Signs Of Ovarian Cancer Signs And Risk
Learn how to recognise the early signs of ovarian cancer, understand risk factors, and take proactive steps for early detection and prevention.

Written by Dr. M L Ezhilarasan
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Introduction
Ovarian cancer has long been called a "silent killer," but that label is misleading and dangerous. The truth is, it often does whisper—it sends subtle, persistent signals that are easy to dismiss as everyday digestive or menstrual issues. Knowing how to listen to your body could make a life-saving difference. This guide cuts through the noise to give you a clear, actionable understanding of the early signs of ovarian cancer and the factors that can increase your risk. We'll empower you with knowledge, from recognising the key symptoms to understanding your personal risk profile and the crucial steps to take if you're concerned. Your health advocacy starts here.
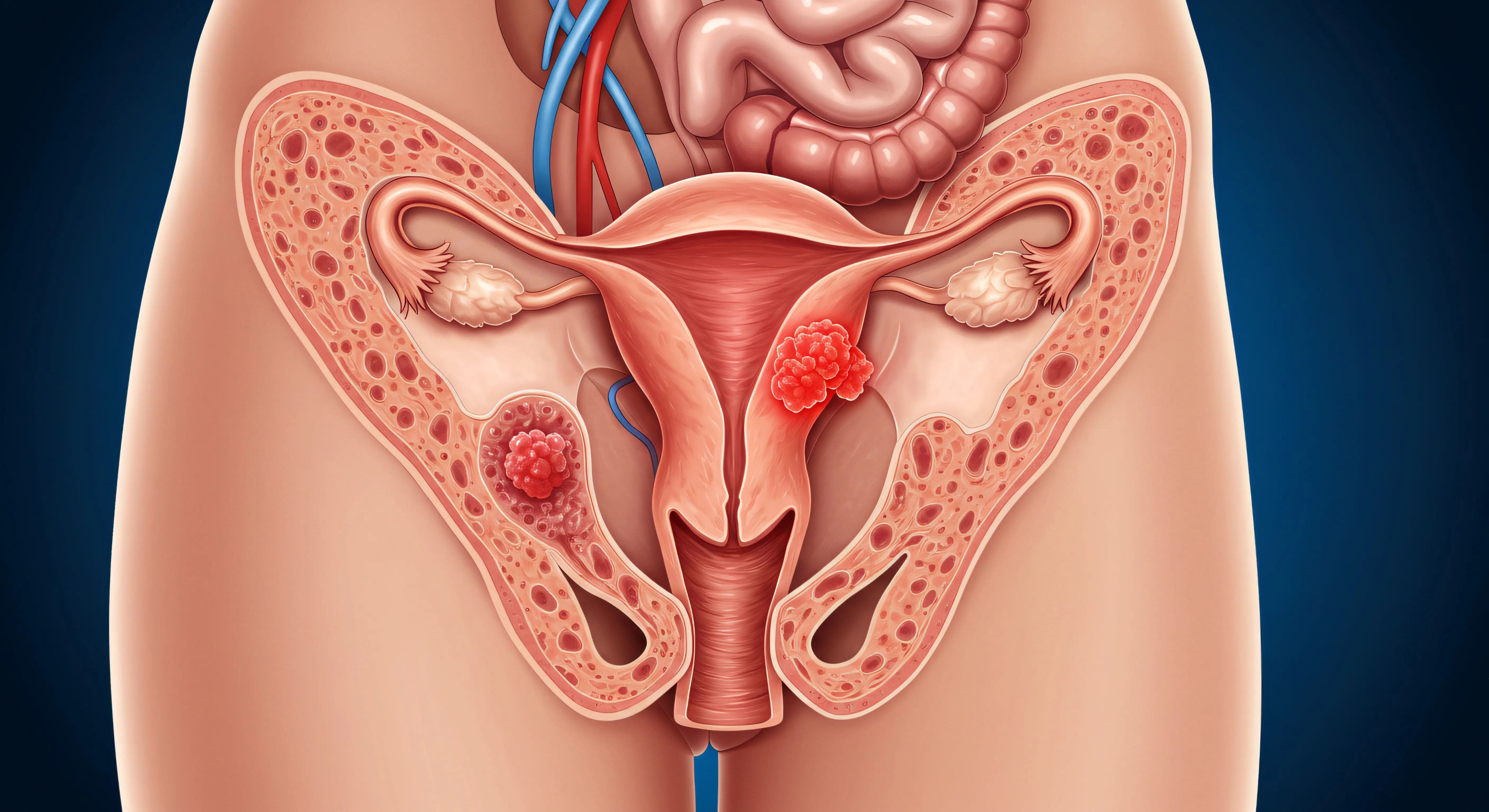
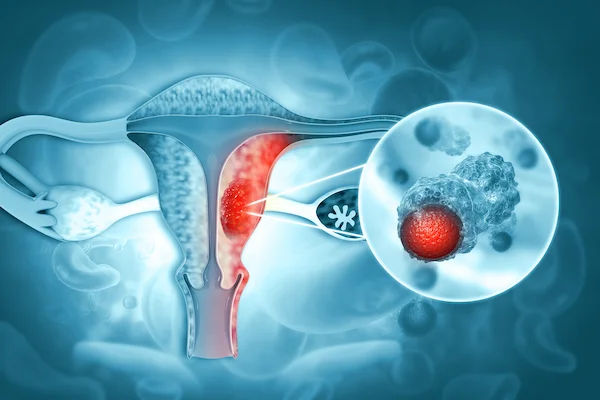
What is Ovarian Cancer? A Brief Overview
Ovarian cancer begins in the ovaries, the small, almond-shaped organs on either side of the uterus that produce eggs (ova) and the hormones oestrogen and progesterone. It occurs when abnormal cells in or near the ovaries grow and multiply uncontrollably, forming a tumour. While it is relatively rare compared to other cancers, ovarian cancer is the fifth leading cause of cancer-related deaths among women, largely because it is frequently diagnosed at an advanced stage. This late diagnosis underscores the critical importance of early detection and awareness of the initial symptoms.
The Silent Whisper: Recognising the Early Signs of Ovarian Cancer
The myth that ovarian cancer has no early symptoms is just that—a myth. Research has shown that most women do experience symptoms, even in the early stages. The challenge is that these warning signs are common and often attributed to less serious conditions like irritable bowel syndrome (IBS) or stress.
The Most Common Symptoms You Shouldn't Ignore
The key to identifying potential ovarian cancer symptoms is their persistence and change from your normal baseline. If any of the following are new, frequent (occurring more than 12 times a month), and persist for more than two weeks, it's time to see a doctor.
- Bloating: Persistent abdominal bloating or increased abdominal size.
- Feeling Full Quickly: Difficulty eating or feeling full rapidly after starting a meal (early satiety).
- Pelvic or Abdominal Pain: A constant ache or pain in the pelvis or lower abdomen.
- Urinary Symptoms: Increased urgency or frequency of urination.
Other symptoms can include unexplained fatigue, indigestion, back pain, pain during intercourse, and changes in bowel habits (constipation or diarrhoea).
How These Symptoms Are Different: Persistence and Frequency
A bad day of bloating after a big meal is normal. What isn't normal is bloating that doesn't go away and continues for weeks. This pattern of persistent and frequent symptoms is the major red flag that distinguishes potential ovarian cancer from routine digestive issues. Track your symptoms in a diary for a few weeks. Note what they are, how severe they are, and how often they occur. This data is incredibly valuable for your doctor.
The "BLOCKED" Mnemonic: An Easy Way to Remember
To make the symptoms easier to recall, remember the word BLOCKED:
- Bloating that is persistent
- Loss of appetite or feeling full quickly
- Ovarian or abdominal pain
- Changes in bathroom habits (urinary frequency, constipation)
- Knowledge (listen to your body, know what's normal for you)
- Energy loss, extreme fatigue
- Discomfort during intercourse
Who is at Risk? Understanding Ovarian Cancer Risk Factors
A risk factor is anything that increases your chance of getting a disease. Having one or more risk factors does not mean you will get ovarian cancer, but it does mean your vigilance should be higher.
Consult an Oncologist for Personalised Advice
Genetic and Family History Risks (BRCA1 & BRCA2)
This is the most significant risk factor. Approximately 15-20% of ovarian cancers are linked to inherited genetic mutations.
- BRCA1 and BRCA2 Genes: Women with mutations in these genes have a significantly higher lifetime risk of
developing both ovarian and breast cancer. - Lynch Syndrome: This inherited condition increases the risk of colorectal, endometrial, and ovarian cancer.
- Family History: Having a first-degree relative (mother, sister, daughter) with ovarian cancer raises your risk. A family history of breast, colorectal, or uterine cancer also increases risk.
Age and Reproductive History Factors
- Age: The risk of ovarian cancer increases with age. Most cases develop after menopause, with half of all diagnoses in women aged 63 or older.
- Reproductive History: Women who started menstruating early (before 12) or experienced late menopause (after 52) have a slightly higher risk. Conversely, never having been pregnant is also a risk factor.
Lifestyle and Environmental Risk Factors
- Hormone Replacement Therapy (HRT): Long-term use of oestrogen-only HRT after menopause can increase risk.
- Obesity: Having a body mass index (BMI) of 30 or higher may increase the risk of developing ovarian cancer.
- Endometriosis: This condition, where tissue similar to the uterine lining grows outside the uterus, is associated with an increased risk of certain types of ovarian cancer.
What Reduces Your Risk? Protective Factors Against Ovarian Cancer
Just as some factors increase risk, others can decrease it. These include:
- Oral Contraceptives: Using birth control pills for five or more years can reduce risk by up to 50%.
- Pregnancy and Breastfeeding: Carrying a pregnancy to term, especially before age 30, and breastfeeding can lower risk.
- Tubal Ligation or Hysterectomy: Surgical procedures like having your "tubes tied" or a hysterectomy may reduce risk.
- Healthy Weight: Maintaining a healthy weight through diet and exercise is beneficial for overall cancer prevention.
Diagnosis: What to Expect If You Have Symptoms
If your symptoms are persistent and concerning, your doctor will not jump to conclusions. The diagnostic process is methodical:
- Pelvic Exam: The doctor will physically examine your uterus, ovaries, and cervix for any lumps or changes.
- Transvaginal Ultrasound: This imaging test uses sound waves to create a picture of your ovaries and uterus to check for the size, shape, and texture of the ovaries and for any masses.
- CA-125 Blood Test: This test measures the level of a protein called CA-125 in your blood. Many women with ovarian cancer have high levels of CA-125. However, this test is not perfect, as other non-cancerous conditions can also elevate this protein.
If these tests suggest cancer, a biopsy (taking a tissue sample) is needed for a definitive diagnosis.
Action Plan: What to Do If You're Concerned
- Track Your Symptoms: Keep a detailed diary for 2-3 weeks.
- Schedule an Appointment: See your gynaecologist or primary care physician. Be specific: "I have been experiencing persistent bloating and pelvic pain for the last three weeks, and it's happening almost daily."
- Advocate for Yourself: If your concerns are dismissed but your symptoms persist, seek a second opinion. You know your body best. If symptoms persist beyond two weeks, consult a gynaecologist online with Apollo24|7 for further evaluation and to discuss the next steps.
Conclusion
Awareness is your most powerful tool in the fight against ovarian cancer. By understanding the signs and risk factors, you move from a position of fear to one of empowered knowledge. Dismissing persistent bloating or pelvic pain as "just something you ate" or "part of getting older" could mean missing a crucial window for early detection. Trust your body's signals. Have open conversations with your family about medical history. And most importantly, if something feels consistently wrong, take action by speaking with a healthcare professional. Early detection saves lives, and it starts with you listening to the whispers your body sends. If your condition does not improve after tracking your symptoms, book a physical visit to a gynaecologist with Apollo24|7 for a comprehensive examination.
Consult an Oncologist for Personalised Advice
Consult an Oncologist for Personalised Advice

Dr.sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
Dr. Sanchayan Mandal Oncology Clinic, Kolkata

Dr Gowshikk Rajkumar
Oncologist
10 Years • MBBS, DMRT, DNB in Radiation oncology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
Dr. B Shravanthi Reddy
Radiation Specialist Oncologist
8 Years • MBBS, DNB(Radiation Oncology)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
Dr. Amit Kumar Jain
Medical Oncologist
7 Years • MBBS, MD, Dr. NB (Medical Oncology)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru
Consult an Oncologist for Personalised Advice

Dr.sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
Dr. Sanchayan Mandal Oncology Clinic, Kolkata

Dr Gowshikk Rajkumar
Oncologist
10 Years • MBBS, DMRT, DNB in Radiation oncology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
Dr. B Shravanthi Reddy
Radiation Specialist Oncologist
8 Years • MBBS, DNB(Radiation Oncology)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
Dr. Amit Kumar Jain
Medical Oncologist
7 Years • MBBS, MD, Dr. NB (Medical Oncology)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru
More articles from Ovarian Cancer
Frequently Asked Questions
1. What does ovarian cancer pain feel like?
It's often described as a constant, dull ache or a feeling of pressure in the pelvis, abdomen, or lower back. It's not typically a sharp, stabbing pain that comes and goes quickly.
2. Can a Pap test detect ovarian cancer?
No. A Pap test is designed to screen for cervical cancer specifically. There is no simple, routine screening test for ovarian cancer like there is for cervical or breast cancer, which is why symptom awareness is so critical.
3. I have a family history of breast cancer. Does that affect my ovarian cancer risk?
Yes, significantly. The BRCA1 and BRCA2 gene mutations are strongly linked to both breast and ovarian cancer. If you have a strong family history of either, speak to your doctor about genetic counselling and testing.
4. Are ovarian cysts the same as cancer?
No. The vast majority of ovarian cysts are harmless (benign), fluid-filled sacs that form as part of the menstrual cycle and go away on their own. However, some complex cysts can be cancerous, which is why any persistent cyst needs to be monitored by a doctor.
5. How can I reduce my risk of ovarian cancer?
Discuss risk-reducing strategies with your doctor. These may include long-term use of oral contraceptives, maintaining a healthy weight, and, for those with a very high genetic risk, preventive surgery like removing the ovaries and fallopian tubes.


.webp)