What Leads To Common Liver Problems? A Comprehensive Guide
Discover the main causes of common liver problems, including lifestyle choices, infections, and genetic factors. Learn how to recognise symptoms, prevent damage, and protect your liver health.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. Siri Nallapu MBBS
Last updated on 13th Jan, 2026
Introduction
Your liver is a remarkable organ, working tirelessly behind the scenes to keep you healthy. But when something goes wrong, the consequences can be severe. Many of us take our liver health for granted until a problem arises. This guide dives deep into the primary causes of common liver problems, moving beyond a simple list to explain the why and how. We'll explore everything from lifestyle choices and infections to genetic factors, empowering you with the knowledge to protect this vital organ. Understanding what leads to common liver issues is the first step toward prevention and long-term well-being.
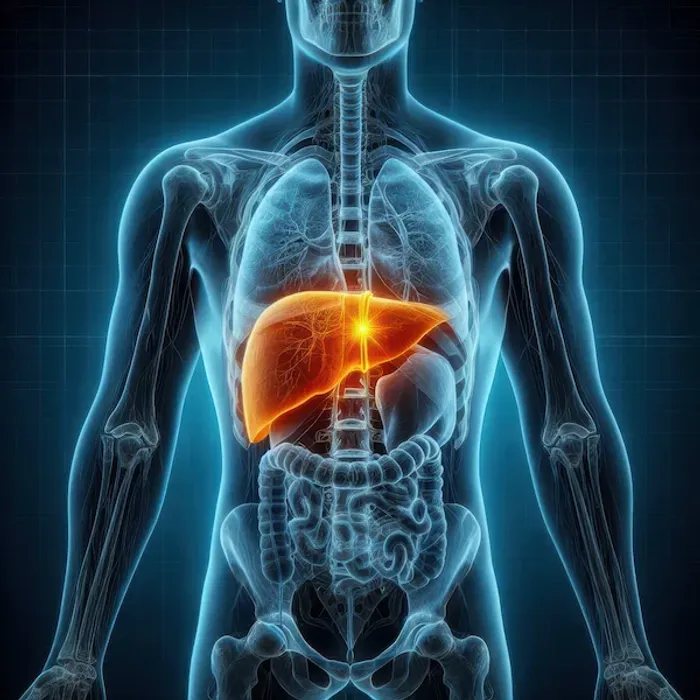
Understanding Your Liver: The Body's Silent Powerhouse
Before we examine what can go wrong, it's crucial to appreciate what the liver does right. Weighing about three pounds, it's your body's largest internal organ, acting as a sophisticated processing plant. Located in the upper right portion of your abdomen, it performs over 500 essential functions. Because the liver has a limited number of ways to signal distress, problems can often go unnoticed until they become significant. This is why understanding the causes of liver damage is so important for early intervention.
Key Functions of a Healthy Liver
A healthy liver is central to your metabolism and detoxification. Its key roles include:
Filtering Blood: It processes everything you eat, drink, and absorb through your skin, removing toxins like alcohol and environmental pollutants.
Bile Production: It produces bile, a fluid essential for digesting fats and absorbing fat-soluble vitamins (A, D, E, K).
Metabolising Nutrients: It converts nutrients from your food into essential blood components, stores vitamins and minerals, and regulates blood sugar by storing glucose as glycogen.
Protein Synthesis: It creates most of the proteins needed for blood clotting and other vital functions.
When any of these functions are impaired, it can lead to a cascade of health issues, making it critical to address the root causes of elevated liver enzymes and other signs of trouble.
The Top Culprits Behind Common Liver Diseases
Liver disease doesn't typically stem from a single source. Instead, it's often the result of one or more overlapping factors that persistently damage liver cells (hepatocytes). The most common culprits can be broadly categorised into lifestyle choices, infections, and other medical conditions. The relentless nature of this damage leads to inflammation (hepatitis), which, if left unchecked, can cause scarring (fibrosis) that progresses to permanent cirrhosis or even liver cancer. Identifying which category applies to you is key to formulating a prevention or treatment plan.
Lifestyle Factors: The Modern Assault on Liver Health
In today's world, our daily habits pose the most significant threat to liver health for the majority of people. The combination of poor diet, sedentary behaviour, and substance use creates a perfect storm for liver damage.
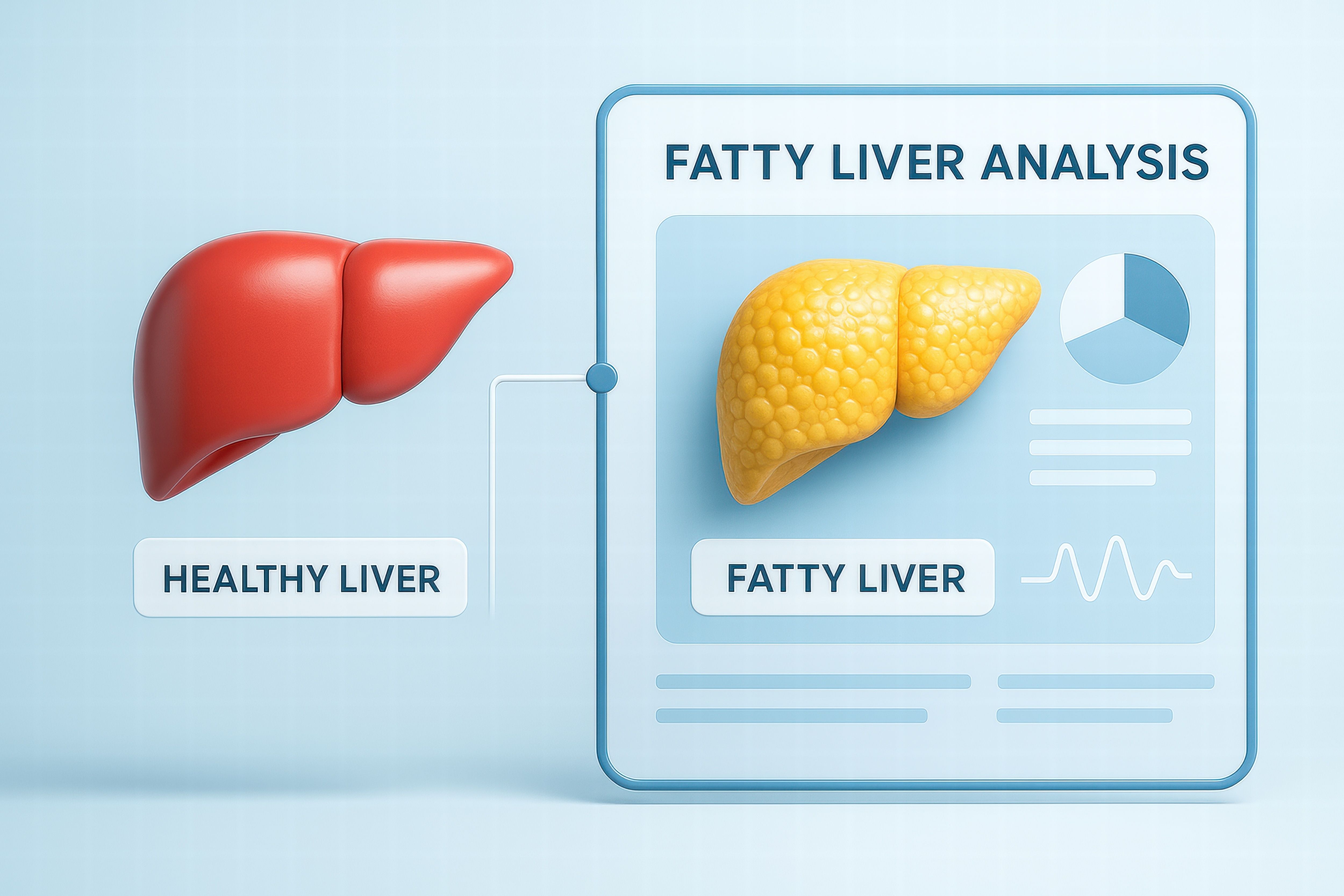
Non-Alcoholic Fatty Liver Disease (NAFLD): The Silent Epidemic
NAFLD is rapidly becoming the most common liver problem in Western countries, affecting an estimated 25-30% of the global population. It occurs when excess fat builds up in the liver cells of people who drink little to no alcohol. The primary driver is insulin resistance, often linked to:
Obesity and Overweight: Excess body fat, particularly around the abdomen, increases the amount of free fatty acids delivered to the liver.
High-Sugar, High-Fructose Diets: Sugary drinks and processed foods overwhelm the liver's ability to process fructose, leading to fat production and storage within the organ itself.
Type 2 Diabetes and High Cholesterol: These conditions are closely intertwined with NAFLD, creating a cycle of metabolic dysfunction.
The insidious part of NAFLD is that it often has no symptoms in its early stages. However, for some, it can progress to a more severe form called non-alcoholic steatohepatitis (NASH), involving inflammation and cell damage, which significantly raises the risk of cirrhosis. The good news is that early-stage NAFLD is often reversible through lifestyle changes.
The Direct Impact of Alcohol: Alcoholic Liver Disease
Alcohol is a direct toxin to liver cells. Alcoholic Liver Disease (ALD) encompasses a spectrum of conditions: fatty liver, alcoholic hepatitis, and cirrhosis. When you drink alcohol, your liver prioritises its metabolism over other functions. This process produces harmful by-products that damage liver cells, promote inflammation, and weaken your body's natural defences. The risk of ALD is directly related to the amount and duration of alcohol consumption. For men, consuming more than two drinks per day, and for women, more than one drink per day, significantly increases the risk. If you are concerned about your alcohol intake, consulting a doctor can provide guidance. If symptoms like unexplained weight loss or abdominal pain persist, consult a doctor online with Apollo24|7 for further evaluation.
Infections and Viruses: Hepatitis Explained
Viral infections are another major cause of liver inflammation, collectively known as hepatitis. Different viruses (hepatitis A, B, C, D, and E) have different modes of transmission and health implications.
Hepatitis A, B, and C: Transmission and Differences
Hepatitis A (HAV): Spread primarily through contaminated food or water. It typically causes an acute, short-term infection and does not lead to chronic disease. Vaccination is available and highly effective.
Hepatitis B (HBV): Transmitted through contact with infectious blood, semen, or other body fluids. It can be either acute or chronic. Chronic HBV is a major global health problem and a leading cause of liver cancer. Vaccination is available.
Hepatitis C (HCV): Primarily spread through contact with the blood of an infected person, most commonly through shared needles. Unlike HBV, most HCV infections become chronic. Until recently, treatment was difficult, but new antiviral medications can now cure over 95% of persons with HCV infection.
Understanding the difference between hepatitis A, B and C is critical for prevention and seeking appropriate medical care.
Health topic carousel:
Doctor's speciality: Nephrology
Text: Consult a Nephrologist for the best advice
Medications, Toxins, and Genetic Conditions
Beyond lifestyle and viruses, other factors can seriously impact liver health.
Over-the-Counter and Prescription Drug Risks
The liver processes most medications. Some drugs, even common over-the-counter ones like paracetamol (acetaminophen), can cause liver damage if taken in excess or combined with alcohol. Certain prescription medications, herbs, and supplements (e.g., high doses of vitamin A, kava) are also known to be hepatotoxic. It's essential to always follow dosage instructions and inform your doctor of all medications and supplements you are taking.
Inherited Liver Disorders
Some liver conditions are inherited. These include:
Haemochromatosis: A condition where the body absorbs and stores too much iron, which can build up to toxic levels in the liver.
Wilson's Disease: A rare disorder that causes a build-up of copper in the liver and other organs.
Alpha-1 Antitrypsin Deficiency: A genetic condition that can lead to lung and liver disease.
Recognising the Warning Signs of a Struggling Liver
Liver disease is often called a "silent" illness because symptoms may not appear until significant damage has occurred.
Early Symptoms Often Missed
Persistent fatigue and weakness
Loss of appetite
Nausea or vomiting
Mild abdominal discomfort or pain on the right side
Signs of Advanced Liver Damage
Jaundice: Yellowing of the skin and eyes.
Ascites: Swelling in the abdomen due to fluid build-up.
Easy Bruising or Bleeding: The liver fails to produce enough clotting proteins.
Dark Urine and Pale Stools.
Itchy Skin.
If you experience any signs of advanced liver damage, it is crucial to seek immediate medical attention. Apollo24|7 offers convenient home collection for tests like Liver Function Tests (LFTs) to help assess your liver health from home.
Proactive Steps: How to Protect and Heal Your Liver
The liver has an incredible ability to regenerate. By addressing the root causes, you can often prevent or even reverse early-stage damage.
Dietary Choices for Liver Detoxification
Focus on a balanced, whole-foods diet:
Increase: Fruits, vegetables, whole grains, lean proteins.
Limit: Sugary beverages, refined carbohydrates, processed foods, and saturated fats.
Hydrate: Drink plenty of water.
Coffee: Studies suggest moderate coffee consumption may be protective against liver fibrosis and cirrhosis.
The Role of Exercise and Weight Management
Regular physical activity helps reduce liver fat independently of weight loss. Aim for at least 150 minutes of moderate-intensity exercise per week. Even a 5-10% reduction in body weight can significantly improve liver health in individuals with NAFLD.
When to Seek Professional Help
Do not ignore persistent symptoms. If you have risk factors (obesity, diabetes, high alcohol intake, family history) or experience any warning signs mentioned above, it's time to see a doctor. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24|7 for a proper diagnosis, which may involve blood tests, imaging, or a liver biopsy.
Frequently Asked Questions (FAQs)
1. Can you reverse fatty liver disease?
Yes, in its early stages, Non-Alcoholic Fatty Liver Disease (NAFLD) is often reversible. The most effective strategy is lifestyle modification, including weight loss, a healthy diet low in sugar and processed foods, and regular exercise.
2. What are the first signs of a liver problem?
The earliest signs are often non-specific and can include persistent fatigue, weakness, loss of appetite, and mild nausea. Because these can be mistaken for other issues, it's important to see a doctor if they persist, especially if you have known risk factors.
3. How is hepatitis B different from hepatitis C?
Both can cause chronic infection, but they are different viruses. Hepatitis B is spread through bodily fluids (blood, semen), while Hepatitis C is spread primarily through blood-to-blood contact. Importantly, there is a vaccine to prevent Hepatitis B, but not for Hepatitis C.
4. Are liver function tests painful?
No, a Liver Function Test (LFT) is a simple blood test. A small blood sample is drawn from a vein in your arm, which may cause a brief pinch, but the procedure is not painful.
5. What is the best drink for liver health?
Water is the best choice. It helps the liver flush out toxins. Moderate coffee consumption has also been linked to protective benefits for the liver. It is crucial to avoid sugary drinks and limit alcohol significantly.
Conclusion
Understanding what leads to common liver problems empowers you to take control of your health. While factors like genetics and viruses play a role, the overwhelming majority of liver issues in the modern world are tied to manageable lifestyle choices. The journey to a healthier liver begins with conscious decisions about what you eat, how you move, and how you manage substances like alcohol and medications. Remember, your liver is a resilient organ. By providing it with the right support, you can significantly reduce your risk of disease and ensure it continues to perform its vital functions for years to come. Take the insights from this guide, assess your own habits, and take the first step toward proactive liver care today.
Health topic carousel:
Doctor's speciality: Nephrology
Text: Consult a Nephrologist for the best advice
Consult Top Specialists for Personalised Tips
Dr Ch Sashidhar
Nephrologist
20 Years • MBBS, MD General Medicine, DNB, Nephrology
Secunderabad
Apollo Hospitals Secunderabad, Secunderabad

Dr Praveen Kumar Etta
Nephrologist
10 Years • MBBS,MD DM(SGPGI) FORMER ASST(PIMS)
Hyderabad
Apollo Spectra Ameerpet, Hyderabad

Dr. Pardha Saradhi
Nephrologist
9 Years • MBBS, MD-DNB (Gen. Med.), DNB (Nephro)
Hyderabad
Apollo Hospitals D R D O kanchanbagh, Hyderabad
(75+ Patients)

Dr. Aswini Kumar Panigrahi
Nephrologist
23 Years • MBBS, MD (Int. Med.), DNB Nephro
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(225+ Patients)

Dr. Manju Kamal
Nephrologist
12 Years • MBBS,MD(General Medicine), DNB,DM(Nephrology)
Angamaly
Apollo Hospitals Karukutty, Angamaly
Consult Top Specialists
Dr Ch Sashidhar
Nephrologist
20 Years • MBBS, MD General Medicine, DNB, Nephrology
Secunderabad
Apollo Hospitals Secunderabad, Secunderabad

Dr Praveen Kumar Etta
Nephrologist
10 Years • MBBS,MD DM(SGPGI) FORMER ASST(PIMS)
Hyderabad
Apollo Spectra Ameerpet, Hyderabad

Dr. Pardha Saradhi
Nephrologist
9 Years • MBBS, MD-DNB (Gen. Med.), DNB (Nephro)
Hyderabad
Apollo Hospitals D R D O kanchanbagh, Hyderabad
(75+ Patients)

Dr. Aswini Kumar Panigrahi
Nephrologist
23 Years • MBBS, MD (Int. Med.), DNB Nephro
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(225+ Patients)

Dr. Manju Kamal
Nephrologist
12 Years • MBBS,MD(General Medicine), DNB,DM(Nephrology)
Angamaly
Apollo Hospitals Karukutty, Angamaly