Are You Morbidly Obese? A Guide to Understanding Your Health
Know about the morbidly obese, what it is, connection with bmi, measurement of risk, causes, treatment options and more.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 13th Jan, 2026

Introduction
Are you concerned that your weight may be classified as morbidly obese? This term can sound alarming, but it's a specific medical diagnosis used to identify individuals at a significantly higher risk for serious health conditions. Understanding what it means is the first powerful step toward taking control of your well-being. This guide is designed not to frighten you, but to empower you with clear, factual information. We will break down the medical definitions, explain the associated health risks, and explore the various causes and, most importantly, the many effective treatment paths available.
What Does "Morbidly Obese" Actually Mean?
The term "morbidly obese" (now more clinically known as Class III obesity) is not a judgment on a person's character or willpower. It is a medical classification based on the Body Mass Index (BMI), a screening tool that correlates weight with height to categorize potential health risks. A diagnosis of morbid obesity indicates that an individual's excess body fat has reached a level that significantly increases the risk of developing obesity-related diseases, potentially leading to decreased life expectancy.
The Body Mass Index (BMI) Explained
BMI is calculated by dividing a person's weight in kilograms by the square of their height in meters (kg/m²). For adults, the Class III obesity threshold is a BMI of 40.0 or higher. It can also be defined as a BMI of 35.0 or higher in the presence of serious weight-related health conditions like type 2 diabetes or severe sleep apnea. While BMI is a useful population-level screening tool, it does have limitations—it doesn't distinguish between muscle and fat mass—which is why it's not the sole indicator of health.
Consult Dietician for Personalised Advice
Beyond the Scale: Other Ways to Measure Health Risk
BMI doesn't tell the whole story. Where you carry your weight is just as important as how much you weigh.
Waist Circumference and Waist-to-Hip Ratio
Visceral fat, which accumulates deep within the abdomen around vital organs, is particularly dangerous. A simple tape measure can be revealing. For women, a waist circumference greater than 35 inches (88 cm), and for men, greater than 40 inches (102 cm), indicates a higher risk of heart disease and type 2 diabetes, even if their BMI is in a lower category.
Body Composition and Visceral Fat
Two people can have the same BMI but vastly different health profiles based on their body composition (the ratio of fat, muscle, and bone). Advanced methods like bioelectrical impedance scales or DEXA scans can provide a more accurate picture of visceral fat levels, which are a major driver of metabolic complications. This is a key insight often missed: the location of your fat is a greater health predictor than the number on the scale alone.
The Health Risks of Morbid Obesity: More Than Just a Number
Morbid obesity is linked to a profoundly increased risk of developing over 50 different health problems. These aren't minor inconveniences; they are serious, life-altering conditions.
Cardiovascular and Metabolic Conditions
This category includes some of the most common and dangerous comorbidities. The risk of coronary heart disease, heart attack, and stroke rises dramatically. Morbid obesity is a primary driver of type 2 diabetes due to insulin resistance. It also significantly increases the likelihood of high blood pressure (hypertension) and unhealthy levels of cholesterol and triglycerides (dyslipidemia).
Impact on Joints, Mobility, and Respiratory Health
The skeletal system bears the brunt of excess weight. Osteoarthritis, particularly in the knees and hips, is extremely common due to the added stress on joints. This often leads to chronic pain and reduced mobility. Respiration is also affected, with conditions like sleep apnea (where breathing repeatedly stops and starts during sleep) and obesity hypoventilation syndrome being prevalent.
The Psychological and Emotional Toll
The impact is not solely physical. The social stigma, discrimination, and challenges with daily life can lead to depression, anxiety, low self-esteem, and social isolation. This creates a difficult cycle, as poor mental health can make it harder to adopt healthy habits. Acknowledging this emotional struggle is a critical part of holistic treatment for managing severe obesity.
Common Causes and Contributing Factors
Morbid obesity is rarely caused by a single factor. It is a complex disease resulting from a combination of genetic, physiological, environmental, and psychological influences.
Lifestyle, Diet, and Physical Inactivity
The modern environment, with its abundance of high-calorie, processed foods and sedentary lifestyles, is a major contributor. Consistent consumption of more calories than the body burns for energy leads to weight gain over time. A lack of regular physical activity exacerbates this energy imbalance.
Genetic, Hormonal, and Medical Factors
Science shows that genetics can influence how your body stores fat and how it regulates appetite. Hormones like leptin and ghrelin, which control hunger and satiety, can malfunction. Certain medical conditions, such as an underactive thyroid (hypothyroidism), Cushing's syndrome, and polycystic ovary syndrome (PCOS), can also make weight loss incredibly challenging.
The Role of Medications and Mental Health
Some prescription drugs, including certain antidepressants, antipsychotics, and corticosteroids, can lead to weight gain as a side effect. Furthermore, mental health conditions can influence eating behaviors, leading to emotional eating or binge eating disorder, which are significant causes of class 3 obesity.
Taking the First Step: How to Know for Sure
If you're concerned, the first step is objective assessment.
Calculating Your BMI at Home
You can use a reliable online BMI calculator from a reputable health source (like the NIH). Simply input your height and weight. Remember, this is a screening tool, not a diagnosis. A result of 40 or above places you in the Class III category.
The Importance of a Professional Medical Diagnosis
This is the most crucial step. A doctor is the only person who can provide an official diagnosis of morbid obesity. They will do more than calculate BMI. They will assess your overall health, measure your waist circumference, review your personal and family medical history, and screen for related conditions through blood tests (e.g., checking blood sugar and cholesterol levels). If you have calculated a high BMI at home, consult a doctor online with Apollo24|7 for a comprehensive evaluation and to discuss your health risks. Apollo24|7 also offers convenient home collection for tests like HbA1c and lipid profiles, which are essential for assessing metabolic health.
Treatment Paths and Managing Morbid Obesity
The good news is that morbid obesity is treatable. Treatment is not about quick fixes but sustainable, long-term strategies tailored to the individual.
Foundational Lifestyle Changes: Diet and Exercise
Under medical supervision, a structured program of dietary modification and increased physical activity is the cornerstone. This isn't about fad diets but a sustainable, nutrient-dense eating plan that creates a moderate calorie deficit. Similarly, exercise should be introduced gradually, focusing on low-impact activities initially to protect joints, with a goal of building up to 150+ minutes of moderate activity per week.
Medical Interventions: Weight-Loss Medications
For some individuals, lifestyle changes alone may not be sufficient. Several FDA-approved prescription medications can help manage appetite or reduce fat absorption. These are used as an adjunct to, not a replacement for, lifestyle changes and require ongoing supervision by a physician.
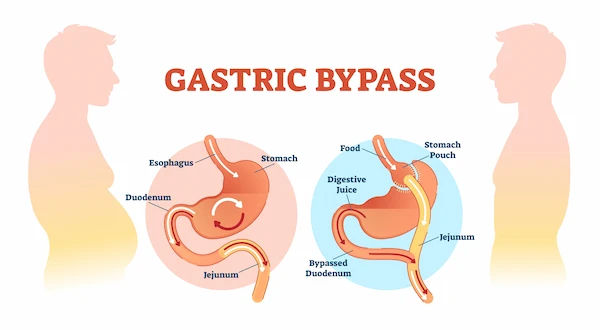
Bariatric Surgery: Types and Considerations
Bariatric surgery (e.g., gastric sleeve, gastric bypass) is the most effective long-term treatment for morbid obesity for suitable candidates. These procedures work by restricting food intake and/or altering gut hormones to reduce hunger and enhance satiety. They can lead to significant, sustained weight loss and remarkable resolution of comorbidities like diabetes.
The Critical Role of Behavioral Therapy and Support
Addressing the psychological relationship with food is often the key to lasting success. Behavioral therapy can help develop healthier coping mechanisms, improve self-esteem, and build the skills needed for long-term weight management. Support groups, either in-person or online, provide a community of understanding and accountability.
Conclusion
Understanding whether you fall into the category of morbid obesity is not about attaching a label, but about gaining clarity on your health landscape. It's a starting point for a transformative journey. While the associated risks are serious, they are not a foregone conclusion. Modern medicine offers a robust and multi-pronged approach to treatment, from lifestyle interventions and medication to highly effective surgical options. The path forward requires courage, support, and professional guidance. By taking that first step of seeking a medical opinion, you are choosing to invest in a healthier, more active, and fulfilling future.
Consult Dietician for Personalised Advice
Consult Dietician for Personalised Advice

Dr Venkata Naga Sai Tribhushan Rambhatla
General Physician
3 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Ms. Sushma Jaiswal
Dietician
42 Years • M.Sc.(Food & Nutrition)
Bengaluru
Swasthya Nutrition, Bengaluru

Ms. Suhita Sinha
Dietician
8 Years • BSC Food & Nutrition
Kolkata
Chikitsa Medicare Centre Pvt. Ltd.Sattelite Centre Behala Chowrasta, Kolkata

Ms. Neelanjana J
Dietician
5 Years • Bsc., Msc. Nutrition and Dietetics specialised general weight management, PCOS/PCOD weight loss and Diabetes management. A clinical dietitian with 4+ year experience specializing in evidence-based, result-oriented nutrition therapy. I have extensive experience in weight loss, thyroid management, PCOD/PCOS, weight gain, and diabetes & prediabetes care. My approach is personalized, practical, and sustainable—focusing on helping individuals achieve long-term lifestyle change rather than quick fixes. I work closely with clients to understand their medical history, lifestyle, and goals, and then design customized diet plans that support hormonal balance, metabolic health, and overall wellbeing. My goal is to make nutrition simple, realistic, and effective—so you see measurable results and feel your healthiest self.Auther in Health benefits of jackfruit (Artocarpus heterophyllus Lam.) seeds: A review (2023) The Pharma Innovation Journal Co- Auther in Malnutrition in Women: A review (2023) The Pharma Innovation Journal. Highfield Level 3 in HACCP. Highfield Level 4 International Award in Food Safety Managment
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Ms. Sreeparna Dey Dhara Deb
Dietician
10 Years • DNHE
Bansdroni
Siddhita Healthcare., Bansdroni
More articles from Obesity
Frequently Asked Questions
1. What is the life expectancy of someone with morbid obesity?
Studies suggest that Class III obesity can reduce life expectancy by an estimated 6 to 14 years due to the heightened risk of fatal conditions like heart disease and cancer. However, this is an average, and significant weight loss, even a 5-10% reduction, can dramatically improve health metrics and longevity.
2. Can you be morbidly obese and still healthy?
The concept of 'metabolically healthy obesity' is debated. While some individuals with a high BMI may not have immediate metabolic issues (like high blood pressure), the excess weight still places immense strain on joints and the respiratory system. The long-term risk of developing serious conditions remains significantly higher than for someone in a healthy weight range.
3. What qualifies you for weight loss surgery?
General qualifications include having a BMI of 40 or higher, or a BMI of 35-39.9 with a serious obesity-related health condition (e.g., type 2 diabetes, hypertension). Candidates must also have previously attempted weight loss through diet and exercise and be committed to lifelong lifestyle changes and medical follow-up.
4. How fast can you lose weight if you are morbidly obese?
Safe and sustainable weight loss is typically 1-2 pounds per week initially. With significant changes, someone with morbid obesity may lose weight more rapidly at the very start, but a gradual pace is better for preserving muscle mass and preventing rebound weight gain. Medical supervision is crucial.
5. Is morbid obesity a disability?
In many countries, morbid obesity itself is not automatically classified as a disability. However, if it leads to physical or mental impairments that significantly limit one or more major life activities (e.g., walking, breathing, working), it may be covered under disability anti-discrimination laws. Legal definitions vary.