CAKUT Explained Kidney and Urinary Tract Birth Defects
Learn about CAKUT, a group of kidney and urinary tract birth defects. Understand its causes, symptoms, diagnosis, and treatment options for children.

Introduction
The 20-week prenatal ultrasound is a milestone filled with anticipation. For most parents, it’s the first glimpse of their baby. But sometimes, this scan reveals something unexpected: a potential issue with the baby’s kidneys or urinary tract. If you've found yourself in this situation, hearing terms like "pyelectasis," "hydronephrosis," or the umbrella term CAKUT, it’s natural to feel worried and overwhelmed. This guide is here to help.
CAKUT stands for Congenital Anomalies of the Kidney and Urinary Tract. It's not a single disease but a spectrum of birth defects that affect the development of a baby's kidneys, ureters (tubes connecting kidneys to bladder), bladder, or urethra. These are among the most common congenital disorders, but the outcomes vary widely. Many conditions are mild and resolve on their own, while others require careful monitoring or treatment. This article will walk you through everything you need to know from understanding the different types of congenital abnormality kidney and urinary tract issues to diagnosis, treatment options, and long-term care, empowering you to be an informed advocate for your child's health.
What exactly is CAKUT? Understanding the Basics
At its core, CAKUT represents a glitch in the complex developmental process of the urinary system, which forms in the first trimester of pregnancy. Instead of developing normally, one or more parts of the system may be missing, shaped incorrectly, blocked, or positioned in the wrong place. This can disrupt the vital function of the urinary system: to filter waste from the blood and remove it from the body as urine.
A key thing to understand is that CAKUT is a descriptive category, not a prognosis. The severity can range from a minor, harmless issue that never causes problems to a serious condition that requires significant medical intervention.
How Common Are These Birth Defects?
Congenital kidney abnormalities are relatively common. They are estimated to occur in approximately 1 in every 500 live births. They account for nearly 20-30% of all prenatally diagnosed birth defects. This high prevalence makes awareness and early detection crucial for managing potential health outcomes effectively.
Consult a Paediatric Nephrologist for the best advice
A Closer Look at Common CAKUT Conditions
The world of CAKUT includes several specific conditions. Understanding the differences can help you better comprehend your child's diagnosis.
Kidney-Related Anomalies
Kidney-related anomalies are structural or functional abnormalities that can affect a child’s kidney health from birth.
Renal Agenesis (Missing Kidney)
This occurs when one or both kidneys fail to develop. Unilateral renal agenesis (one missing kidney) is more common. The solitary kidney often enlarges to compensate (hyperfiltration) and can sustain normal life. Bilateral renal agenesis (both kidneys missing) is a severe, life-threatening condition because it leads to a lack of amniotic fluid (oligohydramnios), which is critical for lung development.
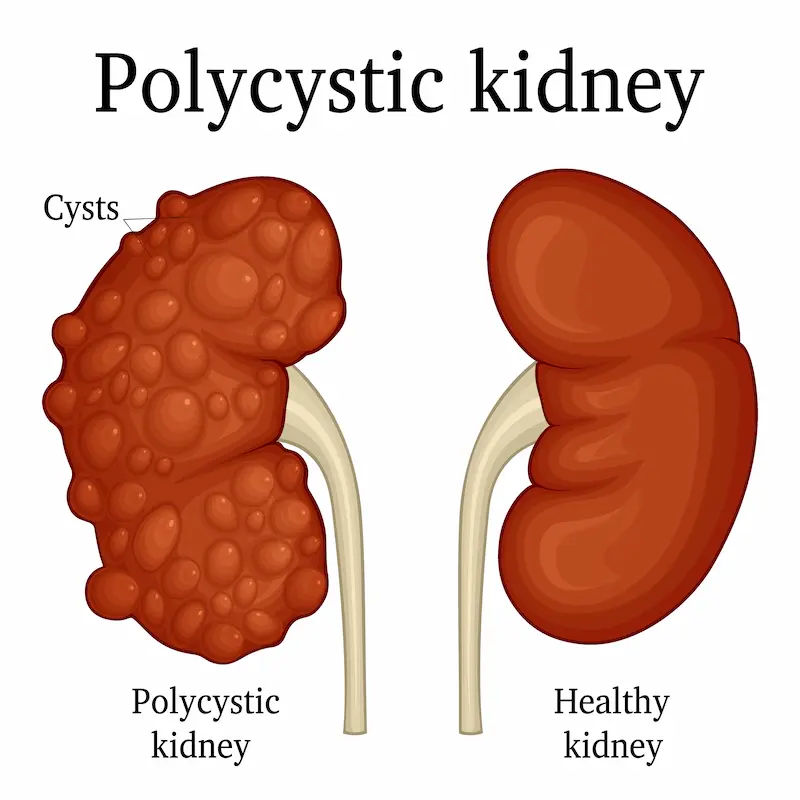
Multicystic Dysplastic Kidney (MCDK)
In MCDK, the kidney does not develop properly and is replaced by multiple cysts. It has no function. Unlike polycystic kidney disease (a genetic disorder), MCDK is usually isolated and non-hereditary. Fortunately, in many cases, the cysts shrink and disappear over several years, and the other kidney takes over.
Hydronephrosis (Swollen Kidney)
This is the most commonly detected congenital abnormality kidney issue on prenatal ultrasound. It means the kidney is swollen due to a backup of urine. This can be caused by a blockage or, commonly, by a condition called vesicoureteral reflux (VUR). The severity guides management, which can range from watchful waiting to surgery.
Urinary Tract and Bladder Anomalies
Urinary tract and bladder anomalies involve structural or functional issues that can impact a child’s ability to store and pass urine properly.
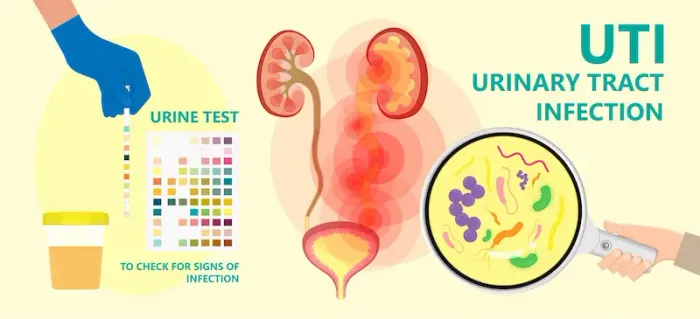
Vesicoureteral Reflux (VUR)
VUR happens when the valve between the ureter and bladder doesn't close properly, allowing urine to flow backward from the bladder up to the kidneys. This can increase the risk of kidney infections. Treatment for vesicoureteral reflux often starts with low-dose antibiotics to prevent infections, as many children outgrow mild to moderate VUR.
Posterior Urethral Valves (PUV)
This is a serious condition that occurs only in boys. It involves extra flaps of tissue in the urethra that block the outflow of urine. This can cause severe back-pressure, damaging the bladder and kidneys. It is typically diagnosed prenatally and requires surgical intervention soon after birth.
Bladder Exstrophy
This is a rare, complex defect where the bladder develops inside out and is exposed on the outside of the abdomen. It requires major reconstructive surgery after birth but has good long-term outcomes with specialised care.
What Causes CAKUT? Unraveling the Mystery
In most cases, the exact cause of a congenital kidney abnormality is unknown. It's believed to result from a combination of genetic and environmental factors that disrupt normal development.
Genetic Factors and Syndromes
Some cases of CAKUT are linked to genetic mutations or are part of broader genetic syndromes, such as VACTERL association or chromosomal disorders like Down syndrome. If there's a family history of kidney anomalies, the risk may be slightly higher.
Environmental and Maternal Factors
Certain factors during pregnancy may increase risk, though the link is not always clear. These can include poorly controlled maternal diabetes, use of specific medications (like ACE inhibitors), or vitamin deficiencies (e.g., Vitamin A). However, it's important to note that most cases occur sporadically without any identifiable cause.
Recognising the Signs: Symptoms of CAKUT
Many cases are detected prenatally with no immediate symptoms in a newborn. When symptoms do appear, they vary by age and condition.
Symptoms in Newborns and Infants
• A palpable mass or lump in the abdomen.
• Swollen abdomen.
• Failure to thrive (not gaining weight).
• Unexplained fever, which could indicate a kidney infection.
• Fussy feeding or vomiting.
Symptoms in Older Children
• Recurrent fevers or urinary tract infections (UTIs).
• Bedwetting (enuresis) after being potty-trained.
• Pain in the flank or abdomen.
• High blood pressure (hypertension).
• Swelling in the face, hands, or feet.
• Excessive thirst and urination.
If your child exhibits any of these symptoms, especially recurrent fevers or swelling, it is crucial to consult a paediatrician. For a quick evaluation, you can also consult a paediatric specialist online with Apollo24|7.
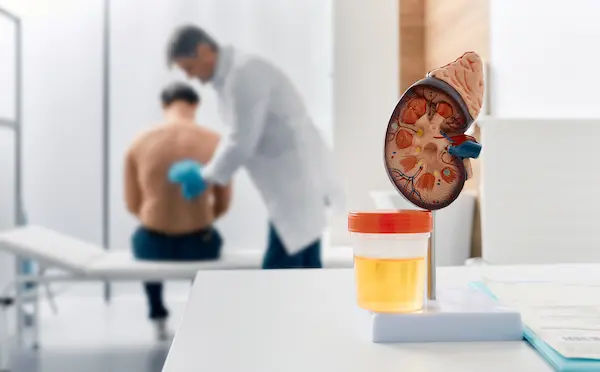
How is CAKUT Diagnosed? The Step-by-Step Process
Early and accurate diagnosis of CAKUT is essential to manage kidney and urinary tract anomalies effectively.
The Role of Prenatal Ultrasound
The journey often begins before birth. Routine fetal ultrasounds can detect signs like hydronephrosis, an absent kidney, or a bladder that doesn't empty properly. This allows for planning with a team of specialists (maternal-fetal medicine, paediatric urologist, paediatric nephrologist) for the birth and postnatal care.
Postnatal Tests and Scans
After birth, the diagnosis is confirmed and refined using:
• Renal Ultrasound: A painless scan to visualise the kidneys and bladder.
• Voiding Cystourethrogram (VCUG): A special X-ray that checks for VUR by inserting a catheter into the bladder and filling it with contrast dye.
• Nuclear Renal Scan (DMSA/MAG3): Tests that use a small amount of radioactive tracer to assess kidney function and drainage.
• Blood and Urine Tests: To measure kidney function (creatinine, BUN) and check for infection or protein loss.
Apollo24|7 offers convenient home collection for tests like creatinine and urine analysis, making follow-up monitoring easier for families.
Get Your Health Assessed
Treatment Pathways for Congenital Kidney Abnormalities
Treatment is highly individualised. The goal is always to preserve kidney function, prevent infections, and ensure normal growth and development.
Monitoring and Medication
For many mild conditions like low-grade hydronephrosis or VUR, the first line of "treatment" is careful observation with repeated ultrasounds. Long-term effects of multicystic dysplastic kidney, for instance, are often just annual monitoring of the solitary kidney. Children with VUR may be placed on a daily low-dose antibiotic to prevent UTIs while waiting to see if they outgrow the condition.
Surgical Interventions and Procedures
Surgery is reserved for cases where there is a significant blockage, high-grade reflux that isn't improving, or a condition like PUV.
• Pyeloplasty: Corrects a blockage where the ureter meets the kidney (UPJ obstruction).
• Ureteral Reimplantation: Corrects VUR by repositioning the ureter into the bladder to create a better valve.
• Valve Ablation: A minimally invasive procedure to cut away the obstructing tissue in Posterior Urethral Valves.
Long-Term Outlook and Living with CAKUT
With modern medicine, the prognosis for children with CAKUT is excellent. Even those with significant anomalies can lead full, active lives with proper care.
The Importance of Ongoing Nephrology Care
Children with CAKUT need long-term follow-up with a paediatric nephrologist (kidney specialist) or urologist. This includes regular monitoring of blood pressure, urine tests for protein, and blood tests to track kidney function. This proactive approach helps catch any decline in function early.
Potential Complications: Chronic Kidney Disease (CKD)
A small percentage of children with severe CAKUT may develop chronic kidney disease (CKD). This underscores the importance of lifelong monitoring. Management of CKD focuses on controlling blood pressure, managing diet, and, in some cases, preparing for dialysis or a kidney transplant in the future.
Conclusion
Receiving a CAKUT diagnosis for your child can be a daunting experience, filled with complex medical terms and uncertainty. However, knowledge is power. Understanding that these congenital abnormalities of the kidney and urinary tract exist on a broad spectrum is the first step. From minor, self-resolving issues to conditions requiring sophisticated care, modern paediatric medicine has a robust toolkit for diagnosis, management, and treatment. The key is partnership: working closely with your child’s medical team, staying vigilant with follow-up appointments, and being an advocate for their health. Remember, with appropriate care, the vast majority of children with CAKUT thrive. Stay informed, ask questions, and lean on the expertise of your healthcare providers to navigate this journey with confidence.
Consult a Paediatric Nephrologist for the best advice
Consult a Paediatric Nephrologist for the best advice

Dr Bharath Kumar S
Cardiologist
5 Years • MBBS MD DrNB ( Cardiology )
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Rohit Vohra
Paediatric Pulmonologist
10 Years • MBBS, MD PEDIATRICS, FELLOWSHIP IN PEDIATRIC INTENSIVE CARE,FELLOWSHIP IN PULMONOLOGY
Delhi
Apollo Hospitals Indraprastha, Delhi
(75+ Patients)

Dr Varakishan Kuramana
Paediatrician
8 Years • MBBS MD Pediatrics Fellowship in Neonatology
Visakhapatnam
Apollo Hospital, Healthcity, Visakhapatnam, Visakhapatnam

Dr Akkammal Sathyabama
neonatologist
9 Years • MBBS,MD,F(NNF)
Madurai
Apollo Women & Child care Hospital, Madurai, Madurai

Dr Edison Albert B E
neonatologist
6 Years • MBBS, DCH, DNB(Pediatrics), Fellowship Neonatology
Chennai
Apollo Speciality Hospitals OMR, Chennai
Consult a Paediatric Nephrologist for the best advice

Dr Bharath Kumar S
Cardiologist
5 Years • MBBS MD DrNB ( Cardiology )
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Rohit Vohra
Paediatric Pulmonologist
10 Years • MBBS, MD PEDIATRICS, FELLOWSHIP IN PEDIATRIC INTENSIVE CARE,FELLOWSHIP IN PULMONOLOGY
Delhi
Apollo Hospitals Indraprastha, Delhi
(75+ Patients)

Dr Varakishan Kuramana
Paediatrician
8 Years • MBBS MD Pediatrics Fellowship in Neonatology
Visakhapatnam
Apollo Hospital, Healthcity, Visakhapatnam, Visakhapatnam

Dr Akkammal Sathyabama
neonatologist
9 Years • MBBS,MD,F(NNF)
Madurai
Apollo Women & Child care Hospital, Madurai, Madurai

Dr Edison Albert B E
neonatologist
6 Years • MBBS, DCH, DNB(Pediatrics), Fellowship Neonatology
Chennai
Apollo Speciality Hospitals OMR, Chennai
More articles from Kidney Disease
Frequently Asked Questions
1. Can CAKUT be prevented?
In most cases, no, because the causes are often unknown or genetic. However, maintaining a healthy pregnancy with good prenatal care, managing chronic conditions like diabetes, and avoiding certain medications can help reduce overall risks.
2. My baby’s prenatal ultrasound showed mild hydronephrosis. Should I be worried?
Mild hydronephrosis is very common and often resolves on its own after birth without any treatment. Your doctor will recommend a postnatal ultrasound to confirm, but in most cases, it's a reason for monitoring, not for immediate concern.
3. What is the difference between CAKUT and Polycystic Kidney Disease (PKD)?
CAKUT refers to structural malformations that happen during development. PKD is a specific genetic disorder that causes numerous cysts to grow in the kidneys over time, leading to enlarged kidneys and progressive loss of function. MCDK, a type of CAKUT, is different from PKD.
4. If I have a child with CAKUT, what are the chances of it happening in a future pregnancy?
The risk depends on the specific type of CAKUT and whether it's part of a known genetic syndrome.

_6.webp)