Understanding Osteoarthritis Symptoms, Causes, and Management
Learn about osteoarthritis symptoms, causes, risk factors, treatment options, and daily management tips to maintain mobility and joint health.

Written by Dr. Siri Nallapu
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026
Introduction
Osteoarthritis (OA) is more than just occasional joint pain; it's the most common chronic condition affecting the joints, impacting millions of adults worldwide. Often called "wear and tear" arthritis, osteoarthritis occurs when the protective cartilage that cushions the ends of your bones wears down over time. This can lead to pain, stiffness, swelling, and a decreased ability to perform everyday activities. While any joint can be affected, it most commonly impacts the hands, knees, hips, and spine. This comprehensive guide will walk you through everything you need to know about osteoarthritis, from recognising the early warning signs and understanding your risk factors to exploring effective treatment options and practical daily management strategies. Our goal is to empower you with knowledge to better manage your joint health and maintain your quality of life.
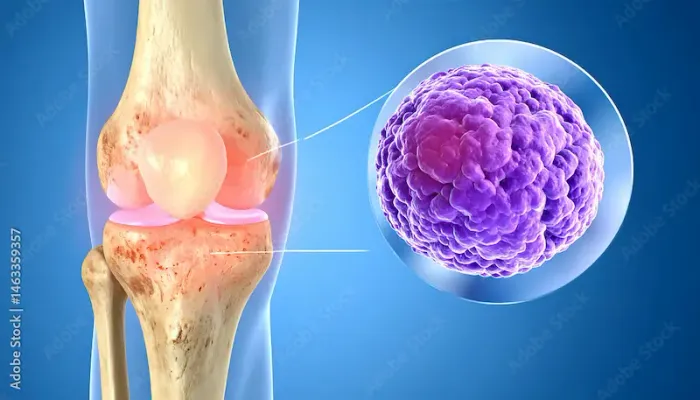
What is Osteoarthritis? The "Wear and Tear" Arthritis Explained
At its core, osteoarthritis is a degenerative joint disease. To understand it, picture a healthy joint: the ends of your bones are covered in a smooth, slippery tissue called articular cartilage. This cartilage allows bones to glide against each other with minimal friction and acts as a shock absorber. In OA, this cartilage gradually breaks down. As it wears thin, the bone underneath becomes exposed and can start to thicken. The joint may try to repair itself, leading to the growth of new bone at the edges of the joint (osteophytes), which are often visible as bone spurs on an X-ray. Furthermore, the synovium (the lining of the joint) can become inflamed, and the amount of synovial fluid (which lubricates the joint) can increase, causing swelling. This entire process changes the joint's structure, leading to the classic symptoms of pain, stiffness, and loss of mobility. It's crucial to remember that while ageing is a primary risk factor, osteoarthritis is not an inevitable part of getting older; it's a complex disease influenced by genetics, mechanics, and inflammation.
Recognising the Signs; Common Osteoarthritis Symptoms
The symptoms of osteoarthritis develop slowly and worsen over time. They can vary greatly from person to person, and not everyone with OA will experience all symptoms.
Early-Stage Symptoms
In the beginning, you might only feel pain in a joint after intense activity or at the end of the day. The most common early signs include:
• Pain: Aching or sharp pain during or after movement.
• Stiffness: Joint stiffness is most noticeable upon waking up in the morning or after a period of inactivity, but it typically lasts for less than 30 minutes.
• Tenderness: The joint may feel tender when you apply light pressure to it.
Progressive Symptoms
As the condition advances, symptoms become more persistent and pronounced:
• Loss of Flexibility: You may not be able to move the joint through its full range of motion.
• Grating Sensation: You might hear or feel a popping or crackling sound (crepitus) when you use the joint.
• Bone Spurs: Extra bits of bone, which feel like hard lumps, can form around the affected joint.
• Swelling: This can be caused by soft tissue inflammation around the joint.
If you are experiencing persistent joint pain and stiffness that doesn't improve with rest, it's important to seek a professional opinion.
Who is at Risk? Key Osteoarthritis Risk Factors
Certain factors make you more susceptible to developing osteoarthritis. These are divided into factors you cannot change and those you can influence.
Unmodifiable Risk Factors (Age, Gender, Genetics)
• Age: The risk of OA increases significantly after age 50.
• Gender: Women are more likely than men to develop OA, especially after menopause.
• Genetics: A family history of OA can predispose you to the condition.
• Bone Deformities: Some people are born with malformed joints or defective cartilage.
Modifiable Risk Factors (Weight, Injury, Occupation)
• Obesity: Excess body weight is one of the most significant modifiable risk factors. It adds stress to weight-bearing joints like hips and knees. Furthermore, fat tissue produces proteins that can cause harmful inflammation in and around your joints.
• Joint Injuries: Injuries from sports, accidents, or falls, even those that occurred years ago and seemed to heal, can increase your risk of osteoarthritis in that joint.
• Certain Occupations: Jobs that involve repetitive stress on a particular joint (e.g., kneeling for plumbing, heavy lifting in construction) can lead to the development of OA over time.
How is Osteoarthritis Diagnosed?
Diagnosing OA typically involves a multi-step process to confirm the condition and rule out other types of arthritis, like rheumatoid arthritis.
The Doctor's Visit: Medical History and Physical Exam
Your doctor will start by asking about your symptoms, their severity, and how they affect your daily life. They will also perform a physical examination of the affected joint, checking for tenderness, swelling, range of motion, and any instability.
Imaging Tests: X-rays and MRIs
• X-rays: These are the most common tool. They can reveal a narrowing of the space between bones in a joint (a sign of cartilage loss), bone spurs, and other bone changes. However, X-rays often don't show early cartilage damage.
• MRI (Magnetic Resonance Imaging): An MRI uses radio waves and a strong magnetic field to produce detailed images of bone and soft tissues, including cartilage. This can help identify damage earlier than an X-ray.
Lab Tests: Ruling Out Other Conditions
While there is no blood test for OA, your doctor might order them to rule out other causes of joint pain, such as rheumatoid arthritis. Analysing fluid from an inflamed joint (arthrocentesis) can also help confirm a diagnosis by checking for inflammation or infection. Apollo24|7 offers convenient home collection for tests like ESR or CRP, which are often used in this diagnostic process.
Effective Osteoarthritis Treatment Strategies
There is no cure for OA, but a combination of treatments can effectively reduce pain and maintain joint function, helping you stay active. The approach is always tailored to the individual's needs.
Lifestyle Modifications and Home Remedies
These are often the first and most important steps in managing osteoarthritis.
Weight Management and Exercise
Losing even a small amount of weight can significantly reduce stress on weight-bearing joints. Exercise is critical, it strengthens the muscles around the joints, increases flexibility, and reduces pain. Low-impact activities like swimming, cycling, and walking are excellent choices.
Heat and Cold Therapy
Applying a heating pad can relax muscles and ease stiffness. Cold packs applied to the sore joint for 15-20 minutes can numb pain and reduce inflammation after activity.
Medications for Pain and Inflammation
• Oral Pain Relievers: Paracetamol can help with mild to moderate pain.
• NSAIDs: Non-steroidal anti-inflammatory drugs like ibuprofen or naproxen, available over-the-counter or in stronger prescription doses, help reduce both pain and inflammation.
• Topical Creams: Gels and creams containing NSAIDs or capsaicin can be applied directly to the skin over the painful joint.
Physical and Occupational Therapy
A physiotherapist can teach you exercises to strengthen muscles, increase your range of motion, and reduce pain. An occupational therapist can show you how to perform daily tasks like housework or grooming, in ways that are easier on your joints.
Consult an Orthopaedician for the best advice
Surgical Interventions: When Are They Considered?
Surgery is usually reserved for severe osteoarthritis that hasn't responded to other treatments. Options include:
• Joint Realignment (Osteotomy): Cutting and reshaping the bones to relieve pressure on the joint.
• Joint Replacement (Arthroplasty): The damaged joint surfaces are removed and replaced with plastic and metal parts. This is most commonly done for hips and knees and can dramatically improve quality of life.
If your condition does not improve after trying these methods, book a physical visit to an orthopaedic specialist with Apollo24|7 to discuss if you are a candidate for further interventions.
Living Well with Osteoarthritis: Daily Management Tips
• Managing OA is an ongoing process. Beyond formal treatment, small daily habits can make a big difference:
• Pace Yourself: Alternate periods of activity with periods of rest to avoid overstressing your joints.
• Use Assistive Devices: Canes, shoe inserts, splints, or braces can help reduce stress on your joints.
• Choose Supportive Footwear: Shoes that provide good cushioning and support can reduce impact on your knees and hips.
• Adapt Your Home: Install grab bars in the shower, use a raised toilet seat, and keep frequently used items within easy reach.
Can Osteoarthritis Be Prevented?
While you can't completely prevent OA, you can significantly reduce your risk and slow its progression by controlling modifiable risk factors. Maintaining a healthy weight, staying active with low-impact exercises, protecting your joints from injury during sports and work, and managing blood sugar (as diabetes is a risk factor) are your best strategies for prevention.
Conclusion
Osteoarthritis is a common and challenging condition, but it doesn't have to define your life. By understanding the causes and symptoms, you can become an active participant in your care. A proactive approach, combining weight management, appropriate exercise, pain management techniques, and working closely with healthcare professionals, is the key to maintaining mobility and reducing pain. Remember, every small positive change contributes to better joint health over the long term. Listen to your body, be consistent with your management strategies, and don't hesitate to seek support. If symptoms persist beyond two weeks, consult a doctor online with Apollo24|7 for further evaluation and a personalised management plan.
Consult an Orthopaedician for the best advice
Consult an Orthopaedician for the best advice

Dr. Anil Pradeep Jadhav
Orthopaedician
23 Years • MBBS MS (Ortho)
Nashik
Apollo Hospitals Nashik, Nashik
(25+ Patients)

Dr. Rupam Chowdhury
Orthopaedician
10 Years • MBBS, DNB (Ortho.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Padam Singh Gautam
General Physician/ Internal Medicine Specialist
43 Years • M.B.B.S (WARDHA M. S.), F.A.G.E. (MANIPAL), F.A.I.M.S. (Pb.), M.A.I.M.S. (Pb.), M.R.S.H. (LONDON)
Noida
Dr Padam Singh Gautam Fracture Clinic, Noida

Dr. Suraj Prakash
Orthopaedician
5 Years • MBBS, MS (Ortho)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru

Dr. Susheel B
Orthopaedician
13 Years • MBBS, MS, Ortho Fellowship in Trauma ( Germany) Fellowship in Arthroscopy and Arthroplasty ( Switzerland)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
Consult an Orthopaedician for the best advice

Dr. Anil Pradeep Jadhav
Orthopaedician
23 Years • MBBS MS (Ortho)
Nashik
Apollo Hospitals Nashik, Nashik
(25+ Patients)

Dr. Rupam Chowdhury
Orthopaedician
10 Years • MBBS, DNB (Ortho.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Padam Singh Gautam
General Physician/ Internal Medicine Specialist
43 Years • M.B.B.S (WARDHA M. S.), F.A.G.E. (MANIPAL), F.A.I.M.S. (Pb.), M.A.I.M.S. (Pb.), M.R.S.H. (LONDON)
Noida
Dr Padam Singh Gautam Fracture Clinic, Noida

Dr. Suraj Prakash
Orthopaedician
5 Years • MBBS, MS (Ortho)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru

Dr. Susheel B
Orthopaedician
13 Years • MBBS, MS, Ortho Fellowship in Trauma ( Germany) Fellowship in Arthroscopy and Arthroplasty ( Switzerland)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
More articles from Osteoarthritis
Frequently Asked Questions
1. What is the main difference between osteoarthritis and rheumatoid arthritis?
Osteoarthritis is a degenerative 'wear and tear' condition primarily affecting cartilage. Rheumatoid arthritis is an autoimmune disease where the body's immune system attacks the lining of the joints (the synovium), causing inflammation that can damage joints and other organs.
2. What are the best exercises for knee osteoarthritis?
The best exercises are low-impact activities that strengthen the muscles around the knee without causing pain. These include swimming, water aerobics, cycling, walking, and specific strengthening exercises like leg lifts and hamstring curls.
3. Does cracking your knuckles cause osteoarthritis?
No, extensive research has not found a link between knuckle cracking and the development of osteoarthritis. The popping sound is caused by gas bubbles bursting in the synovial fluid, not by bones grinding together.
4. What foods should you avoid if you have osteoarthritis?
While no specific diet cures OA, some foods may increase inflammation. It's often recommended to limit processed foods, sugar, refined carbohydrates, and saturated fats. A Mediterranean-style diet rich in fish, fruits, vegetables, and healthy fats is generally considered beneficial for managing joint inflammation.
5. Can weather changes affect osteoarthritis pain?
Many people with OA report that their pain and stiffness worsen with changes in barometric pressure, humidity, or temperature, particularly in cold, damp weather. While the science isn't definitive, the effect is real for many sufferers.

.webp)

