Polycythemia Vera: A Comprehensive Patient Guide
Polycythemia vera is a rare blood cancer where the bone marrow makes too many blood cells, thickening the blood and raising clot risks. Learn its causes, symptoms, diagnosis, treatments, and tips for living well with PV.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

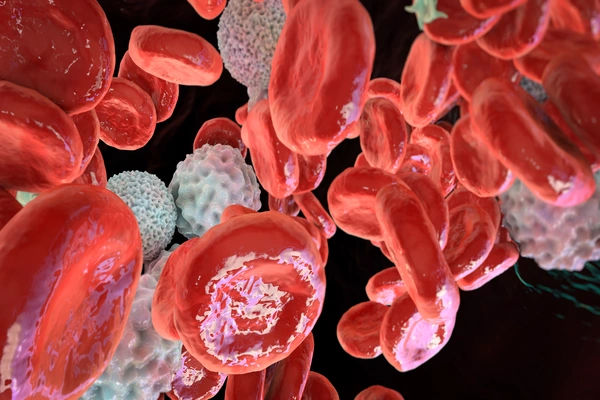
Have you or a loved one been diagnosed with polycythemia vera (PV) and feel overwhelmed by the complex medical jargon? You're not alone. Polycythemia vera is a rare, chronic blood cancer that belongs to a group of diseases known as myeloproliferative neoplasms (MPNs). In simple terms, your bone marrow goes into overdrive, producing too many red blood cells, and often too many white blood cells and platelets as well. This thickens your blood, slowing its flow and increasing the risk of serious complications like blood clots. This guide will walk you through everything you need to know—from understanding the first symptoms and getting an accurate diagnosis to exploring modern treatment options and practical tips for managing daily life. Our goal is to empower you with knowledge and hope.
What is Polycythemia Vera? The Basics Explained
At its core, polycythemia vera is a disorder of the bone marrow, the spongy tissue inside your bones where blood cells are made. Normally, this process is tightly regulated. In PV, a genetic mutation causes the marrow to overproduce blood cells, primarily red blood cells. This leads to "thick blood," or elevated hematocrit levels, which is the hallmark of the condition.
Is Polycythemia Vera a Cancer?
Yes, it is classified as a chronic blood cancer. The word "cancer" can be frightening, but it's important to understand that PV is typically a very manageable condition with proper treatment. The "neoplasm" in myeloproliferative neoplasm means a new, abnormal growth of cells—in this case, blood cells. Unlike aggressive cancers, PV often progresses slowly, and many people live with it for decades.
How PV Affects Your Blood and Body
The excess blood cells fundamentally change the properties of your blood. It becomes more viscous, like maple syrup instead of water. This thickened blood has a harder time flowing through small blood vessels, depriving tissues of oxygen. It also creates a heightened state of inflammation and increases the tendency for platelets to clump together, leading to a high risk of clotting (thrombosis) and, paradoxically, bleeding.
Recognising the Signs; Polycythemia Vera Symptoms
Many symptoms of polycythemia vera are related to the increased volume and thickness of your blood. Some people are diagnosed incidentally after a routine blood test shows abnormal levels, while others seek help after experiencing noticeable symptoms.
Common Early Warning Signs
Headaches, Dizziness, and Weakness: Caused by sluggish blood flow to the brain.
Itching after a warm shower or bath (Aquagenic Pruritus): A classic and distinctive PV symptom caused by the release of chemicals from abnormal white blood cells.
Ruddy or reddish complexion: Especially on the face, palms, and feet, due to engorgement of blood vessels.
Fatigue: Severe and persistent tiredness is one of the most common complaints.
Shortness of breath and blurred vision.
Symptoms of Advanced PV
Enlarged spleen (Splenomegaly): As the spleen works overtime to filter excess blood cells, it can enlarge, causing a feeling of fullness or pain under the left ribs.
Burning pain in the hands or feet (Erythromelalgia): Characterized by redness, warmth, and burning pain.
Gout: Caused by a high turnover of blood cells leading to elevated uric acid.
Bleeding problems, such as nosebleeds or easy bruising.
Emergency Symptoms: When to Seek Immediate Help
If you experience symptoms of a blood clot, such as sudden chest pain, shortness of breath, slurred speech, weakness on one side of the body, or severe leg pain and swelling, seek emergency care immediately. If you have been diagnosed with PV and suspect a clot, do not wait—consult a doctor online with Apollo24|7 for immediate guidance or go to the nearest emergency room.
Why Does Polycythemia Vera Happen?
The exact trigger for polycythemia vera is unknown, but it almost always starts with a genetic mutation acquired during a person's lifetime (it is not typically inherited).
Consult an Oncologist for Personalised Advice
The JAK2 Gene Mutation: The Primary Driver
In over 95% of cases, the mutation is found in the JAK2 (Janus kinase 2) gene. Think of the JAK2 gene as a "on/off" switch for blood cell production. The mutation jams this switch in the "on" position, causing the bone marrow to continuously produce blood cells without the normal regulatory signals. Testing for the JAK2 mutation is a critical part of the diagnostic process.
Getting a Diagnosis; The Polycythemia Vera Testing Process
Diagnosing PV involves a combination of tests to confirm the elevated blood counts and identify the underlying cause. If your primary care doctor notices consistently high hemoglobin and hematocrit levels in your blood work, they may refer you to a hematologist, a blood disorder specialist. Apollo24|7 offers convenient home collection for CBC tests, which are often the first indicator.
Blood Tests: The First Step
A Complete Blood Count (CBC) will show elevated red blood cell mass, often accompanied by increases in white blood cells and platelets. Your doctor will also check your EPO (erythropoietin) level; in PV, it's usually very low because the body is making cells without needing this hormone.
The Role of Bone Marrow Biopsy
While not always required for diagnosis, a bone marrow biopsy (taking a small sample from the hip bone) can show the hypercellularity (overcrowding) of the marrow and help rule out other myeloproliferative disorders.
Treatment Strategies; Managing Polycythemia Vera
The main goals of treatment for polycythemia vera are to reduce the risk of thrombosis, manage symptoms, and minimize the risk of progression. Treatment is highly personalized based on age, history of clots, and symptom burden.
Phlebotomy: The Cornerstone of Therapy
This is the first line of treatment. Similar to donating blood, a pint of blood is regularly removed from your body to lower the red blood cell count and reduce blood thickness. The goal is to achieve and maintain a hematocrit level below 45%.
Medications to Control Blood Cell Production
When phlebotomy alone isn't enough, medications are used:
Hydroxyurea: A common oral chemotherapy drug that suppresses bone marrow production.
Interferon-alpha (e.g., Ropeginterferon): A biologic therapy that helps the immune system regulate the bone marrow. It's often used in younger patients.
Ruxolitinib (Jakafi): A targeted therapy that specifically inhibits the malfunctioning JAK pathway. It's used if patients are intolerant or resistant to hydroxyurea.
Living Well with Polycythemia Vera
A diagnosis of PV means adapting to a "new normal." Focus on cardiovascular health: stay well-hydrated, engage in gentle exercise like walking to promote circulation, and adopt a heart-healthy diet low in saturated fats and purines (to help manage gout). For managing the challenging itching with PV, strategies include using pH-balanced soaps, taking cooler showers, and antihistamines.
The Emotional and Mental Health Impact
Living with a chronic cancer can lead to anxiety, depression, and "scanxiety" around regular check-ups. It's crucial to acknowledge these feelings. Seeking support from therapists, counselors, or patient support groups like the MPN Research Foundation can provide invaluable coping strategies and a sense of community.
Conclusion
Receiving a polycythemia vera diagnosis is a life-changing event, but it is far from a hopeless one. Modern medicine has transformed PV from a fatal disease into a highly manageable chronic condition. With consistent treatment, careful monitoring, and proactive lifestyle changes, the vast majority of patients can lead full, active lives. The landscape of treatment is also evolving rapidly, with new targeted therapies for JAK2 mutation offering even more hope for the future. Remember, you are the most important member of your healthcare team. Stay informed, communicate openly with your doctor, and advocate for your well-being. If your symptoms are not well-controlled or you have concerns about your treatment plan, booking a physical visit to a hematologist with Apollo24|7 can provide the specialized care you need.
Consult an Oncologist for Personalised Advice
Consult an Oncologist for Personalised Advice

Dr. Sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr.sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
Dr. Sanchayan Mandal Oncology Clinic, Kolkata

Dr Gowshikk Rajkumar
Oncologist
10 Years • MBBS, DMRT, DNB in Radiation oncology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Vishwanath S
Oncologist
8 Years • MBBS, MD, DM, Fellowship at MD Anderson Cancer Center
Bengaluru
Apollo Spectra Hospitals, Koramangala, Bengaluru

Ms. Hiba Siddiqui
Oncologist
13 Years • BA (Hons), MA, Professional Certification Psycho-oncology, PhD
Delhi
Apollo Hospitals Indraprastha, Delhi
More articles from Polycythemia vera
Frequently Asked Questions
1. What is the life expectancy for someone with polycythemia vera?
With modern treatment, the life expectancy for many PV patients can be nearly normal. The key is careful, lifelong management to prevent thrombotic complications, which are the primary cause of mortality.
2. Can polycythemia vera be cured?
The only potential cure is an allogeneic stem cell transplant, a high-risk procedure reserved for very young patients or those whose disease has transformed into acute leukemia. For most, treatment focuses on control and management rather than cure.
3. What is the difference between primary and secondary polycythemia?
Polycythemia vera is 'primary' polycythemia, caused by a problem within the bone marrow itself. Secondary polycythemia is a normal reaction to low oxygen levels (e.g., from smoking, sleep apnea, or high altitude) and EPO levels are high, not low.
4. How often is phlebotomy needed for treatment?
The frequency varies greatly. Initially, it might be weekly until the target hematocrit is reached. For maintenance, it could be every few weeks to every few months. Your hematologist will determine the schedule based on your blood counts.
5. Does PV always turn into leukemia?
No, transformation to acute myeloid leukemia (AML) is a rare complication, occurring in a small percentage of patients (estimated 2-5% over 20 years), often after many years. The risk may be slightly higher with certain treatments like hydroxyurea, but the benefit of preventing clots far outweighs this small risk.