Guide to Diabetes And Liver All You Need To Know
Discover the essential link between diabetes and liver health, including risk factors, prevention tips, and strategies to maintain a healthy liver.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Introduction
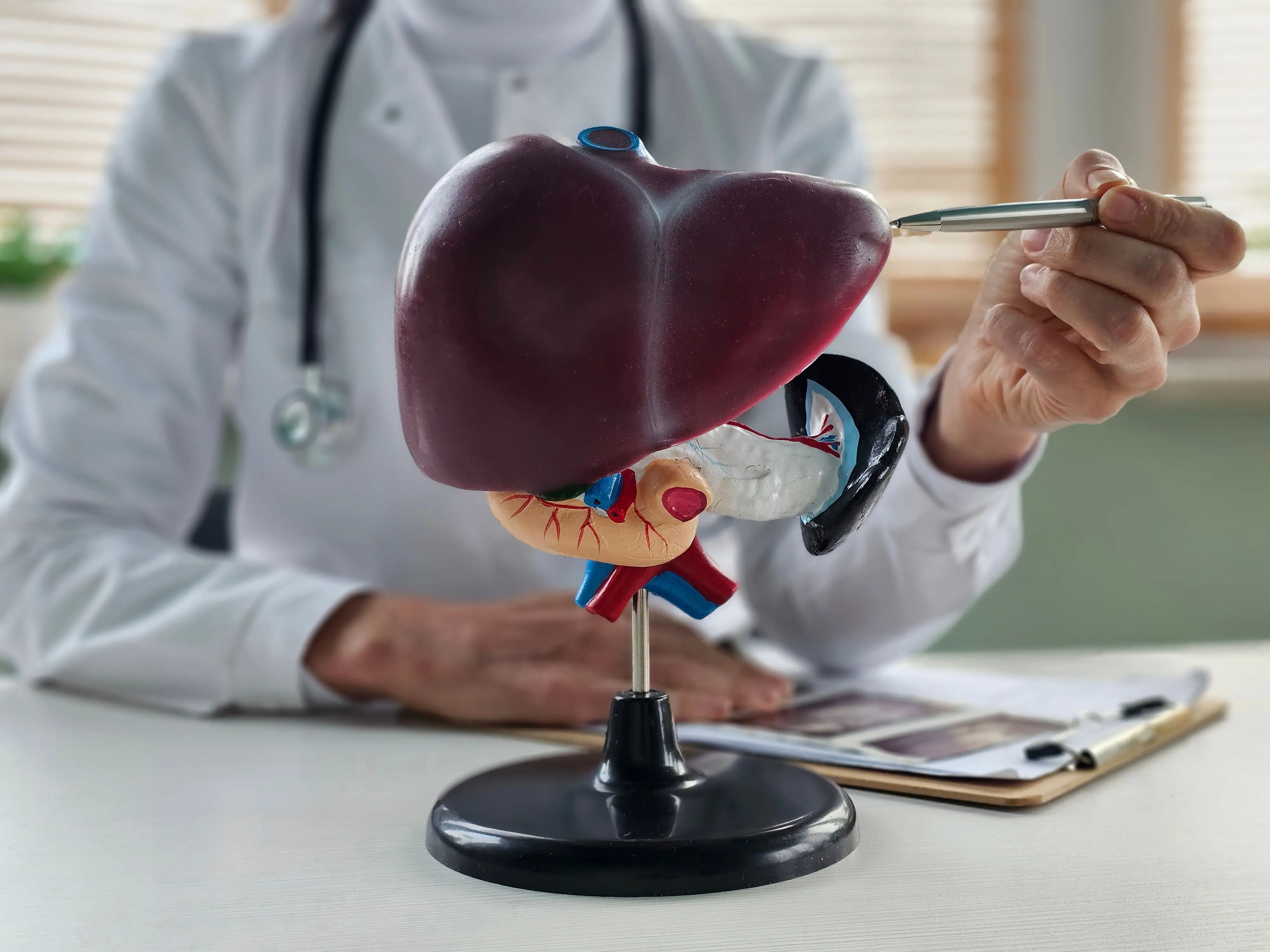
Living with diabetes involves managing more than just blood sugar levels. It requires a holistic understanding of how the condition affects your entire body, and one of the most critical yet often overlooked organs is the liver. This powerful organ acts as your body's processing plant, and when diabetes is in the picture, it can be placed under significant strain. The connection between diabetes and liver disease is strong and bidirectional; each condition can worsen the other. This comprehensive guide will demystify this complex relationship, exploring everything from the underlying mechanisms and common liver conditions to practical steps for diagnosis, management, and prevention. Whether you are newly diagnosed or have been managing diabetes for years, understanding your liver health is a non-negotiable part of your wellness journey.
The Critical Link: How Diabetes Affects Your Liver
Your liver and your pancreas are in constant communication, working together to manage your body's energy supply. When you have diabetes, this communication breaks down, primarily due to a condition known as insulin resistance. Understanding this link is the first step toward protecting your liver.
Understanding Insulin Resistance's Role
Insulin is a hormone that acts like a key, unlocking your cells to allow glucose (sugar) from your blood to enter and be used for energy. In type 2 diabetes, your cells become resistant to insulin. The pancreas compensates by producing even more insulin, leading to high levels of insulin in the blood (hyperinsulinemia). This excess insulin signals the liver to increase fat production. At the same time, the liver continues to release glucose into the bloodstream because it doesn't get the "stop producing glucose" signal properly. This double whammy increased fat production and increased glucose output is a primary driver of liver fat accumulation.
The Vicious Cycle of Diabetes and Liver Disease
This relationship creates a dangerous cycle. As fat builds up in the liver (a condition called steatosis), it makes the liver more inflamed and resistant to insulin. This worsened insulin resistance then makes blood sugar control more difficult, further exacerbating the diabetes. It’s a classic feedback loop where each condition fuels the progression of the other. Breaking this cycle is the cornerstone of effective management.
Common Liver Conditions Linked to Diabetes
Several specific liver diseases are intimately connected to diabetes. Knowing these conditions by name and understanding their progression is crucial.
Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD is the most common liver disorder in Western countries and is exceptionally prevalent among people with type 2 diabetes, affecting up to 70% of individuals. It is defined by the accumulation of excess fat in more than 5% of liver cells, not caused by alcohol consumption. In its early stages, NAFLD often has no symptoms and is largely reversible with lifestyle changes.
Non-Alcoholic Steatohepatitis (NASH)
A subset of NAFLD progresses to a more severe form called NASH. This is characterised by liver cell inflammation and damage, alongside the fat accumulation. Think of NAFLD as a simple fatty liver, while NASH is a fatty liver that has become inflamed and injured. This inflammation can lead to scarring (fibrosis). If your condition is diagnosed as NASH, it requires more aggressive management and monitoring.
Cirrhosis and Liver Cancer
Over time, persistent inflammation and scarring from NASH can lead to cirrhosis, where healthy liver tissue is replaced by scar tissue. This scar tissue impairs the liver's ability to function, which can lead to liver failure. Furthermore, having cirrhosis significantly increases the risk of developing hepatocellular carcinoma (HCC), a type of liver cancer. While not everyone with NAFLD will progress to cirrhosis or cancer, having diabetes substantially increases the risk.
Consult a Hepatologist for the best advice
Recognising the Signs: Symptoms of Liver Problems
Liver disease is often called a "silent" condition because symptoms may not appear until significant damage has occurred.
Early Warning Signs Often Missed
In the early stages of NAFLD and even NASH, there are typically no obvious symptoms. Some people may experience vague, non-specific signs that are easy to attribute to other issues, such as:
- Persistent fatigue or weakness
- Discomfort or mild pain in the upper right abdomen
When to Seek Immediate Medical Help
As liver disease advances to cirrhosis, symptoms become more pronounced and serious. If you experience any of the following, it is essential to consult a doctor promptly:
- Yellowing of the skin and eyes (jaundice)
- Swelling in the legs, ankles, or abdomen (ascites)
- Unexplained weight loss
- Itchy skin
- Dark urine
- Confusion or difficulty thinking
If symptoms like abdominal swelling or confusion develop, consult a doctor online with Apollo24|7 for further evaluation to determine the next steps.
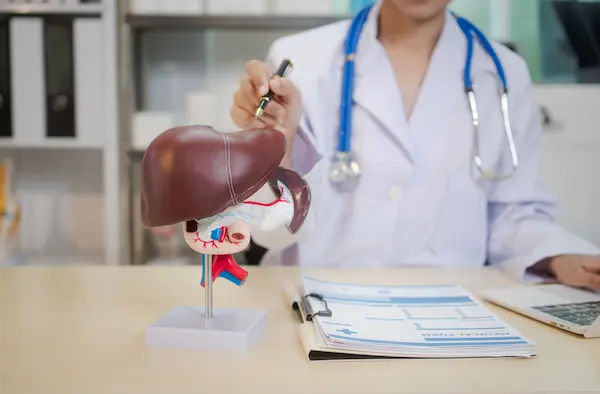
Diagnosis: How Liver Disease is Detected
Due to the lack of early symptoms, screening for liver disease is a critical part of diabetes care.
Key Blood Tests and What They Mean
Routine blood tests are the first line of defence.
- Liver Function Tests (LFTs): These measure enzymes like ALT (Alanine Transaminase) and AST (Aspartate Transaminase). Elevated levels can indicate liver inflammation or damage.
- HbA1c: This test provides a three-month average of your blood sugar levels, indicating how well your diabetes is
controlled.
Your doctor will interpret these results together. Apollo24|7 offers convenient home collection for tests like HbA1c and comprehensive liver function panels, making regular monitoring easier.
Imaging Tests: Ultrasound, FibroScan, and MRI
If blood tests suggest a problem, imaging is the next step.
- Ultrasound: A simple, painless test that can detect fat accumulation in the liver.
- FibroScan® (Transient Elastography): This specialised ultrasound measures liver stiffness, which correlates with the level of scarring (fibrosis). It's a non-invasive alternative to a biopsy.
- MRI: Can provide detailed images of the liver and quantify fat content.
Get Your Health Assessed
A Proactive Approach: Treatment and Management Strategies
The good news is that you can take control. The most effective treatment for NAFLD and early NASH is lifestyle modification, which also benefits your diabetes management.
Dietary Changes for a Healthier Liver
Diet is your most powerful tool. The goal is to reduce liver fat and improve insulin sensitivity.
Foods to Embrace
- High-Fibre Foods: Vegetables, fruits, legumes, and whole grains.
- Lean Protein: Fish (especially fatty fish like salmon rich in omega-3s), skinless poultry, tofu, and legumes.
- Healthy Fats: Avocados, nuts, seeds, and olive oil.
Foods to Avoid or Limit
- Added Sugars and Refined Carbs: Sugary drinks, pastries, white bread, and candy. These are major contributors to liver fat.
- Saturated and Trans Fats: Found in fried foods, red meat, and processed snacks.
- Alcohol: It's advisable to avoid alcohol completely, as it adds additional stress to the liver.
The Power of Physical Activity
Regular exercise helps your muscles use glucose for energy, improving insulin sensitivity and directly reducing liver fat. Aim for a combination of:
- Aerobic Exercise: At least 150 minutes per week of moderate-intensity activity (brisk walking, cycling, swimming).
- Resistance Training: At least 2 days per week (weight lifting, resistance bands).
Medications for Diabetes and Liver Health
While there are no FDA-approved medications specifically for NASH, some diabetes drugs have shown benefits for the liver.
- Pioglitazone: An insulin-sensitising drug that can reduce liver inflammation and fibrosis in people with NASH.
- GLP-1 Receptor Agonists (e.g., liraglutide, semaglutide): These drugs not only help with blood sugar control and weight loss but have also been shown to improve liver health in clinical trials.
- Vitamin E: An antioxidant that may be recommended for some non-diabetic adults with NASH, but its use must be discussed with a doctor due to potential risks.
Always consult your doctor before starting or changing any medication.
Conclusion
The relationship between diabetes and liver health is undeniable and demands your attention. However, it's not a predetermined path to poor health. By understanding the connection of how insulin resistance drives fat accumulation in the liver, you are empowered to take proactive steps. The same lifestyle strategies that are the cornerstone of good diabetes management, a whole-foods diet, regular physical activity, and maintaining a healthy weight are also your best defence against liver disease. This journey is about more than managing numbers; it's about nurturing your body's vital organs. Your liver is a resilient organ, and with the right care, you can protect it for years to come.
Consult a Hepatologist for the best advice
Consult a Hepatologist for the best advice

Dr. Pavan Kumar Y M
Gastroenterology/gi Medicine Specialist
5 Years • MBBS, MD Medicine, DM Gastroenterology
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. Srinivasa Reddy
Hepatologist
12 Years • MBBS, MD (General Medicine), DM (Hepatology),ASGE
Hyderabad
Myra Liver & Gastro Care, Hyderabad
Consult a Hepatologist for the best advice

Dr. Pavan Kumar Y M
Gastroenterology/gi Medicine Specialist
5 Years • MBBS, MD Medicine, DM Gastroenterology
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. Srinivasa Reddy
Hepatologist
12 Years • MBBS, MD (General Medicine), DM (Hepatology),ASGE
Hyderabad
Myra Liver & Gastro Care, Hyderabad
More articles from Liver disease
Frequently Asked Questions
1. Can you reverse fatty liver disease if you have diabetes?
Yes, in its early stages (NAFLD), fatty liver disease is often reversible. The most effective method is sustained weight loss of 5-10% of your total body weight through dietary changes and increased physical activity, which also improves blood sugar control.
2. What are the best foods to eat for a diabetic fatty liver?
Focus on a Mediterranean-style diet rich in vegetables, fruits, whole grains, lean proteins (especially fish), and healthy fats like those found in olive oil and nuts. This diet is naturally anti-inflammatory and helps manage both blood sugar and liver fat.
3. What is the difference between NAFLD and NASH?
NAFLD is simple fat accumulation in the liver, while NASH includes fat plus inflammation and liver cell damage. NASH is more serious because it can lead to scarring (fibrosis) and cirrhosis over time.
4. How often should someone with diabetes get their liver checked?
It's generally recommended that all adults with type 2 diabetes be screened for liver disease at diagnosis and regularly thereafter, typically annually. This usually involves a liver function blood test. Discuss the right screening schedule with your doctor.
5. Are there any specific symptoms of liver damage from diabetes?
In the early stages, there are usually no specific symptoms. As the disease progresses to advanced fibrosis or cirrhosis, symptoms like jaundice (yellowing skin), abdominal swelling, and unexplained weight loss may appear. This is why screening is so important before symptoms begin.