOS: Balancing Blood Sugar
Focus on a low-glycemic index diet to manage insulin resistance. Think complex carbohydrates (whole grains, legumes, vegetables), lean proteins, and healthy fats. The goal is to avoid blood sugar spikes that exacerbate insulin production.
Exercise: More Than Just Weight Loss
A combination of moderate-intensity cardio (like brisk walking) and strength training is ideal. Muscle is metabolically active and helps improve insulin sensitivity.
Ovulation Induction Medications: Clomid and Letrozole
If lifestyle changes aren't enough, the next step is often medication to induce ovulation.
• Letrozole: Now often considered a first-line treatment, Letrozole works by temporarily lowering estrogen levels, which prompts the brain to produce more FSH to stimulate follicle growth. Studies show it may have higher ovulation and live birth rates than Clomid in women with PCOS.
• Clomiphene (Clomid): A well-established drug that blocks estrogen receptors in the brain, also leading to increased FSH production.
Your doctor will monitor you with ultrasounds to track follicle growth and prevent the risk of multiples. The debate of letrozole vs clomid for PCOS is best had with your fertility specialist.
Assisted Reproductive Technologies (ART)
If ovulation induction isn't successful, ART may be recommended.
• Intrauterine Insemination (IUI): Often combined with ovulation drugs, IUI involves placing washed, concentrated sperm directly into the uterus around the time of ovulation, giving sperm a head start.
• In Vitro Fertilisation (IVF): This is the most effective ART. Eggs are retrieved after ovarian stimulation, fertilised with sperm in a lab, and resulting embryos are transferred to the uterus. For women with PCOS, IVF protocols are carefully managed to prevent Ovarian Hyperstimulation Syndrome (OHSS), a potential risk.
Beyond Medicine: Supporting Your Overall Health with PCOS
Managing PCOS isn’t just about medication; here’s how you can support your overall health naturally and effectively.
Managing the Emotional Journey of PCOS Infertility
The stress of infertility can be overwhelming. Seeking support from a therapist, joining a support group, or practicing mindfulness and yoga can be incredibly beneficial for your mental well-being, which is an integral part of your health.
The Role of Supplements (Inositol, Vitamin D, etc.)
Some supplements show promise in managing PCOS symptoms. Myo-inositol and D-chiro-inositol (forms of Vitamin B8) have been shown to improve insulin sensitivity and ovarian function. Many women with PCOS are also deficient in Vitamin D, which is important for egg quality. Always discuss any supplements with your doctor before starting.
Conclusion: Empowering Your Path to Parenthood
Navigating PCOS and infertility can feel like a complex and emotional journey, but it's a path paved with growing understanding and effective solutions. From foundational lifestyle changes that reset your metabolic health to targeted medical interventions that directly address ovulation, the options available today are powerful and promising. Remember, knowledge is your greatest asset. By understanding the "why" behind your PCOS, you can proactively partner with your healthcare team to choose the best fertility treatment for PCOS that aligns with your body and your goals. While the road may have challenges, each step you take whether it's adopting a new healthy habit, completing a cycle of medication, or simply giving yourself grace on a difficult day brings you closer to your dream of building a family. Stay informed, advocate for yourself, and lean on your support system.
Consult a Gynaecologist for the best advice
Consult a Gynaecologist for the best advice

Dr. Vineet Mishra
Infertility Specialist
36 Years • MD, Phd, DSc
Ahmedabad
Apollo Hospitals - Gandhinagar, Ahmedabad, Ahmedabad
Dr. Arti Sharma
Obstetrician and Gynaecologist
8 Years • MBBS, DNB(obstetrics and gynaecology)
Bengaluru
DIAGNOFY CLINIC, Bengaluru

Dr. Sreeparna Roy
Obstetrician and Gynaecologist
8 Years • MBBS , MS (OBSTETRICS & GYNAECOLOGY), Fellowship in Infertility, Endoscopy & Ultrasonography), Fellowship in Laparoscopy & Hysteroscopy,DRM
Kolkata
Dr Utsa Basu Clinic, Kolkata

Dr. Saheli Kapat
Obstetrician and Gynaecologist
11 Years • MBBS, DNB Obstetrics & Gynaecology,FMAS(Fellowship in Minimal access surgery)
Kolkata
Dr. Saheli Kapat's Clinic, Kolkata

Dr. Millie Dasgupta
Obstetrician and Gynaecologist
10 Years • MBBS,DNB (Obst. & Gynae.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
Consult a Gynaecologist for the best advice

Dr. Vineet Mishra
Infertility Specialist
36 Years • MD, Phd, DSc
Ahmedabad
Apollo Hospitals - Gandhinagar, Ahmedabad, Ahmedabad
Dr. Arti Sharma
Obstetrician and Gynaecologist
8 Years • MBBS, DNB(obstetrics and gynaecology)
Bengaluru
DIAGNOFY CLINIC, Bengaluru

Dr. Sreeparna Roy
Obstetrician and Gynaecologist
8 Years • MBBS , MS (OBSTETRICS & GYNAECOLOGY), Fellowship in Infertility, Endoscopy & Ultrasonography), Fellowship in Laparoscopy & Hysteroscopy,DRM
Kolkata
Dr Utsa Basu Clinic, Kolkata

Dr. Saheli Kapat
Obstetrician and Gynaecologist
11 Years • MBBS, DNB Obstetrics & Gynaecology,FMAS(Fellowship in Minimal access surgery)
Kolkata
Dr. Saheli Kapat's Clinic, Kolkata

Dr. Millie Dasgupta
Obstetrician and Gynaecologist
10 Years • MBBS,DNB (Obst. & Gynae.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
More articles from Infertility
Frequently Asked Questions
1. Can I get pregnant with PCOS without any treatment?
Yes, it is possible, especially for women with milder forms of PCOS who still ovulate occasionally. However, because ovulation is unpredictable, the chances are significantly lower than for women with regular cycles. Most women will require some form of intervention to improve their odds.
2. What are the chances of getting pregnant with PCOS using IVF?
IVF success rates with PCOS are generally very good. Women with PCOS often have a high number of eggs retrieved. The main challenge is quality over quantity, and modern lab techniques have improved outcomes significantly. Success rates depend on age, overall health, and the clinic, but many women with PCOS achieve pregnancy through IVF.
3. Does metformin help with PCOS fertility?
Metformin is primarily used to treat insulin resistance. By improving insulin sensitivity, it can help regulate menstrual cycles and restore ovulation in some women, making it easier to conceive. It is often used alongside fertility drugs like Letrozole or Clomid.
4. Are pregnancy risks higher with PCOS?
Women with PCOS have a slightly increased risk of certain pregnancy complications, such as gestational diabetes, preeclampsia, and premature birth. This is why careful monitoring and management by your healthcare team during pregnancy are essential.
5. What is the best PCOS diet plan for pregnancy?
There is no single 'best' diet, but a low-glycemic, anti-inflammatory approach is most recommended. This includes plenty of vegetables, lean proteins, healthy fats (like avocado and nuts), and complex carbohydrates (like quinoa and sweet potatoes), while minimising processed foods, sugar, and refined carbs.