Osteoarthritis: Symptoms, Treatment And Daily Care
Learn about osteoarthritis symptoms, risk factors, diagnosis, treatments, exercises, medications, and surgery options. Practical tips for daily living and long-term joint health.


Introduction
If your knees ache after a short walk or your fingers feel stiff when you wake up, osteoarthritis might be on your mind. Osteoarthritis is the most common form of arthritis—a degenerative joint condition where cartilage gradually wears down, bones remodel, and low-grade inflammation contributes to pain and stiffness. It most often affects the knees, hips, hands, and spine, but any joint can be involved. The good news is that while osteoarthritis cannot be “cured,” there is much you can do to slow progression, ease pain, and stay active.
In this guide, you’ll learn what osteoarthritis is and how it differs from other types of arthritis, who is at risk and why, and the symptoms to watch for. We will cover how doctors diagnose osteoarthritis and the full range of treatments—from exercise and weight management to medications, injections, and surgery when needed. You’ll also get practical tips for daily living, including sleep, work, and flare management. Along the way, plain-language explanations and examples help you understand research and guideline recommendations you can apply today.
What Is Osteoarthritis?
Here's what you need to know about this common joint condition:
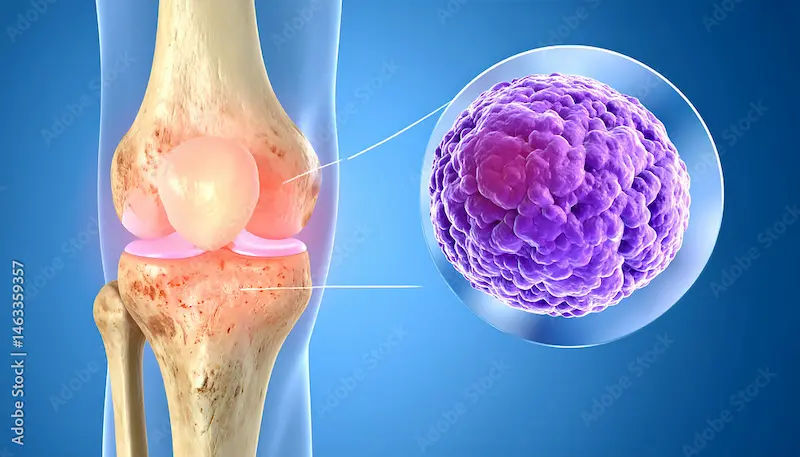
Osteoarthritis is a chronic joint condition characterised by gradual cartilage breakdown, thickening of the bone beneath, growth of bone spurs, changes in ligaments and menisci, and low-grade inflammation of the joint lining. Together, these changes cause pain, stiffness, decreased range of motion, and sometimes swelling. Unlike autoimmune arthritis, osteoarthritis is primarily a mechanical and biological “wear, repair, and remodel” process, influenced by age, load, and genetics.
How osteoarthritis differs from arthritis in general
- Arthritis is a broad term for joint inflammation. Osteoarthritis is the degenerative, most common type, distinct from inflammatory types such as rheumatoid arthritis or psoriatic arthritis.
- OA tends to be asymmetric and joint-specific; morning stiffness is usually under 30 minutes, while inflammatory arthritis stiffness lasts longer.
- OA often worsens with joint use and improves with rest, unlike rheumatoid arthritis, which often improves with activity once joints are warmed.
Consult Top Specialists
The biology of cartilage wear, bone changes, and inflammation
- Cartilage loses its smooth surface and cushioning properties; the underlying bone becomes denser and forms spurs; the joint lining may become mildly inflamed.
- Pain originates from multiple tissues including bone, synovium, ligaments, and surrounding muscles, highlighting why strengthening and load management are crucial.
Who gets osteoarthritis?
- Osteoarthritis affects hundreds of millions globally, being a leading cause of disability in older adults.
- It is more common with age but not merely a consequence of ageing. Prior injuries, obesity, and occupational stresses are major contributors.
Causes and Risk Factors
Here's what contributes to osteoarthritis:
Age, genetics, and sex differences
- Age increases cumulative joint loading and reduces tissue repair efficiency. Genetics play a role, with family history raising risk.
- Women have higher risk after midlife, possibly due to hormonal and anatomical factors, and are more likely to develop hand and knee OA.
Weight, joint loading, and previous injuries
- Excess body weight increases load across weight-bearing joints; losing 5–10% of body weight can significantly reduce knee pain and improve function.
- Previous joint injuries, such as ACL tears or meniscal damage, increase osteoarthritis risk by altering biomechanics.
Occupation, sports, and biomechanical factors
- Repetitive kneeling, squatting, heavy lifting, or vibration exposure at work increases knee and hip OA risk.
- High-impact sports or poor training techniques accelerate joint stress, whereas cycling and swimming are protective.
Metabolic factors
- Metabolic syndrome, type 2 diabetes, and dyslipidaemia are linked to OA, possibly through systemic inflammation and altered cartilage metabolism.
Symptoms and When to See a Doctor
Here's how osteoarthritis may present:
Common signs by joint
- Knee: activity-related pain, stiffness after sitting, grinding, occasional swelling, reduced flexion.
- Hip: groin or buttock pain, pain with walking and turning, reduced internal rotation.
- Hand: bony nodules at finger joints, thumb base pain, grip weakness.
- Spine: neck or lower back stiffness and pain, often fluctuating.
Red flags needing urgent evaluation
Sudden hot, swollen joint with fever, severe new pain after injury, rapidly progressive weakness or numbness, or unexplained weight loss.
Osteoarthritis vs rheumatoid arthritis
- OA: shorter morning stiffness, asymmetric, localized, worsens with use.
- RA: prolonged morning stiffness, symmetrical swelling, systemic features.
If symptoms persist beyond two weeks or you are unsure, consult a doctor online with Apollo24|7.
Diagnosis and Tests
Here's what doctors look for:
Clinical exam and functional assessment
- Diagnosis is often clinical: symptom patterns, risk profile, and exam findings. Functional tests track impact.
Imaging
- X-ray: shows joint space narrowing, bone spurs, and subchondral sclerosis. Severity on X-ray does not always match pain.
- MRI: used selectively for meniscal tears, bone marrow lesions, or early cartilage changes.
- Ultrasound: assesses effusions and guides injections.
Lab tests
Blood tests like ESR, CRP, rheumatoid factor, anti-CCP, and uric acid help rule out other conditions. Apollo24|7 offers convenient home collection.
Staging and tracking progression
Radiographic grading and patient-reported outcomes help monitor changes over time. Tracking pain, function, and activity is as important as imaging.
Non-Surgical Treatment and Self-Management
Here's how to manage osteoarthritis without surgery:
Exercise therapy
Strength training (quadriceps, hip abductors), aerobic activity, balance, and flexibility improve symptoms. Aim for 150 minutes/week of moderate activity plus 2 days of strength training.
Weight loss and load management
Losing 5–10% of body weight can significantly reduce knee pain. Use trekking poles, level paths, and joint-friendly cardio.
Physical therapy, braces, footwear, and assistive devices
PT teaches joint-protective movement patterns. Unloader braces help alignment; cushioned footwear and lateral wedges may reduce knee load. Canes in the opposite hand are beneficial.
Heat, cold, pacing, and flare management
Heat for stiffness, ice after activity. Use pacing strategies and temporary rest during flares.
Medications and Injections
Here's what may help with pain:
Topical and oral pain relievers
Topical NSAIDs for knees and hands have lower systemic risk. Oral NSAIDs help but carry gastrointestinal, kidney, and cardiovascular risks. Acetaminophen has modest benefit.
Duloxetine
Can assist chronic pain with central sensitisation or comorbid anxiety/depression. Requires medical oversight.
Injections
Corticosteroids provide short-term relief. Hyaluronic acid has mixed results. PRP is emerging with evolving evidence.
Supplements
Glucosamine and chondroitin show inconsistent benefits; turmeric/curcumin may offer mild pain relief. Always review with a clinician.
If symptoms do not improve, book a physical visit to a doctor with Apollo24|7.
Procedures and Surgery
Here's when surgical options are considered:
Arthroscopy
Not routinely recommended for degenerative knee OA, except for mechanical locking from a meniscal tear.
Osteotomy
For younger patients with unicompartmental OA and malalignment to redistribute load.
Joint replacement
Total hip or knee replacement provides dramatic pain relief and restored function when conservative care fails. Partial replacements may suit select patients.
Rehabilitation
Prehab improves outcomes; post-surgery rehab focuses on pain control, range of motion, strength, and gait retraining. Adherence to home exercises is crucial.
Living Well with Osteoarthritis
Here's how to manage daily life:
Sleep, stress, and mental health
Maintain sleep hygiene and consider mind-body practices like yoga or tai chi.
Ergonomics and pacing
Adjust workstations, take micro-breaks, rotate tasks, and use supportive tools.
Building a care team
Include primary care, physiotherapy, dietitian, and orthopaedic specialists. Track pain, activity, and progress.
Preventing future joint problems
Maintain strength, flexibility, healthy weight, and balance training. Treat injuries early.
Conclusion
Osteoarthritis may be common, but it is not inevitable or untreatable. Understanding joint changes—cartilage wear, bone remodelling, and low-grade inflammation—explains why a whole-joint approach is effective. Movement, strength training, weight management, load management, supportive footwear, and smart pacing form the foundation of care.
Medications, injections, and surgery provide additional relief when necessary, with success strongly influenced by rehabilitation, sleep, and consistent habits. Begin with small steps such as a daily walk, chair rises, or stretching, and monitor your progress. If symptoms persist beyond two weeks, consult a doctor online with Apollo24|7. Home collection for tests like ESR, CRP, or uric acid is available if required. With the right plan and support, living well with osteoarthritis is achievable.
Consult Top Specialists
Consult Top Specialists

Dr. Anil Pradeep Jadhav
Orthopaedician
23 Years • MBBS MS (Ortho)
Nashik
Apollo Hospitals Nashik, Nashik
(25+ Patients)

Dr. Suraj Prakash
Orthopaedician
5 Years • MBBS, MS (Ortho)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru

Dr. Padam Singh Gautam
General Physician/ Internal Medicine Specialist
43 Years • M.B.B.S (WARDHA M. S.), F.A.G.E. (MANIPAL), F.A.I.M.S. (Pb.), M.A.I.M.S. (Pb.), M.R.S.H. (LONDON)
Noida
Dr Padam Singh Gautam Fracture Clinic, Noida

Dr. Susheel B
Orthopaedician
13 Years • MBBS, MS, Ortho Fellowship in Trauma ( Germany) Fellowship in Arthroscopy and Arthroplasty ( Switzerland)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Prof. Dr. Jambu N
Orthopaedician
23 Years • MBBS, M.S Ortho, FRCS ,FACS
Chennai
Apollo Speciality Hospitals Vanagaram, Chennai
(150+ Patients)
Consult Top Specialists

Dr. Anil Pradeep Jadhav
Orthopaedician
23 Years • MBBS MS (Ortho)
Nashik
Apollo Hospitals Nashik, Nashik
(25+ Patients)

Dr. Suraj Prakash
Orthopaedician
5 Years • MBBS, MS (Ortho)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru

Dr. Padam Singh Gautam
General Physician/ Internal Medicine Specialist
43 Years • M.B.B.S (WARDHA M. S.), F.A.G.E. (MANIPAL), F.A.I.M.S. (Pb.), M.A.I.M.S. (Pb.), M.R.S.H. (LONDON)
Noida
Dr Padam Singh Gautam Fracture Clinic, Noida

Dr. Susheel B
Orthopaedician
13 Years • MBBS, MS, Ortho Fellowship in Trauma ( Germany) Fellowship in Arthroscopy and Arthroplasty ( Switzerland)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Prof. Dr. Jambu N
Orthopaedician
23 Years • MBBS, M.S Ortho, FRCS ,FACS
Chennai
Apollo Speciality Hospitals Vanagaram, Chennai
(150+ Patients)
More articles from Osteoarthritis
Frequently Asked Questions
What are the early signs of osteoarthritis?
Early signs include activity-related joint pain, brief morning stiffness, and mild swelling. In the hands, small bony bumps may appear. If you notice early signs of osteoarthritis that persist, seek medical advice.
What’s the difference between osteoarthritis vs rheumatoid arthritis?
Osteoarthritis pain worsens with use and morning stiffness is usually short. Rheumatoid arthritis often causes longer stiffness, symmetrical swelling, and systemic symptoms. Blood tests and imaging help tell them apart.
What are the best exercises for osteoarthritis?
Low-impact cardio (walking, cycling, swimming), strength training (legs/hips/core), balance, and flexibility. A physical therapist can tailor a non-surgical treatment for osteoarthritis to your needs.
Do hyaluronic acid injections work for knee osteoarthritis?
Results are mixed: some feel relief, others don’t. Many guidelines are neutral or cautious about routine use. Discuss with your clinician whether hyaluronic acid injections for knee osteoarthritis fit your case.
When should I consider joint replacement for osteoarthritis?
Consider it if pain and disability remain high despite optimised conservative care (exercise, weight loss, medications/injections), and X-rays show significant joint damage. A specialist can review benefits and risks.

.webp)
