A Woman’s Guide to Obesity: Risks, Causes, and Healthy Strategies
Explore how obesity impacts women’s hormones, fertility, and overall health — plus evidence-based tips for effective, healthy weight management.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026

Introduction
Obesity is a complex health issue that affects millions worldwide, but its impact on women is uniquely profound. Far beyond a number on a scale, obesity in women is intricately linked with hormonal balance, reproductive health, and long-term wellness. This guide delves deep into the relationship between obesity and women's health, moving past simplistic solutions to explore the root causes, significant risks, and empowering strategies for management. If you've ever felt that losing weight is a different, more challenging journey for you as a woman, you're not alone. Biological, psychological, and social factors create a distinct landscape. Here, we will unpack how conditions like PCOS and menopause influence weight, the very real threats to heart and metabolic health, and the importance of a compassionate, holistic approach to achieving a healthier you. This article is your comprehensive resource for understanding and taking charge of your well-being.
Understanding Obesity: More Than Just a Number
Obesity is classified as a chronic disease characterised by an excessive amount of body fat that presents a risk to health. It's a multifaceted condition influenced by genetics, environment, metabolism, and behaviour. For women, understanding this complexity is the first step toward effective management.
How is Obesity Measured? BMI and Beyond
The most common screening tool is body mass index (BMI), a calculation based on your height and weight. A BMI of 30 or higher typically falls into the obese category. However, BMI is a starting point, not a definitive diagnosis. It doesn't distinguish between muscle mass and fat mass. A more accurate assessment often involves measuring waist circumference, as abdominal or visceral fat—the fat stored deep within the abdomen—is particularly dangerous and strongly linked to metabolic syndrome and heart disease. For women, a waist circumference greater than 35 inches (88 cm) indicates increased health risk.
Why Obesity is Different for Women
Women's bodies are designed to store more fat than men's, primarily for reproductive purposes. This biological reality, driven by hormones like estrogen, means that women often have a higher essential body fat percentage. Furthermore, women experience significant hormonal shifts throughout their lives—during puberty, menstruation, pregnancy, and menopause—each of which can dramatically influence appetite, metabolism, and fat storage patterns. This makes the journey of weight management for women inherently different and often more challenging.
Consult a Specialist for the best advice
The Root Causes: Why Women are at Risk
Understanding the "why" behind weight gain is crucial for developing an effective response. The causes are rarely just about diet and exercise.
Hormonal Fluctuations and Their Impact
Hormones are the body's chemical messengers, and they play a starring role in regulating weight.
The Role of Estrogen and Leptin
Estrogen generally promotes the storage of fat on the hips and thighs (subcutaneous fat), which is less harmful than abdominal fat. However, when estrogen levels fluctuate or drop, as seen in perimenopause and menopause, fat storage often shifts to the abdomen. Leptin, the "satiety hormone," signals to your brain that you're full. Obesity can lead to leptin resistance, where the brain no longer responds to these signals, causing persistent overeating.
Lifestyle and Societal Factors
Modern lifestyles contribute significantly to obesity. Desk jobs, sedentary hobbies, and the easy availability of high-calorie, processed foods are major factors. For women, societal roles often mean juggling career, family, and household responsibilities, leaving little time for self-care, meal preparation, or regular exercise. Chronic stress, a common feature of this "juggling act," elevates cortisol levels, a hormone that can increase appetite and drive abdominal fat storage.
The Crucial Link: PCOS and Obesity
Polycystic ovary syndrome (PCOS) is a common hormonal imbalance affecting up to 10% of women of reproductive age. A key feature of PCOS is insulin resistance, where the body's cells don't respond effectively to insulin. This forces the pancreas to produce more insulin, which in turn promotes fat storage and makes weight loss extremely difficult. This creates a challenging cycle where obesity worsens PCOS symptoms, and PCOS promotes obesity. For many women, understanding this link is the key to unlocking effective strategies for managing weight with PCOS.
The Profound Impact on a Woman’s Body and Mind
The consequences of obesity extend far beyond physical appearance, affecting nearly every system in a woman's body.
Reproductive Health and Fertility Challenges
Obesity can disrupt the delicate balance of reproductive hormones, leading to irregular menstrual cycles and anovulation (lack of ovulation). This is a primary cause of female infertility. Conditions like PCOS are exacerbated by excess weight. Furthermore, obesity during pregnancy increases the risk of complications such as gestational diabetes, preeclampsia, miscarriage, and the need for a C-section.
Increased Risk of Chronic Diseases
Women with obesity have a significantly higher risk of developing serious health conditions:
Type 2 Diabetes: Insulin resistance is a direct precursor.
Heart Disease: Obesity raises blood pressure, negatively impacts cholesterol levels, and increases strain on the heart.
Certain Cancers: Postmenopausal breast cancer, endometrial cancer, and colon cancer have strong links to obesity.
Osteoarthritis: The extra weight places added stress on weight-bearing joints.
The Psychological Toll: Body Image and Mental Health
The social stigma surrounding weight can be devastating. Women often face immense pressure to conform to unrealistic body standards, leading to poor self-esteem, social anxiety, and depression. This can create a vicious cycle where emotional distress leads to emotional eating, further contributing to weight gain. Addressing mental well-being is therefore not a separate issue but a core component of managing obesity.
Taking Control: Sustainable Strategies for Weight Management
The goal is not rapid weight loss but sustainable, lifelong health. Fad diets don't work. Instead, focus on building healthy habits.
Building a Nourishing Diet Plan for Women
Shift from restriction to nourishment. Focus on whole foods: fruits, vegetables, lean proteins, whole grains, and healthy fats. Pay attention to portion sizes and practice mindful eating. For women with insulin resistance, a diet lower in refined carbohydrates and sugars can be particularly beneficial. If you need help creating a personalised plan, consulting a nutritionist via Apollo24|7 can provide tailored guidance.
Finding Joy in Movement: Exercise You Love
Exercise is about health, not punishment. Aim for a mix of activities:
Cardiovascular Exercise (brisk walking, swimming, cycling) for heart health.
Strength Training (weight lifting, resistance bands) is crucial for women. It builds muscle, which burns more calories at rest and combats age-related muscle loss.
Find activities you enjoy, so you're more likely to stick with them. Even small changes, like taking the stairs, add up.
The Power of Sleep and Stress Management
Prioritising 7-9 hours of quality sleep per night is non-negotiable. Poor sleep disrupts hunger hormones (ghrelin and leptin), increasing appetite. Similarly, managing stress through techniques like yoga, meditation, or simple deep-breathing exercises can help lower cortisol levels and reduce stress-related eating.
When to Seek Professional Help
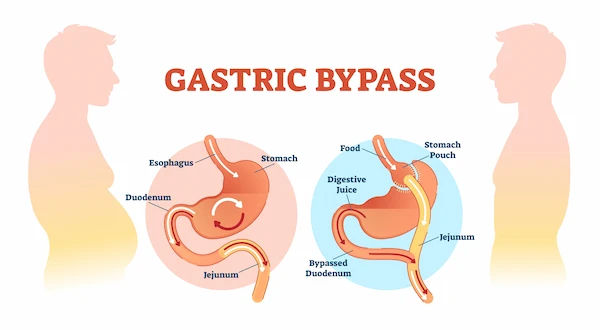
If you've struggled to lose weight despite your best efforts, or if you suspect an underlying condition like PCOS or thyroid issues, it's time to seek help. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24|7. They can order necessary tests (Apollo24|7 offers convenient home collection for tests like vitamin D or HbA1c) to check for hormonal imbalances, insulin resistance, or other metabolic issues. For some, treatments like medication or bariatric surgery may be considered under medical supervision.
Conclusion
Navigating obesity as a woman requires a compassionate and informed approach. It's essential to understand that the challenges are real and rooted in biology, not a lack of willpower. By focusing on the interconnectedness of hormones, lifestyle, and mental health, you can move beyond quick fixes and build a sustainable path to better health. Remember, small, consistent changes are far more powerful than drastic, short-lived measures. Your journey is unique, and seeking support—whether from healthcare professionals, loved ones, or credible resources—is a sign of strength. Take the first step today by committing to one positive change for your women's health. Your future self will thank you.
Consult a Specialist for the best advice
Consult a Specialist for the best advice

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)
Aditya Singh
Endocrinologist
8 Years • MBBS
Bengaluru
Apollo One Electronic City, Bengaluru

Dr. Usha Ayyagari
Endocrinologist
25 Years • MBBS, MRCP(UK), MRCP (Edin), CCT (UK), FRCP (London)
Chennai
Apollo Sugar Clinics, OMR, Chennai
(125+ Patients)

Dr. Chaithanya R
Internal Medicine Specialist Diabetologist
16 Years • MBBS, MD Internal Medicine, Fellowship in Diabetes(UK), CCEBDM(PHFI)
Bangalore
Apollo Clinic Bellandur, Bangalore
(75+ Patients)

Dr. Shruthi B
Endocrinologist
20 Years • MBBS,MD ( GEN MED) DM (ENDOCRIONOLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
More articles from Obesity
Frequently Asked Questions
1. What is a healthy BMI for a woman?
A BMI between 18.5 and 24.9 is generally considered healthy for adult women. However, BMI is a screening tool, not a direct measure of body fat. It's best to discuss your BMI and overall health profile with a doctor.
2. Can you reverse the health risks of obesity?
Yes, significantly. Even a modest weight loss of 5-10% of your total body weight can lead to major improvements in blood pressure, cholesterol levels, and insulin sensitivity, substantially reducing the risk of chronic diseases.
3. How does menopause affect weight?
Menopause causes a drop in estrogen, which can slow down metabolism and shift fat storage from the hips to the abdomen. This increase in visceral fat raises the risk of heart disease and diabetes. Managing weight during this stage often requires a renewed focus on strength training and a nutrient-dense diet.
4. What are the first steps to lose weight if I have PCOS?
The most effective first step for managing weight with PCOS is often addressing insulin resistance. This involves reducing intake of sugary foods and refined carbs, increasing fibre, and incorporating regular physical activity. Consulting a doctor or endocrinologist is highly recommended for a formal diagnosis and personalised plan.
5. Are there specific tests I should get if I'm struggling with obesity?
Yes. A doctor might recommend tests for fasting blood sugar and HbA1c (for diabetes risk), a lipid panel (for cholesterol), thyroid function tests (TSH), and tests for hormones like testosterone and prolactin if PCOS or other imbalances are suspected.