Guide to Kidney Transplant Nephrology
Know about kidney transplant, what it is, who needs it, donor options, procedure, recovery, day of surgery, anaesthisia and more.

Introduction
A kidney transplant can be life-changing, but the journey from evaluation to recovery can feel overwhelming. This guide to kidney transplant nephrology breaks down what you need to know in clear, practical language so you can make confident decisions alongside your healthcare team. We’ll explain who needs a kidney transplant, how donor matching works, what to expect before and after surgery, common risks and complications, and how to protect your new kidney for the long term. You’ll also learn about medications, diet, exercise, infection prevention, and special situations like pregnancy and pediatric transplants. Whether you are a patient, caregiver, or family member, this resource translates nephrology concepts into everyday terms, with examples, data from leading sources, and helpful tips. If symptoms like fever, swelling, or decreased urine persist beyond two weeks, consult a doctor online with Apollo24|7 for further evaluation.
Kidney Transplant: What It Is and Who Needs It
A kidney transplant is a surgery to place a healthy kidney from a donor into someone whose kidneys no longer work adequately due to end-stage kidney disease (ESKD). Unlike dialysis, which filters the blood several times a week, a transplant can restore more natural kidney function around the clock. Many people report better energy, improved appetite, and enhanced quality of life after transplant compared with dialysis, and some data show improved survival, especially for those who receive a living donor kidney earlier in their disease course.
Consult Top Nephrology Doctor for Personalised Advice
How a transplant compares with dialysis
1. Benefits: More dietary freedom, fewer fluid restrictions, better fertility and sexual health, and often the ability to return to work or studies.
2. Limitations: Requires lifelong immunosuppression (anti-rejection medicines) with potential side effects and infection risk. Not everyone is a candidate due to other medical conditions.
3. Outcomes: One-year graft survival often exceeds 90% for deceased donor transplants and 95% for living donor transplants at many centres; living donor kidneys typically function longer on average.
Signs you may be ready for transplant evaluation
1. eGFR consistently below 20 mL/min/1.73m² or already on dialysis.
2. Progressive kidney disease with symptoms like severe fatigue, uncontrolled blood pressure, or complications such as anaemia and bone disease.
3. Your nephrologist recommends starting the transplant evaluation process.
If symptoms like swelling, breathlessness, persistent nausea, or low urine output worsen, consult a doctor online with Apollo24|7 for further evaluation and guidance.
Donor Options and Matching: Finding the Right Kidney
Living donor transplants usually offer shorter waiting times, better early function, and longer average graft survival compared with deceased donor kidneys. A donor can be a family member, friend, or altruistic donor. If a compatible living donor isn’t available, patients can be listed for a deceased donor kidney through a national/regional allocation system.
Living vs deceased donors: pros and cons
1. Living donor advantages: Planned surgery, reduced cold ischemia time, often higher-quality kidneys, and improved outcomes. Donors undergo rigorous screening for safety.
2. Deceased donor advantages: No donor needed in your network; options like “kidneys with higher KDPI” may be available sooner. Some programs use machine perfusion to optimise organ quality.
3. Considerations: Discussions should include HLA matching, blood type compatibility, and personal/ethical factors. For many, the paired kidney exchange program is key to finding a compatible match.
HLA, crossmatch, and ABO compatibility explained
• ABO blood type compatibility reduces immediate rejection risk.
• HLA (human leukocyte antigen) matching: Closer matches can improve long-term outcomes, but modern immunosuppression allows successful transplants even with fewer matches [6][8].
• Crossmatch testing checks for donor-specific antibodies in the recipient’s blood; a negative crossmatch is the goal.
Paired exchange and desensitization
1. Paired kidney exchange: Two or more donor-recipient pairs swap donors to overcome incompatibility.
2. Desensitization: Specialized treatments to reduce antibodies in highly sensitized patients so they can accept a kidney they would otherwise reject. Not all centers offer this; risks and benefits must be weighed.
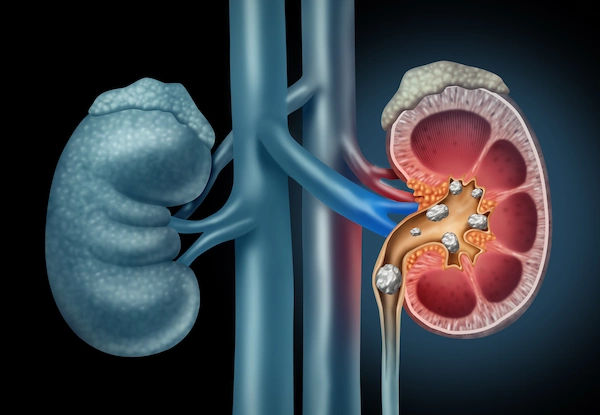
Pre-Transplant Evaluation and Getting Listed
The transplant evaluation ensures it’s safe to proceed and that you’ll benefit. It typically includes blood tests (kidney function, blood group, HLA typing, viral screening), heart assessments (ECG, echocardiogram, sometimes stress tests), imaging (chest X-ray, abdominal imaging), and cancer screenings as age-appropriate [8]. Dental and infection clearance help lower postoperative infection risk. Vaccinations (e.g., hepatitis B, influenza, pneumococcal, COVID-19) are updated before immunosuppression begins.
Medical tests, vaccines, and dental clearance (H3)
1. Labs: Creatinine, eGFR, electrolytes, blood count, HbA1c for diabetes, viral serologies (HBV, HCV, HIV, CMV, EBV). Apollo24|7 offers convenient home collection for many pretransplant labs, and post-transplant tacrolimus monitoring when prescribed.
2. Imaging: Ultrasound of kidneys/bladder, vascular mapping, cardiac testing based on risk.
3. Vaccines and dental health: Address cavities, gum disease, and complete recommended vaccines prior to transplant.
Cardiac risk, diabetes, and weight considerations
Heart health is pivotal; untreated coronary disease can increase surgical risk. good diabetes control helps wound healing and reduces infection risks.
- Weight optimization supports smoother recovery; some centers set BMI goals before listing.
Practical prep: paperwork, caregiver plans, finances
1. Identify a caregiver for the first weeks after surgery.
2. Discuss time off, travel plans to the transplant center, and medication costs.
3. Keep all documents (test results, insurance approvals) organized.
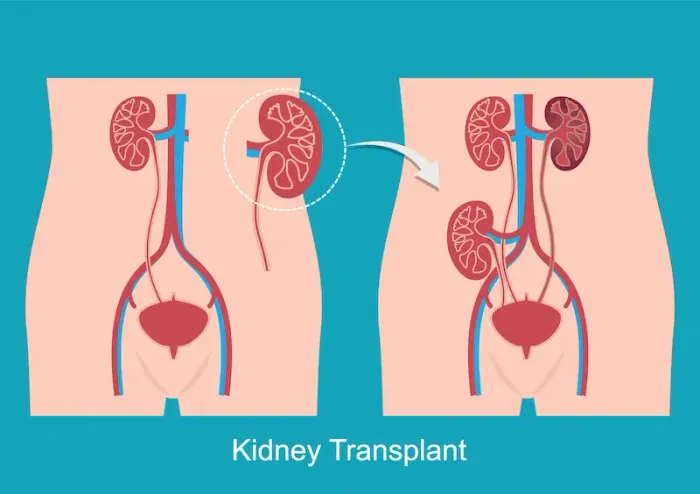
The Surgery and Hospital Stay: What to Expect
Kidney transplant surgery generally takes 2–3 hours. The new kidney is placed in the lower abdomen (iliac fossa), and the donor ureter is connected to your bladder. Most people begin making urine soon after blood flow is restored—especially with living donor kidneys—though some deceased donor kidneys may be “sleepy” initially and need temporary dialysis [1][2].
Day of surgery and anesthesia
Immunosuppression and Rejection: Your Daily Playbook
Most recipients take a combination of medicines: a calcineurin inhibitor (tacrolimus or cyclosporine), an antiproliferative agent (mycophenolate or azathioprine), and steroids. Some regimens use steroid minimization after the early months. Induction therapy (e.g., basiliximab or anti-thymocyte globulin) may be given around the time of surgery based on immunologic risk.
Tacrolimus, mycophenolate, steroids—how they work
Tacrolimus: Reduces T-cell activation. Trough levels are monitored; too low risks rejection, too high risks toxicity (tremor, kidney effects). Ask about tacrolimus level monitoring at home via lab home collection if available.
Mycophenolate: Lowers lymphocyte proliferation; common side effects include stomach upset and low white blood cells.Steroids: Control inflammation; side effects can include weight gain, mood changes, and elevated blood sugar.
Recognizing rejection and when to call your team
1. Symptoms can be subtle: rising creatinine, reduced urine output, swelling, fever, tenderness over the graft, or sudden high blood pressure. Only a biopsy can confirm rejection, and many episodes are treatable when caught early.
2. If you notice fever, decreasing urine, or new swelling, consult a doctor online with Apollo24|7 promptly for guidance and possible urgent evaluation.
Infections, vaccines, and cancer screening
Early months: Higher risk of infections like CMV or BK virus; your team may prescribe preventive medications and regular blood tests.
Vaccines: Keep up with non-live vaccines; avoid live vaccines after transplant unless guided by your transplant team.
Screening: Because long-term immunosuppression can increase cancer risk, adhere to regular screenings (skin checks, Pap smears, colonoscopies as indicated).
Life After Transplant: Diet, Exercise, Work, and Travel
Your new kidney thrives on steady routines: medication adherence, heart-healthy habits, and prudent infection prevention. Nutrition counseling helps you strike the right balance of protein for healing without overloading the kidney. A “kidney transplant diet plan” often focuses on moderate protein, low salt, and safe food handling to minimize infection risk.
Nutrition: salt, protein, potassium, and food safety
Salt: Limit to help control blood pressure and protect the kidney.
Protein: Adequate for healing but avoid high-protein fads; your dietitian will guide amounts.
Potassium and phosphorus: These usually improve after transplant, but levels can vary with medications; labs guide adjustments.
Food safety: Wash produce well, avoid undercooked meats/eggs, and be careful with unpasteurized products to reduce infection risk.
Fitness, bone health, and mental wellbeing (H3)
1. Start with walking and gradually add strength training to rebuild muscle.
2. Bone health: Steroids and prior kidney disease raise fracture risk—ensure adequate calcium and vitamin D; ask about bone density checks.
3. Mental health: Anxiety about rejection or lab results is common. Support groups and counseling help many people cope.
4. Pregnancy, sexual health, and family planning (H4)
5. Fertility often improves. Most centers recommend waiting 1–2 years after transplant before pregnancy, with stable kidney function and medicines safe in pregnancy [3][6].
6. Use contraception until your team confirms it’s safe to try. Discuss any plans early with your nephrology and obstetric teams.
Complications and Long-Term Outcomes
Common post-transplant issues include high blood pressure, diabetes (sometimes steroid- or tacrolimus-associated), and elevated lipids. Your nephrologist will fine-tune medicines and recommend lifestyle steps to protect both your heart and kidney.
Common issues: high blood pressure, diabetes, lipids (H3)
1. Target blood pressure is individualized; ACE inhibitors or ARBs may be used if appropriate.
2. Blood sugar monitoring is essential, especially if you’re on steroids or tacrolimus.
3. Lipid control reduces cardiovascular risk—diet plus statins when needed.
BK virus, CMV, and urinary infections
BK virus nephropathy: Managed by adjusting immunosuppression and close monitoring; early detection matters.
CMV infection: Preventive drugs or preemptive monitoring strategies reduce risk; report fever or GI symptoms promptly.
UTIs: Common post-transplant; stay hydrated and practice hygiene. Seek care for burning, fever, or back pain.
How long a kidney transplant lasts and what affects it ?
1. A living donor kidney often functions 15–20 years on average; deceased donor kidneys often 10–15 years, with wide individual variation [3][4].
2. 0Factors: Donor type, HLA matching, adherence to meds, control of blood pressure/diabetes, and avoiding infections/tobacco.
3. Even if a transplant eventually fails, many patients can be re-listed or pursue a second transplant.
When a second transplant is considered (H4)
If a graft fails, options include re-transplantation or dialysis. Antibody levels and prior history guide strategy; paired exchange may help when sensitization is high.
Building Your Care Team and Staying Engaged
Successful transplant nephrology care is a team effort. You, your caregiver, nephrologist, surgeon, transplant coordinator, pharmacist, dietitian, and social worker all play key roles.
Roles of nephrologist, surgeon, coordinator, and pharmacist
1. Nephrologist: Oversees kidney health, immunosuppression, and long-term risks.
2. Surgeon: Leads the operation and immediate surgical recovery.
3. Coordinator: Your point person for scheduling, education, and logistics.
4. Pharmacist: Educates on drug interactions (for example, avoiding grapefruit with tacrolimus).
Medication adherence and tracking tips (H3)
- Use phone alarms, pill organizers, and a “medication passport” card.
- Keep a backup set of medicines when traveling; plan time-zone changes with your team.
- Unique insight: Perform a “10-second check” at morning and evening: confirm you took your dose, check for new side effects, and glance at your daily fluid/blood pressure goals.
Conclusion
Kidney transplant nephrology brings together advanced surgery, precise immunosuppression, and everyday healthy habits to give your new kidney the best chance to thrive. From choosing between living and deceased donors to navigating pre-transplant testing, surgery, and lifelong follow-up, each step is designed to reduce risk and maximize your quality of life. The most powerful tools you can bring are medication adherence, infection awareness, heart-healthy lifestyle choices, and a strong partnership with your care team. If you experience warning signs like fever, swelling, pain over the graft, or a drop in urine output, seek medical advice quickly—early action saves kidneys. For ongoing care and convenience, consider teleconsultations and home lab collections for tests such as creatinine, eGFR, and tacrolimus trough levels through Apollo24|7. Stay engaged, ask questions, and celebrate milestones. With the right knowledge and support, you can protect your transplant and live fully.
Consult Top Nephrology Doctor for Personalised Advice
Consult Top Nephrology Doctor for Personalised Advice

Dr. Aswini Kumar Panigrahi
Nephrologist
23 Years • MBBS, MD (Int. Med.), DNB Nephro
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(225+ Patients)

Dr. Pardha Saradhi
Nephrologist
9 Years • MBBS, MD-DNB (Gen. Med.), DNB (Nephro)
Hyderabad
Apollo Hospitals D R D O kanchanbagh, Hyderabad
(75+ Patients)

Dr. Hareesha Babu K
Nephrologist
25 Years • MBBS, MD (General Medicine), DM (Nephrology),FASN, FRCP(Glasg), FRCP (Edin)
Bangalore
Kidney & Hypertension Care, Bangalore
(125+ Patients)

Dr. Sanjay Maitra
Nephrologist
24 Years • MBBS, MD (Int. Med.), DM (Nephro)
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(100+ Patients)

Dr. Kity Sarkar
Nephrologist
15 Years • MBBS,MD(Genl. Med.), DrNB(NEPHROLOGY)
Kolkata
Dr. Kity Sarkar's Clinic, Kolkata
Consult Top Nephrology Doctor for Personalised Advice

Dr. Aswini Kumar Panigrahi
Nephrologist
23 Years • MBBS, MD (Int. Med.), DNB Nephro
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(225+ Patients)

Dr. Pardha Saradhi
Nephrologist
9 Years • MBBS, MD-DNB (Gen. Med.), DNB (Nephro)
Hyderabad
Apollo Hospitals D R D O kanchanbagh, Hyderabad
(75+ Patients)

Dr. Hareesha Babu K
Nephrologist
25 Years • MBBS, MD (General Medicine), DM (Nephrology),FASN, FRCP(Glasg), FRCP (Edin)
Bangalore
Kidney & Hypertension Care, Bangalore
(125+ Patients)

Dr. Sanjay Maitra
Nephrologist
24 Years • MBBS, MD (Int. Med.), DM (Nephro)
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(100+ Patients)

Dr. Kity Sarkar
Nephrologist
15 Years • MBBS,MD(Genl. Med.), DrNB(NEPHROLOGY)
Kolkata
Dr. Kity Sarkar's Clinic, Kolkata
More articles from Kidney Failure
Frequently Asked Questions
1) How long does a kidney transplant last?
On average, living donor kidneys last 15–20 years and deceased donor kidneys 10–15 years, though individual outcomes vary based on matching, adherence, and overall health.
2) What are common kidney transplant rejection symptoms?
Rising creatinine, reduced urine output, swelling, fever, pain or tenderness over the graft, and sudden high blood pressure. If these occur, consult your transplant team. If symptoms persist, consult a doctor online with Apollo24|7 for further evaluation.
3) How is tacrolimus level monitoring done?
Your team checks blood “trough” levels regularly to keep them in a target range. Many centers allow home collection for labs; Apollo24|7 offers convenient home blood tests where available.
4) Can I get pregnant after a kidney transplant?
Many can, typically after 1–2 years with stable kidney function and safe medications. Discuss plans early with your nephrologist and obstetrician.
5) What is paired kidney exchange?
If your donor isn’t compatible, you can “swap” donors with another pair through a registry, allowing both recipients to receive compatible kidneys.
_2.webp)