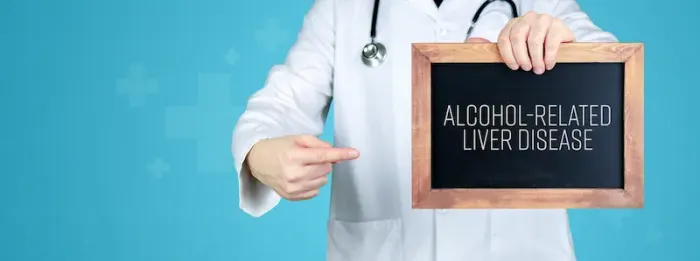
The Sobering Truth: Your Guide to Alcohol-Related Liver Disease Risk
Learn how alcohol affects your liver, the stages of alcohol-related liver disease, and key warning signs. Discover prevention tips, treatment options, and when to consult a liver specialist for timely care.

Introduction
Your liver is one of the hardest-working organs in your body, performing over 500 vital functions, including processing everything you eat and drink. But when alcohol enters the picture, it can place an immense and potentially dangerous burden on this crucial organ. Understanding the risk of alcohol-related liver diseases is the first step toward prevention and long-term health. This isn't just about chronic alcoholism; it's about the cumulative effect of regular drinking patterns that many might consider "social." This guide will walk you through how alcohol affects your liver, the stages of damage from simple fatty liver to life-threatening cirrhosis, and the key risk factors you need to know.
Understanding Your Liver: The Body's Detox Powerhouse
Before we dive into the risks, it's essential to understand the star of the show: your liver. Located in the upper right side of your abdomen, this reddish-brown organ is your body's primary filtration system.
What Does the Liver Actually Do?
Think of your liver as a sophisticated chemical processing plant. Its jobs include:
1. Detoxification: It filters your blood, breaking down harmful substances like alcohol, medications, and metabolic waste products.
2. Metabolism: It processes nutrients from the food you eat, converting them into energy and building blocks for your body.
3. Storage: It stores vitamins, minerals, and sugars to be released when your body needs them.
4. Bile Production: It produces bile, a fluid essential for digesting fats in your small intestine.
The liver is remarkably resilient and can regenerate itself. However, this ability has limits, especially when faced with a constant onslaught of toxins like alcohol.
Consult a Top Liver Specialist for Personalised Advice
How Alcohol Directly Attacks the Liver?
When you drink alcohol, your liver prioritises its breakdown above all else. It produces enzymes to convert alcohol into acetaldehyde, a highly toxic chemical and then into acetate, which is eventually eliminated. This process:
1. Generates harmful byproducts that damage liver cells.
2. Promotes inflammation.
3. Reduces the liver's ability to burn fat, leading to a buildup.
This direct attack is the starting point for all alcohol-related liver diseases. The risk escalates with the amount and duration of alcohol consumption. For those wondering about safe alcohol consumption limits, the answer is nuanced and depends on individual factors, which we'll explore next.
The Spectrum of Alcohol-Related Liver Damage
Alcohol-related liver disease (ARLD) progresses through three main stages. It's crucial to know that progression isn't inevitable; intervention at any stage can halt or even reverse damage.
Stage 1: Fatty Liver Disease (Hepatic Steatosis)
This is the earliest and most common stage, affecting over 90% of heavy drinkers. Fat accumulates inside liver cells, enlarging the organ.
1. Symptoms: Often, there are none, which is why it's so dangerous. Some people may feel tired or have mild discomfort in the upper right abdomen.
2. Outlook: The good news is that fatty liver from alcohol is reversible. Complete abstinence from alcohol for several weeks can allow the liver to heal and the fat to disappear.
Stage 2: Alcoholic Hepatitis
This stage involves inflammation and swelling of the liver, caused by years of drinking. "Hepatitis" means inflammation of the liver.
1. Symptoms: These can be more apparent and include loss of appetite, nausea, vomiting, abdominal pain, jaundice (yellowing of the skin and eyes), and fever.
2. Outlook: Alcoholic hepatitis can range from mild to severe. Mild cases can be reversed with abstinence. Severe, acute alcoholic hepatitis can develop suddenly and lead to life-threatening complications.
Stage 3: Cirrhosis and Liver Failure
This is the most severe stage, where prolonged inflammation causes irreversible scarring (fibrosis). Healthy liver tissue is replaced by scar tissue, which cannot function.
1. Symptoms: These indicate advanced liver diseases and include intense jaundice, swelling in the legs and abdomen (ascites), significant weight loss, and confusion.
2. Outlook: Cirrhosis is generally irreversible. However, stopping alcohol completely can prevent further damage and complications. In end-stage liver failure, a transplant may be the only option. The life expectancy with alcoholic cirrhosis varies greatly but is significantly reduced without abstinence.
Key Risk Factors: Are You in the Danger Zone?
Understanding your personal risk is critical. It's not just about how much you drink, but how, when, and who you are.
How Much Alcohol is Too Much?
Guidelines provide a framework, but it's important to remember that any amount of alcohol carries some risk. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), heavy drinking is defined as:
• For men: More than 4 drinks on any day or more than 14 drinks per week.
• For women: More than 3 drinks on any day or more than 7 drinks per week.
It's a common misconception that only daily heavy drinking is a problem. Binge drinking (4+ drinks for women, 5+ for men in about 2 hours) is also a major risk factor for liver disease.
Beyond Quantity: Patterns of Drinking That Increase Risk
1. Drinking on an Empty Stomach: This speeds up alcohol absorption.
2. Consistent Daily Drinking: Even moderate daily consumption can be riskier than occasional binge drinking for the liver due to constant exposure.
3. Starting Young: The earlier a person starts drinking regularly, the higher the lifetime risk.
Genetic and Biological Predispositions
1. Sex: Women are more vulnerable to alcohol-related liver damage. They have less body water to dilute alcohol and lower levels of the enzyme that breaks it down, leading to higher blood alcohol concentrations from the same amount of drink.
2. Genetics: Variations in genes that control alcohol metabolism can affect an individual's susceptibility.
3. Ethnicity: Some ethnic groups may have a higher predisposition to certain types of liver damage.
Other Health Conditions That Amplify Liver Risk
Your liver's health is interconnected with your overall health. Certain conditions can significantly increase the damage caused by alcohol.
The Dangerous Duo: Alcohol and Obesity
Both alcohol and obesity cause fat to build up in the liver. When combined, they have a synergistic effect, dramatically accelerating the progression from fatty liver to hepatitis and cirrhosis. This is a key reason why maintaining a healthy weight is crucial for liver health.
Alcohol and Viral Hepatitis (B & C)
Viral hepatitis infections already cause liver inflammation and scarring. Adding alcohol to the mix is like pouring gasoline on a fire, drastically speeding up the progression to cirrhosis and liver cancer. If you have hepatitis B or C, complete avoidance of alcohol is strongly recommended.
Recognising the Warning Signs of Liver Trouble
Liver disease is often called a "silent" illness because symptoms may not appear until significant damage has occurred. Knowing the early signs of alcoholic liver damage is vital.
Early Symptoms Often Missed
1. Persistent fatigue and weakness
2. Unexplained weight loss
3. Loss of appetite
4. Nausea
5. Discomfort or pain in the upper right abdomen
Signs of Advanced Liver Disease
1. Jaundice: Yellowing of the skin and the whites of the eyes.
2. Ascites: Swelling and fluid buildup in the abdomen.
3. Easy Bruising and Bleeding: The liver fails to produce enough proteins needed for blood clotting.
4. Confusion or Brain Fog (Hepatic Encephalopathy): Toxins build up in the brain.
If you experience any of these symptoms, especially jaundice or ascites, it is a medical emergency. Consult a doctor immediately. You can book a priority consultation online with a specialist on Apollo24|7 for an initial assessment.
Reducing Your Risk: Proactive Steps for Liver Health
The most effective way to prevent alcohol-related liver diseases is to limit or avoid alcohol. But there's more you can do.
Strategies for Cutting Back or Quitting
1. Set clear, realistic goals (e.g., "I will have three alcohol-free days this week").
2. Choose alcohol-free alternatives.
3. Avoid triggers that make you want to drink.
4. Seek support from friends, family, or professional groups if you find it difficult to cut down.
Liver-Healthy Diet and Lifestyle Choices
Eat a Balanced Diet: Focus on fruits, vegetables, lean proteins, and whole grains. Foods like coffee, nuts, and fatty fish have been associated with liver benefits.
1. Stay Hydrated: Drink plenty of water.
2. Exercise Regularly: This helps reduce liver fat and maintain a healthy weight.
3. Vaccinate: Get vaccinated against Hepatitis A and B.
4. Use Medications Wisely: Follow dosage instructions and avoid mixing medications with alcohol.
When to Seek Help: Diagnosis and Professional Support
If you are concerned about your risk or are experiencing symptoms, don't hesitate to seek medical advice. Diagnosis typically involves:
1. Blood Tests (Liver Function Tests - LFTs): These measure enzyme levels that indicate inflammation or damage. Apollo24|7 offers convenient home collection for these tests, making it easy to get checked.
2. Imaging Tests: An ultrasound, CT scan, or MRI can reveal fat accumulation, scarring, or physical changes to the liver.
3. Liver Biopsy: In some cases, a small sample of liver tissue may be taken for precise analysis.
A doctor can provide a formal diagnosis, discuss the stage of any potential liver diseases, and create a personalised treatment plan focused on abstinence, nutrition, and managing complications.
Get Your Health Assessed
Conclusion
The link between alcohol consumption and liver diseases is undeniable and serious. However, this guide underscores a message of hope: much of the risk is within your control. By understanding the stages of liver damage from reversible fatty liver to irreversible cirrhosis—and honestly assessing your personal risk factors, you are equipped to make informed decisions. The liver's incredible capacity to heal itself, especially in the early stages, means that it's never too late to take positive action. Whether it's committing to alcohol-free days, adopting a liver-friendly diet, or simply going for a walk, every small step counts. Your liver works tirelessly for you; returning the favour by minimising your alcohol intake is one of the most significant investments you can make in your long-term health. If you have concerns, remember that seeking professional advice early is always the best course of action.
Consult a Top Liver Specialist for Personalised Advice
Consult a Top Liver Specialist for Personalised Advice

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)
Dr. Sandeep Kudale
Paediatric Gastroenterologist
16 Years • MBBS,MD, DCH (Diploma in Child Health), MRCPCH (UK),Fellowship in Paediatric Hepatology and Liver Transplant , Fellowship in Paediatric Gastroenterology and Nutrition, FPGH (India)
Mumbai
Apollo Hospitals CBD Belapur, Mumbai
Consult a Top Liver Specialist for Personalised Advice

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)
Dr. Sandeep Kudale
Paediatric Gastroenterologist
16 Years • MBBS,MD, DCH (Diploma in Child Health), MRCPCH (UK),Fellowship in Paediatric Hepatology and Liver Transplant , Fellowship in Paediatric Gastroenterology and Nutrition, FPGH (India)
Mumbai
Apollo Hospitals CBD Belapur, Mumbai
More articles from Liver disease
Frequently Asked Questions
1. Can you drink alcohol with a fatty liver?
It is strongly advised to avoid all alcohol if you have been diagnosed with alcoholic fatty liver disease. Continued drinking can cause the condition to progress to the more serious stages of hepatitis and cirrhosis. Abstinence is the primary treatment for reversal.
2. How long does it take to get liver disease from drinking?
There is no fixed timeline, as it depends on the individual's consumption patterns, genetics, and overall health. Alcoholic fatty liver can develop in as little as a few years of heavy drinking. Progression to cirrhosis typically takes 10-20 years or more of sustained heavy drinking.
3. What are the first signs of liver damage from alcohol?
The earliest signs are often non-specific and easy to miss, including persistent fatigue, general malaise, and discomfort in the upper right abdomen. As damage progresses, clearer signs like jaundice (yellowing skin/eyes) appear.
4. Is alcoholic liver disease different from non-alcoholic fatty liver disease (NAFLD)?
Yes. While both result in fat in the liver, they have different primary causes. Alcoholic Liver Disease is caused by alcohol consumption. NAFLD is associated with metabolic issues like obesity and insulin resistance. However, drinking alcohol can worsen NAFLD.
5. What is the life expectancy with alcoholic cirrhosis?
Life expectancy varies widely and depends on factors like the severity of cirrhosis, whether the person stops drinking, and the presence of complications. Patients who achieve abstinence have a significantly better prognosis. For example, those with compensated cirrhosis (liver still functioning) who stop drinking can have a life expectancy extending over 10-12 years.