Kidney Failure: Causes, Symptoms and Management
Learn about kidney failure, including its causes, warning signs, and management strategies. Understand how early detection and treatment can protect kidney health.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
Witnessing signs of kidney failure can be an overwhelming and frightening experience. Your kidneys, those silent, hard-working bean-shaped organs, are vital filters for your body. When their function declines, it affects your entire system. But here's the crucial message: a kidney failure diagnosis is not the end. Effective kidney failure management is a proactive journey that can significantly improve your quality of life and slow the disease's progression. This comprehensive guide will walk you through everything you need to know, from understanding the root causes and recognising early symptoms to navigating treatment options like dialysis and transplant, and implementing powerful lifestyle changes. Whether you’re a patient or a caregiver, this article will equip you with the knowledge to take confident steps toward better health.
Understanding Kidney Failure: The Basics
Kidney failure, often called end-stage renal disease (ESRD), occurs when your kidneys lose their ability to filter waste and excess fluids from your blood effectively. This isn't usually a sudden event but the final stage of a gradual loss of function known as Chronic Kidney Disease (CKD). Understanding this progression is the first step in managing kidney failure successfully.
What is Chronic Kidney Disease (CKD)?
CKD is a long-term condition categorized into five stages, based on your glomerular filtration rate (GFR), a measure of how well your kidneys are filtering blood. Stages 1 and 2 indicate mild damage with normal or slightly reduced function, while stages 3 and 4 represent moderate to severe damage. Stage 5 is classified as kidney failure, where the kidneys are functioning at less than 15% of their normal capacity. Management strategies become increasingly intensive as you move through these stages of kidney disease.
The Path to Kidney Failure: Common Causes
Two primary culprits are responsible for most cases of kidney failure: diabetes and high blood pressure. Consistently high blood sugar from diabetes can damage the kidneys' delicate filtering units over time. Similarly, uncontrolled hypertension puts excessive pressure on the blood vessels in the kidneys, impairing their function. Other causes include autoimmune diseases like lupus, genetic conditions such as polycystic kidney disease, prolonged urinary tract obstructions, and recurrent kidney infections.
Consult a Nephrologist for the best advice
Recognising the Signs: When to Seek Help
Early detection is powerful. Many people in the early stages of kidney disease experience few to no symptoms, which is why it's often called a "silent" disease. Symptoms typically become noticeable only after significant damage has occurred.
Early Warning Symptoms of Declining Kidney Function
Fatigue and Trouble Concentrating: A buildup of toxins can cause overwhelming tiredness and brain fog.
Trouble Sleeping: When kidneys aren't filtering properly, toxins stay in the blood, which can interfere with sleep.
Swollen Feet and Ankles (Oedema): Impaired kidney function can cause sodium retention, leading to swelling.
Changes in Urination: This includes foamy urine (indicating protein leakage), urinating more often (especially at night), or seeing blood in urine.
Symptoms of Advanced Kidney Failure
As the condition worsens, symptoms become more severe and systemic:
Persistent Nausea and Vomiting: Due to a buildup of waste products (uremia).
Severe Shortness of Breath: Caused by fluid buildup in the lungs or anaemia.
Metallic Taste in Mouth/Food Tasting Funny: Known as uremic fetor.
Itchy, Dry Skin: From mineral and nutrient imbalances in the blood.
Chest Pain: If fluid builds up around the lining of the heart.
If you are experiencing several of these symptoms, especially if you have risk factors like diabetes or hypertension, it is crucial to consult a doctor. You can book a quick online consultation with a nephrologist on Apollo24|7 for an initial evaluation and guidance on next steps.
The Cornerstones of Medical Management
When kidneys can no longer sustain the body's needs, medical intervention is necessary. The choice of treatment depends on the cause of kidney failure, overall health, and personal preferences.
1. Dialysis: Filtering Your Blood Artificially
Dialysis is a life-sustaining treatment that performs the functions of healthy kidneys. There are two main types.
Haemodialysis: How It Works and What to Expect
This process uses a machine (a dialyzer) to filter waste and extra fluid from your blood. To get your blood into the dialyzer, a doctor creates vascular access, typically in your arm. Treatments are usually done at a dialysis centre three times a week for about four hours each session. While it requires a significant time commitment, it allows for professional supervision during treatment.
Peritoneal Dialysis: A Home-Based Approach
This method uses the lining of your own abdomen (the peritoneum) as a natural filter. A catheter is placed in your abdomen, and a special solution (dialysate) is infused. Waste products pass from blood vessels in the peritoneal membrane into the dialysate, which is then drained out after a few hours. The major advantage is that it can be done at home, often overnight, offering greater flexibility.
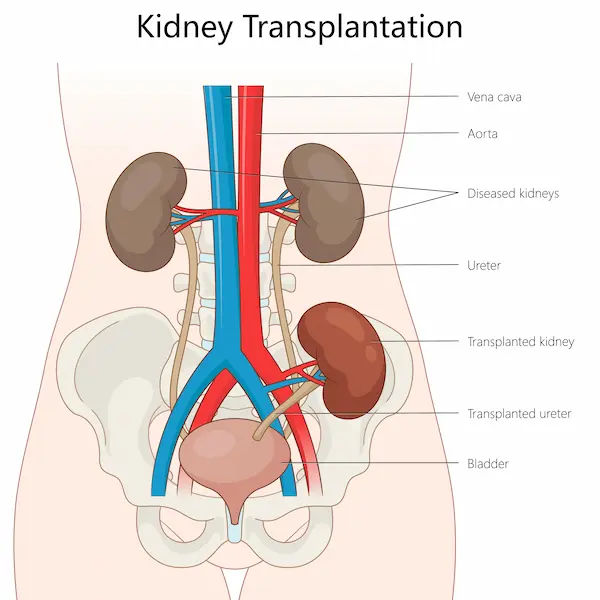
2. Kidney Transplant: The Goal of Long-Term Management
A transplant involves surgically placing a healthy kidney from a living or deceased donor into your body. It is considered the best treatment for many with ESRD, as a successful transplant can free you from dialysis and offer a better quality of life. However, it requires lifelong immunosuppressant medications to prevent your body from rejecting the new organ and comes with its own surgical risks and waiting lists.
3. Medications to Manage Symptoms and Slow Progression
Even with dialysis or transplant, medication is a pillar of managing kidney failure. This can include:
Phosphate binders: To control high phosphorus levels.
Erythropoietin (EPO) shots: To treat anaemia and fatigue.
Blood pressure medications: Like ACE inhibitors or ARBs, which also help protect kidney function.
Diuretics: To help the body eliminate extra fluid.
Vitamin D and calcium supplements: To support bone health.
Conclusion: Taking Control of Your Kidney Health
Navigating the path of kidney failure is undoubtedly challenging, but it is a path you do not have to walk alone. Effective kidney failure management is a multifaceted approach that blends modern medicine with dedicated self-care. By understanding your condition, adhering to your treatment plan, whether it's dialysis, medication, or a transplant, and embracing crucial lifestyle changes, you can take profound control of your health and well-being. Remember, every positive choice, from selecting the right foods to taking your medication on time, contributes to stabilizing your condition and improving your quality of life. This journey requires partnership; your healthcare team, including the specialists available on Apollo24|7, is there to provide expert guidance and support every step of the way. Take that first step today by committing to proactive management.
Consult a Nephrologist for the best advice
Consult a Nephrologist for the best advice

Dr. Pardha Saradhi
Nephrologist
9 Years • MBBS, MD-DNB (Gen. Med.), DNB (Nephro)
Hyderabad
Apollo Hospitals D R D O kanchanbagh, Hyderabad
(75+ Patients)

Dr Praveen Kumar Etta
Nephrologist
10 Years • MBBS,MD DM(SGPGI) FORMER ASST(PIMS)
Hyderabad
Apollo Spectra Ameerpet, Hyderabad

Dr Ajay Kumar Sharma
Transplant Specialist Surgeon
39 Years • MBBS, MS, DNB, FRCS (Glas), FRCS (Edin), FRCS (General Surgery), MSc Medical Education
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Aswini Kumar Panigrahi
Nephrologist
23 Years • MBBS, MD (Int. Med.), DNB Nephro
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(225+ Patients)

Dr. Manju Kamal
Nephrologist
12 Years • MBBS,MD(General Medicine), DNB,DM(Nephrology)
Angamaly
Apollo Hospitals Karukutty, Angamaly
More articles from Kidney Failure
Frequently Asked Questions
1. What are the first steps after a kidney failure diagnosis?
The first steps are to partner closely with a nephrologist (kidney specialist), undergo a full evaluation to determine the cause and stage, and begin discussing treatment options like dialysis or transplant eligibility. Education about diet for renal failure patients is also started immediately.
2. Can you recover from kidney failure?
In most cases, the damage from chronic kidney failure is permanent and not reversible. However, with proper management, you can slow the progression of the disease, manage symptoms effectively, and maintain a good quality of life for years. Acute kidney failure can sometimes be reversed with timely treatment.
3. How long can you live with managed kidney failure?
Life expectancy varies greatly depending on age, overall health, the treatment chosen, and how well the treatment plan is followed. With modern dialysis and transplantation, many people live for many years, even decades. Life expectancy on dialysis can be 5-10 years on average, but many exceed this, while a transplant can offer a longer lifespan.
4. What is the best thing to drink for your kidneys?
Water is generally the best and safest drink for your kidneys, as it helps clear sodium and toxins. However, for those on dialysis with strict fluid intake limits, the amount of water and other fluids becomes just as important as the type. Always follow your doctor's specific fluid recommendations.
5. Are there any new treatments for kidney failure on the horizon?
Yes, medical research is ongoing. Innovations include wearable artificial kidneys, new immunosuppressant drugs for transplants, and advanced regenerative medicine techniques aiming to repair damaged kidney tissue. Always discuss the latest options with your nephrologist.
_2.webp)

.webp)