Kidney Stones Diet Guide: What to Eat and Avoid
Comprehensive kidney stone diet guide: what to eat and avoid, hydration tips, calcium and oxalate management, DASH diet, and personalised strategies for prevention.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026

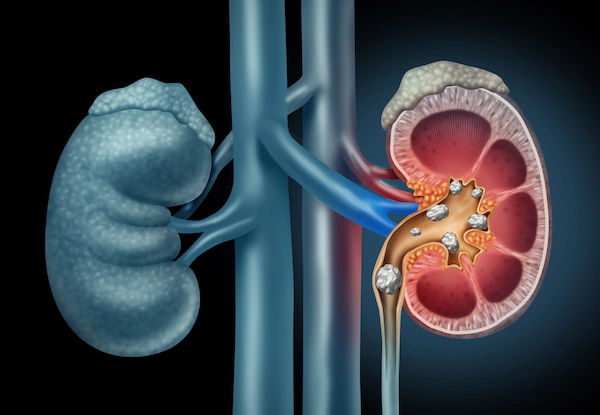
Why Kidney Stones Form—and How Diet Helps
Kidney stones form when minerals and salts in urine become concentrated enough to crystallise. If the urine is too concentrated (low volume), too acidic or alkaline for your stone type, or low in inhibitors like citrate, crystals can grow into stones. Diet influences all three levers: urine volume, urine chemistry (pH and minerals), and inhibitors. For example, eating a high-sodium diet increases urinary calcium, while low fruit/vegetable intake reduces citrate—both raise risk. Conversely, adequate dietary calcium binds oxalate in the gut so less reaches the kidneys, and higher fluid intake dilutes stone-forming minerals.
Environment and genetics matter, too. People living in hot climates sweat more and produce less urine. Some have genetic variants that drive calcium, uric acid, or cystine issues. But across populations, everyday food and drink choices consistently shape stone risk. The kidney stone diet is not one-size-fits-all; it’s a set of evidence-based principles you tailor to your stone type and urine results, with a focus on hydration, balanced minerals, and a plant-forward pattern similar to DASH. If you’ve had recurring stones, a 24-hour urine test helps identify your specific risk factors, so your diet can be precise rather than generic. If you’re unsure where to begin or have pain, blood in urine, fever, or severe symptoms, consult a doctor online with Apollo 24|7 for timely evaluation and treatment.
Know Your Stone Type Before You Change Your Diet
Here’s what you need to know:
Calcium oxalate stones
These account for about 70–80% of stones. Key drivers include low urine volume, high urinary calcium, high urinary oxalate, low citrate, and sometimes high sodium or excessive animal protein. Diet focuses on hydrating, limiting sodium, pairing oxalate-containing foods with calcium, and increasing fruits/vegetables to boost citrate.
Uric acid stones
These form in persistently acidic urine and with high uric acid loads from purine-rich foods and metabolic factors like insulin resistance. Diet works by alkalinising urine (more fruits/vegetables, sometimes potassium citrate), reducing purines (moderate red meat and organ meats), and achieving healthy weight to improve insulin sensitivity.
Struvite and cystine stones
Struvite stones are linked to urinary infections; antibiotics and surgical management are central. Cystine stones arise from a rare genetic disorder; high fluid intake and urine alkalinisation are key, alongside specific medications. For both, your urology team will guide targeted therapy.
Why a 24-hour urine test matters
A 24-hour urine test identifies your personal risk profile—urine volume, calcium, oxalate, citrate, uric acid, sodium, and pH—so you can tailor diet and, if needed, medications such as thiazides for high calcium, potassium citrate for low citrate or uric acid stones, or allopurinol for high uric acid. If you’ve had more than one stone, ask your clinician about this test; it’s the gold standard for personalisation.Consult Top Specialists
Hydration: Your #1 Defense
Here’s what you need to know:
Producing at least 2–2.5 litres of urine daily is the strongest dietary defense against stones; most adults need roughly 2.5–3 litres of fluids per day to meet this goal, more if you sweat heavily or live in hot climates. Practical tip: use urine colour as a guide—aim for pale yellow, like lemonade, not apple juice. Spread fluids across the day and include a glass before bed; if you wake at night, take a few sips.
Best choices include water, infused water, and citrus beverages that provide citrate, a natural inhibitor that binds calcium and reduces crystal formation. Coffee and tea can count toward fluid goals, but be mindful of oxalate in black tea if you form calcium oxalate stones. Sugar-sweetened beverages—especially those with high-fructose corn syrup—are associated with higher stone risk and should be limited. Some colas contain phosphoric acid, which may affect urinary chemistry; swapping to water or sparkling water with citrus is smarter.
Oxalate: What to Limit and How to Pair Foods Wisely
Oxalate binds calcium to form calcium oxalate stones. You don’t need an oxalate-free diet; focus on limiting the highest-oxalate foods and pairing moderate-oxalate foods with calcium at meals. High-oxalate items include spinach, beets, rhubarb, almonds and almond flour, cashews, peanuts, sesame/tahini, wheat bran, Swiss chard, okra, soy products, and dark chocolate/cocoa. Instead of a blanket ban, make smart swaps: replace spinach with romaine or kale; swap almonds for pistachios or walnuts; choose berries or apples over raspberries; and use low-oxalate grains like rice or oats instead of large portions of bran.
Key strategy: Pair oxalate with calcium. Eat oxalate-containing foods alongside dairy or calcium-fortified alternatives so calcium binds oxalate in the gut and less reaches the kidneys. For example, have a small portion of dark chocolate with yoghurt, or a bean-and-veggie bowl with a sprinkle of cheese. Cooking methods help, too: boiling high-oxalate vegetables and discarding the water can reduce oxalate content.
Calcium Is a Friend—If You Get It from Food
It’s counterintuitive, but eating too little calcium can raise stone risk because more free oxalate is absorbed. The goal is adequate dietary calcium: about 1,000–1,200 mg/day from foods like milk, yoghurt, cheese, and calcium-fortified plant milks, plus leafy greens lower in oxalate. Aim to distribute calcium across meals, especially when eating oxalate-containing foods.
Calcium supplements can increase stone risk for some people when taken without food; if you need a supplement, take it with meals and discuss your dose with your clinician, especially if you have a history of calcium stones. Vitamin D is often paired with calcium; test levels before high-dose supplementation.
Sodium and Animal Protein: The “Hidden” Stone Drivers
High sodium intake increases urinary calcium excretion—one of the strongest dietary drivers of stones. Most adults should keep sodium below 2,300 mg/day; many stone formers benefit from aiming closer to 1,500–2,000 mg/day, especially if urinary calcium is high. Label-reading hack: sodium density. Choose products with sodium less than 1 mg per kcal. Restaurant meals are often 1,500–2,500 mg per plate—ask for sauces on the side, choose grilled/steamed options, and skip added salt.
Animal protein (especially red meat, organ meats, and certain seafood) increases urinary calcium and uric acid and lowers citrate. Aim for moderate portions and include more plant proteins, balancing oxalate when needed.
Citrate, Fruits, Vegetables, and the DASH Advantage
Citrate is a natural stone inhibitor that binds calcium and prevents crystals from forming. Fruits and vegetables, especially citrus, increase urinary citrate and alkalinise urine—helpful for calcium oxalate and uric acid stones. “Lemonade therapy” can be part of your daily fluids. While exact amounts vary, many clinicians suggest adding the juice of 1–2 lemons to water daily if tolerated.
A DASH-style diet—rich in fruits, vegetables, low-fat dairy, whole grains, nuts, and legumes, and lower in sodium and red meat—has been associated with a significantly lower risk of kidney stones. Beyond stone prevention, DASH supports blood pressure control and metabolic health.
Sugar, Supplements, and Specialty Drinks: Proceed with Caution
Added sugars, particularly high-fructose corn syrup, can increase urinary calcium and oxalate and are linked to a higher kidney stone risk. Keep added sugars under 10% of calories and avoid sugary sodas and energy drinks. Look for hidden sugars in dressings, sauces, and yoghurts.
Supplements deserve attention. High-dose vitamin C has been associated with increased stone risk in men at intakes around or above 1,000 mg/day; consider food-first vitamin C or modest supplements if needed and discuss with your clinician. Calcium supplements, as noted, should be taken with meals if used; vitamin D should be personalised based on labs. Herbal or “alkaline” waters vary widely; focus on proven strategies—fluids, sodium moderation, adequate calcium, and more produce.Consult Top Specialists
Uric Acid Stones: The Low-Purine Plan and Weight Management
Uric acid stones form in acidic urine. Two powerful levers are urine alkalinisation and reducing purine load. Alkalinise with plentiful fruits/vegetables and, when prescribed, potassium citrate to raise urinary pH to a target your clinician sets. Reduce purine-rich foods and moderate poultry while choosing more plant proteins and low-fat dairy.
Weight management matters: insulin resistance lowers urinary pH, promoting uric acid stone formation. A DASH-like, calorie-appropriate plan, regular activity, and adequate sleep all help improve insulin sensitivity. Rapid crash diets or very high-protein plans can worsen stone risk; steady, sustainable weight loss is best. Some people benefit from allopurinol if urinary uric acid is high despite dietary changes.
A Kidney-Stone-Friendly Grocery List and 7-Day Menu
Here’s what you need to know:
Grocery list highlights
• Fluids: still and sparkling water, unsweetened lemon/lime juice, herbal teas
• Produce: citrus, apples, berries, melons, bananas, crucifers, carrots, zucchini, bell peppers, lettuce/romaine, kale, bok choy
• Grains: oats, brown rice, quinoa, whole-wheat (moderate), corn tortillas
• Proteins: eggs, fish, skinless poultry, beans/lentils, tofu/tempeh, low-fat dairy or fortified plant milks/yogurt
• Fats: olive oil, avocado, walnuts/pistachios (moderate), chia/flax (small amounts)
• Seasonings: herbs/spices, garlic, onion, lemon/lime, vinegar; low-sodium stocks
• Extras: yogurt, kefir, cottage cheese; low-sugar electrolyte tablets; citrus vinaigrette
7-day sample menu (abbreviated)
• Breakfasts: overnight oats with fortified soy milk and berries; vegetable omelet with whole-grain toast; yogurt with fruit and a sprinkle of low-oxalate granola
• Lunches: quinoa bowl with roasted veggies, chickpeas, and feta; grilled chicken salad with citrus dressing; brown rice, tofu, and steamed broccoli with sesame-lime sauce
• Dinners: baked salmon, roasted potatoes, green beans; turkey chili with avocado; stir-fry vegetables with shrimp and rice
• Snacks: fruit, yogurt, pistachios/walnuts (small handful), hummus with cucumber and peppers, cottage cheese with pineapple
• Drinks: water, lemon/lime water, herbal tea, diluted low-sugar electrolyte drink during workouts
Dining out: choose grilled or steamed options, swap fries for vegetables, ask for sauces on the side, and order a citrus water. If you’re eyeing a higher-oxalate dish, add a calcium source to offset.
Using Labs to Personalise Your Diet (and When to Test)
A 24-hour urine test measures stone drivers (urine volume, calcium, oxalate, citrate, uric acid, sodium, pH). Typical targets include urine volume ≥ 2–2.5 L/day, moderate urinary calcium and oxalate, adequate citrate, and a pH tailored to your stone type. Results guide diet tweaks:
• High calcium: reduce sodium, moderate animal protein, consider thiazide per clinician
• High oxalate: trim high-oxalate foods, ensure calcium with meals
• Low citrate: increase fruits/vegetables, add citrus; consider potassium citrate
• Acidic urine: more alkaline foods; consider citrate therapy
Bloodwork can uncover contributors like high serum calcium or uric acid. Apollo 24|7 offers convenient home collection for routine blood tests. If your condition does not improve after applying these methods, book a physical visit to a doctor with Apollo 24|7.
Special Situations: Vegetarians, Athletes, Hot Climates, GI Conditions
Here’s what you need to know:
Plant-based diets without the oxalate trap
Vegetarian and vegan diets can be very kidney-stone-friendly when planned carefully: choose lower-oxalate greens, vary plant proteins and pair them with calcium sources, and favour fruits/vegetables for citrate.
Hydration strategies for heat and workouts
In hot climates or during intense exercise, sweat losses can be high. Weigh yourself before and after workouts; replace each 0.5 kg lost with ~500–700 mL fluid. Use low-sugar electrolytes to maintain volume if you exercise >60 minutes. Schedule fluids around peak heat.
Bariatric surgery, IBD, and malabsorption
Fat malabsorption increases oxalate absorption. Strategies include low-oxalate choices, adequate calcium with meals, possibly lower fat intake, and medical supervision.
Myths vs. Facts About the Kidney Stone Diet
Here’s what you need to know:
• Myth: “Cut all calcium.” Fact: Adequate dietary calcium protects against stones by binding oxalate.
• Myth: “All nuts are banned.” Fact: Portion-controlled, lower-oxalate nuts like pistachios/walnuts can fit.
• Myth: “Lemon water alone cures stones.” Fact: It helps raise citrate but works best within an overall plan.
• Myth: “Low-carb/high-protein is fine.” Fact: Very high animal protein increases risk factors; balance matters.
• Myth: “If I drink lots of tea, I’m safe.” Fact: Fluids help, but high-oxalate teas can be a problem if overused.
Building Habits That Stick
Set up your environment: keep a 1 L bottle at your desk and a citrus wedge bowl in your fridge. Batch-cook low-sodium grains and proteins on weekends. Use a simple tracker to check fluids, sodium, and produce servings.
If you’ve had more than one stone, ask your clinician about medications that complement diet: thiazide diuretics for high urinary calcium, potassium citrate to raise citrate or urine pH, and allopurinol for high urinary uric acid when diet alone isn’t enough. If symptoms persist beyond two weeks or you experience severe pain, fever, or vomiting, consult a doctor online with Apollo 24|7 for further evaluation.
Conclusion
The most powerful tools against kidney stones are in your kitchen and your water bottle. By hydrating to keep urine pale, balancing sodium and animal protein, getting enough calcium from food, and eating more fruits and vegetables—especially citrus—you can meaningfully lower the chance of new stones. If you form calcium oxalate stones, focus on smart oxalate swaps and calcium-with-meals; if you form uric acid stones, prioritise urine alkalinisation and a modest, lower-purine pattern. A DASH-like approach benefits almost everyone.
Your plan is strongest when it’s personal. A 24-hour urine test can pinpoint which levers matter most for you, and retesting after changes ensures you’re on the right track. If symptoms continue or you’ve had multiple stones, consult a doctor online with Apollo 24|7. They can review your results, advise on labs, and discuss medications like potassium citrate, thiazides, or allopurinol if needed.
Start with one or two changes this week—carry a marked water bottle, swap spinach for kale, or set a sodium cap for takeout—and build from there. Small, consistent steps add up to big protection for your kidneys.Consult Top Specialists
Consult Top Specialists

Dr Vinay Kumar A V
Nephrologist
8 Years • MBBS, MD - General Medicine, DM - Nephrology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur

Dr. Pardha Saradhi
Nephrologist
9 Years • MBBS, MD-DNB (Gen. Med.), DNB (Nephro)
Hyderabad
Apollo Hospitals D R D O kanchanbagh, Hyderabad
(75+ Patients)

Dr. Margabandhu Saravanan
Nephrologist
12 Years • MBBS, MD, DM (Nephro), DNB (Nephro), MNAMS, FIMSA
Chennai
Apollo Hospitals Greams Road, Chennai
(950+ Patients)
Dr Ch Sashidhar
Nephrologist
20 Years • MBBS, MD General Medicine, DNB, Nephrology
Secunderabad
Apollo Hospitals Secunderabad, Secunderabad
Dr Gayatri Pegu
Nephrologist
15 Years • MD (General Medicine) DM(Nephrology)
Guwahati
Apollo Clinic Guwahati, Assam, Guwahati
Consult Top Specialists

Dr Vinay Kumar A V
Nephrologist
8 Years • MBBS, MD - General Medicine, DM - Nephrology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur

Dr. Pardha Saradhi
Nephrologist
9 Years • MBBS, MD-DNB (Gen. Med.), DNB (Nephro)
Hyderabad
Apollo Hospitals D R D O kanchanbagh, Hyderabad
(75+ Patients)

Dr. Margabandhu Saravanan
Nephrologist
12 Years • MBBS, MD, DM (Nephro), DNB (Nephro), MNAMS, FIMSA
Chennai
Apollo Hospitals Greams Road, Chennai
(950+ Patients)
Dr Ch Sashidhar
Nephrologist
20 Years • MBBS, MD General Medicine, DNB, Nephrology
Secunderabad
Apollo Hospitals Secunderabad, Secunderabad
Dr Gayatri Pegu
Nephrologist
15 Years • MD (General Medicine) DM(Nephrology)
Guwahati
Apollo Clinic Guwahati, Assam, Guwahati
Consult Top Specialists

Dr Vinay Kumar A V
Nephrologist
8 Years • MBBS, MD - General Medicine, DM - Nephrology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur

Dr. Pardha Saradhi
Nephrologist
9 Years • MBBS, MD-DNB (Gen. Med.), DNB (Nephro)
Hyderabad
Apollo Hospitals D R D O kanchanbagh, Hyderabad
(75+ Patients)

Dr. Margabandhu Saravanan
Nephrologist
12 Years • MBBS, MD, DM (Nephro), DNB (Nephro), MNAMS, FIMSA
Chennai
Apollo Hospitals Greams Road, Chennai
(950+ Patients)
Dr Ch Sashidhar
Nephrologist
20 Years • MBBS, MD General Medicine, DNB, Nephrology
Secunderabad
Apollo Hospitals Secunderabad, Secunderabad
Dr Gayatri Pegu
Nephrologist
15 Years • MD (General Medicine) DM(Nephrology)
Guwahati
Apollo Clinic Guwahati, Assam, Guwahati
More articles from Kidney stones
Frequently Asked Questions
1. What is the best drink for preventing kidney stones?
Water is best. Adding lemon or lime boosts citrate, which helps prevent stones. Limit sugary sodas and high-fructose drinks.
2. Should I avoid all calcium if I have calcium stones?
No. Adequate calcium from food lowers risk by reducing oxalate absorption. If using supplements, take them with meals.
3. Which foods are highest in oxalate?
Common high-oxalate foods include spinach, beets, almonds, cashews, wheat bran, and dark chocolate. Use a low-oxalate diet chart and make swaps like romaine for spinach.
4. How does sodium affect kidney stones?
High sodium increases urinary calcium. Aim for <2,300 mg/day (or lower if advised) and watch restaurant meals and packaged foods.
5. Are vitamin C supplements safe if I’ve had stones?
High-dose vitamin C (around or above 1,000 mg/day) has been linked to higher stone risk in men. Consider food-first vitamin C and discuss any supplement with your clinician.