Guide to Low FODMAP Diet: A Beginner's Plan for Gut Health
Learn how the Low FODMAP Diet can help manage IBS and digestive issues. This beginner’s guide covers phases, food lists, meal plans, and tips for long-term gut health.

Written by Dr. Mohammed Kamran
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026

Introduction
Are you tired of the constant bloating, cramping, and unpredictable digestive distress that makes social events and daily life a challenge? If so, you're not alone. Millions struggle with irritable bowel syndrome (IBS) and similar functional gut disorders. The Low FODMAP Diet has emerged as a powerful, science-backed approach to identifying your personal food triggers and reclaiming control over your gut health. But navigating this diet can seem overwhelming. This comprehensive guide breaks down everything you need to know—from the science of FODMAPs to a practical step-by-step plan. We'll explore what the diet is, who it's for, how to follow its three phases correctly, and provide you with a clear list of foods to enjoy and avoid. Get ready to embark on a journey toward a happier, calmer digestive system.
What Are FODMAPs Anyway?
FODMAP is an acronym that stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. In simpler terms, they are a collection of short-chain carbohydrates and sugar alcohols that are poorly absorbed in the small intestine. Instead of being absorbed into your bloodstream, they travel to your large intestine, where they become a feast for your gut bacteria.
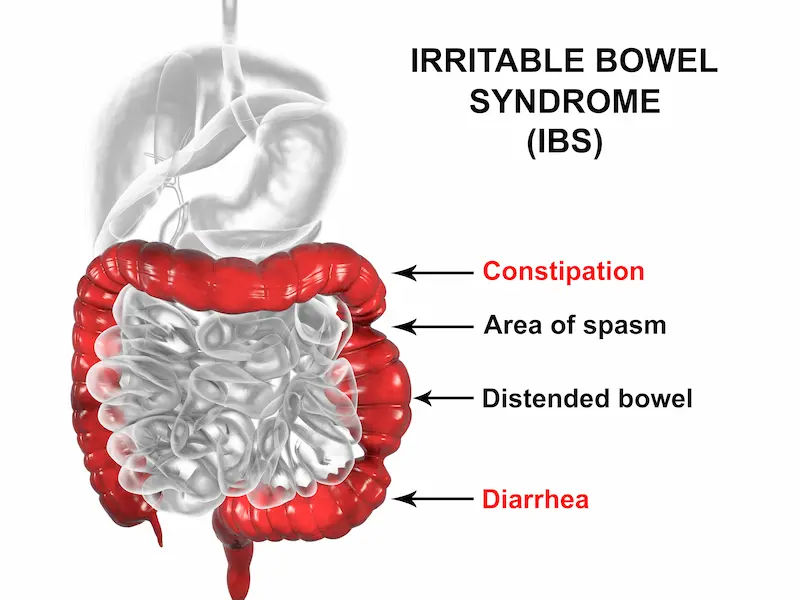
The Science Behind FODMAPs and Digestion
The problem isn't the bacteria themselves, but the byproduct of their feast: gas. Additionally, FODMAPs are osmotically active, meaning they draw water into the large intestine. The combination of excess gas and water leads to the classic symptoms of IBS: bloating, distension, abdominal pain, wind, and altered bowel habits (constipation or diarrhea). It's not an allergy; it's a sensitivity to the volume and type of these poorly absorbed carbs.
The Five Groups of FODMAPs
Understanding the five groups helps you see the patterns in what might be triggering you:
Oligosaccharides: Fructans (wheat, onions, garlic) and GOS (legumes, beans).
Disaccharides: Lactose (milk, soft cheese, yogurt).
Monosaccharides: Fructose (in excess of glucose, found in honey, apples, high-fructose corn syrup).
Polyols: Sorbitol and Mannitol (some fruits and vegetables, and often used as artificial sweeteners).
Who is the Low FODMAP Diet Actually For?
The Low FODMAP Diet is not a weight-loss trend or a general wellness diet. It is a specialised elimination diet designed for a specific medical purpose.
The Primary Link: Irritable Bowel Syndrome (IBS)
Extensive research, pioneered by Monash University, has shown that a low fodmap diet can significantly reduce symptoms in approximately 50-75% of people with medically diagnosed IBS. If you experience chronic bloating, pain, and irregular bowels, this diet could be a transformative tool. A 2017 meta-analysis published in the European Journal of Nutrition confirmed its efficacy in improving abdominal pain and quality of life in IBS patients.
Other Potential Candidates for the Diet
Sometimes, healthcare professionals may recommend it for other functional gut disorders like small intestinal bacterial overgrowth (SIBO), though its role here is more nuanced. It is crucial to note that if your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24|7 to rule out other more serious digestive conditions like celiac disease or inflammatory bowel disease (IBD).
The Three Phases of the Low FODMAP Diet
This diet is not meant to be a lifelong sentence of restriction. It's a diagnostic tool that unfolds in three distinct phases, typically lasting 4-8 weeks total.
Phase 1: The Elimination Phase
This initial stage involves strictly avoiding all high-FODMAP foods for a period of 2-6 weeks. The goal is to give your digestive system a complete break, allowing symptoms to settle down. This phase is temporary. If you don't experience significant symptom relief after 3-4 weeks, it's unlikely that FODMAPs are your primary trigger, and you should consult a doctor online with Apollo24|7 to discuss other possibilities.
Phase 2: The Reintroduction (Challenge) Phase
This is the most important phase. You systematically reintroduce high-FODMAP foods, one group at a time, in controlled amounts while carefully monitoring your symptoms. For example, you might test fructose by eating a small amount of mango on day one, wait two days, then try a larger amount. This process helps you identify which specific FODMAP groups you react to and your individual tolerance threshold.
Phase 3: The Personalisation (Integration) Phase
Armed with knowledge from Phase 2, you can now liberalise your diet. You permanently avoid only the FODMAPs and in the quantities that trigger your symptoms, while happily reintroducing all others. This creates a sustainable, long-term diet unique to you, maximising food variety without provoking symptoms.
Your Comprehensive Low FODMAP Food List
Note: Servings matter! A food can be low FODMAP in a small serving but high in a large one. Always check the latest Monash University FODMAP Diet app for the most updated data.
Foods to Enjoy Freely (Low FODMAP)
Fruits: Bananas (unripe), blueberries, strawberries, oranges, grapes, cantaloupe.
Vegetables: Carrots, cucumbers, bell peppers, spinach, zucchini, eggplant, potatoes.
Proteins: Beef, chicken, fish, eggs, tofu, tempeh.
Grains: Oats, rice, quinoa, gluten-free bread and pasta.
Dairy Alternatives: Lactose-free milk, almond milk, hard cheeses (cheddar, parmesan).
Foods to Avoid or Limit (High FODMAP)
Fruits: Apples, pears, mangoes, watermelon, peaches, dried fruits.
Vegetables: Onions, garlic, asparagus, cauliflower, mushrooms, snow peas.
Dairy: Cow's milk, soft cheeses (ricotta), yogurt, ice cream.
Legumes: Beans, lentils, chickpeas.
Sweeteners: Honey, high-fructose corn syrup, agave nectar, sugar-free sweets with polyols (sorbitol, xylitol).
A Sample Low FODMAP Diet Meal Plan
Here’s what a realistic day on a plate might look like during the elimination phase, full of low fodmap recipes for dinner and beyond:
Breakfast: Scrambled eggs with spinach and bell peppers, served with a side of sliced strawberries.
Lunch: Quinoa salad with grilled chicken, cucumber, carrots, and a lemon-olive oil dressing.
Snack: A handful of walnuts and a lactose-free yogurt.
Dinner: Baked salmon with roasted carrots and zucchini, and a serving of mashed potatoes.
Dessert: Two dark chocolate squares (check for no high-FODMAP sweeteners).
Potential Benefits and Challenges of the Diet
The Proven Benefits for Digestive Wellness
For the right person, the benefits are life-changing. Studies consistently report dramatic reductions in bloating, abdominal pain, and gas. Patients often experience more normalised bowel habits and a significant improvement in overall quality of life, energy levels, and mental well-being, as the constant anxiety around food and symptoms diminishes.
Common Pitfalls and How to Avoid Them
The biggest risk is turning the temporary elimination phase into a permanent, overly restrictive diet. This can lead to nutritional deficiencies, a poor relationship with food, and an unnecessary impact on your gut microbiome due to lack of prebiotic fibers (found in high-FODMAP foods like onions and garlic). This is precisely why the reintroduction phase under guidance is non-negotiable.
Important Considerations Before You Start
Why Working with a Professional is Crucial
This is not a DIY diet. A registered dietitian or nutritionist specialising in digestive health is essential. They can ensure you are a good candidate, provide accurate food lists, guide you through the complex reintroduction phase, prevent nutritional gaps, and offer much-needed support. Self-diagnosing and improperly following the diet can do more harm than good.
Is This a Long-Term Solution?
No. The long-term goal is liberalisation. The personalised diet you create in Phase 3 is your long-term solution, which should be as varied and inclusive as your tolerance allows. The initial strict low FODMAP phase is merely a short-term investigative tool.
Conclusion
Embarking on the Low FODMAP Diet can feel like a daunting task, but it’s important to view it as a structured journey of discovery rather than a permanent restriction. By methodically identifying your unique food triggers, you empower yourself to make informed choices that can lead to a dramatic reduction in digestive discomfort and a significant boost in your overall quality of life. Remember, the path to a happier gut is not about eating the same limited foods forever; it's about learning how to expand your diet confidently by understanding exactly what works for your body. If you suspect you have IBS and are struggling to find relief, take this guide as your starting point and have a conversation with a healthcare professional to see if this approach is right for you. Your journey to digestive peace could begin today.
More articles from Irritable Bowel Syndrome
Frequently Asked Questions
1. How long does it take to see results on a low FODMAP diet?
Most people with a FODMAP sensitivity will notice a significant improvement in bloating and pain within the first week of the elimination phase. Full symptom relief can take up to 3-4 weeks.
2. Can I ever eat garlic and onions again?
Possibly! While they are high in fructans and are common triggers, the reintroduction phase will test your tolerance. You might find you can handle a small amount of garlic-infused oil (where the fructans are not soluble in oil) or a small serving of cooked onion.
3. Is the low FODMAP diet gluten-free?
Not exactly. The diet is low in fructans, and wheat is a major source. Therefore, you avoid wheat, which means you end up eating many gluten-free foods. However, the target is the fructan, not the gluten. Pure gluten protein is actually low FODMAP.
4. Will this diet harm my gut microbiome?
The strict elimination phase can reduce the intake of prebiotic fibers that feed good gut bacteria, which is why it should be short-term. The personalisation phase, where you reintroduce all tolerated FODMAPs, is designed to restore a healthy and diverse microbiome.
5. Do I need to worry about nutrient deficiencies?
This is a key reason to work with a professional. A dietitian can ensure you get adequate fiber, calcium, and B vitamins from low FODMAP sources during the elimination phase to prevent any deficiencies.