Understanding IVF Success Rates: A Realistic Guide
Worried about IVF success rates? This comprehensive guide breaks down the statistics, explains the influencing factors, and offers practical advice to improve your chances and manage expectations on your fertility journey.

Written by Dr. Siri Nallapu
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026

Introduction
The decision to pursue in vitro fertilisation (IVF) is a significant one, often accompanied by a whirlwind of hope, anxiety, and a multitude of questions. It's completely natural to find yourself fixated on one number above all else: the success rate. If you're lying awake at night worried about IVF success rates, you are not alone. This guide is designed to demystify those statistics, moving beyond the overwhelming percentages to give you a clear, realistic understanding of what they truly mean for your unique journey. We will explore the key factors that influence outcomes, from age and embryo quality to clinic selection and lifestyle choices. Our goal is to empower you with knowledge, helping you to approach your treatment with informed confidence and a balanced perspective, transforming worry into proactive strategy.
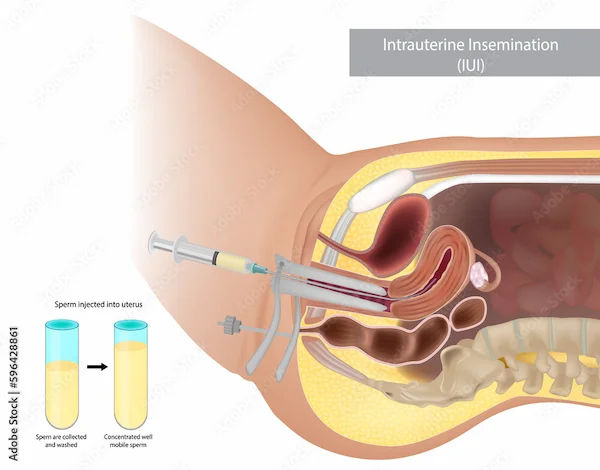
What Do IVF Success Rates Actually Measure?
When you hear a clinic quote a "60% success rate," it's crucial to understand what that percentage represents. Success in IVF can be measured in several ways, and not all metrics are created equal.
Positive Pregnancy Test
This measures the rate of a positive beta hCG blood test. It's the earliest indicator, but it doesn't account for chemical pregnancies (very early miscarriages).
Clinical Pregnancy Rate: This is confirmed by an ultrasound that shows a gestational sac. This is a more reliable metric than a positive test alone.
Live Birth Rate: This is the gold standard. It measures the percentage of cycles that result in the birth of a living child. This is the statistic you should prioritise when evaluating clinics and setting personal expectations.
The most reputable source for this data in the United States is the SART website, which collects and reports clinic-specific data. Remember, these are statistical averages across a large group of people and may not perfectly predict your individual outcome.
Consult a Gynaecologist for Personalised Advice
Key Factors That Influence Your Personal IVF Success Rate
Your personal chance of success is influenced by a combination of factors. Understanding these can help you contextualise the general statistics.
1. Age: The Single Biggest Predictor
A woman's age is the most significant factor affecting IVF success. This is because egg quality and quantity (ovarian reserve) decline with age. For example, SART data shows that for women using their own eggs:
Under 35: Average live birth rate per cycle is around 55%.
35-37: Average live birth rate drops to approximately 40%.
38-40: The rate is about 26%.
41-42: It falls to around 13%.
Over 42: Success rates are typically under 4%.
This is why many clinics encourage earlier intervention or discuss the option of donor eggs with patients over 40, which can dramatically increase the chance of success.
2. The Cause of Infertility
The underlying reason for infertility plays a role. Issues like tubal factor infertility or ovulatory disorders often have high success rates with IVF. Conditions like severe male factor infertility (requiring ICSI), endometriosis, or uterine abnormalities can present additional challenges that may slightly lower the odds per cycle.
3. Embryo Quality and Stage
Not all embryos are created equal. The development stage and grading of the embryo transferred are critical.
Blastocyst Transfer: Embryos that survive to Day 5 or 6 (blastocysts) have a higher implantation potential than Day 3 embryos.
PGT-A Testing: Preimplantation Genetic Testing for Aneuploidies screens embryos for chromosomal abnormalities. Transferring a euploid (chromosomally normal) embryo significantly increases implantation rates and reduces miscarriage risk, especially for women over 35.
4. Lifestyle and Medical History
Factors such as Body Mass Index (BMI), smoking status, alcohol consumption, and underlying medical conditions like thyroid disorders or diabetes can impact outcomes. A preconception consultation with a doctor can help optimise these factors before you start treatment.
How to Read and Compare Clinic Success Rates?
Not all clinic success rates are comparable. A high-volume clinic specialising in difficult cases might have a slightly lower rate than a clinic that only accepts ideal candidates. When reviewing SART data, look for:
Live Birth Rate for Your Age Group: This is the most important number.
Percentage of Cycles Cancelled: A high cancellation rate might indicate poor protocol personalisation.
Singleton vs. Multiple Births: A clinic with high singleton rates demonstrates a commitment to elective single embryo transfer (eSET), which is safer for mother and baby.
Freeze-All Cycles vs. Fresh Transfers: Some clinics may have higher success rates with frozen embryo transfers (FETs).
Strategies to Improve Your Odds of IVF Success
While some factors are fixed, there are proactive steps you can take to stack the odds in your favour.
Choose the Right Clinic: Do your research. Use the SART patient predictor tool and schedule consultations to find a clinic and doctor you trust.
Ask About add-ons: Inquire about the evidence behind treatments like PGT-A testing, endometrial receptivity analysis (ERA), or assisted hatching. Understand if they are recommended for your specific situation.
Focus on Preconception Health: Optimise your nutrition, maintain a healthy weight, take prenatal vitamins (especially folate), and manage stress. If you have underlying health conditions, consult a doctor online with Apollo24|7 to ensure they are well-controlled before beginning treatment.
Consider Multiple Cycles: IVF is often a process, not a single event. Cumulative success rates over 2-3 cycles are much higher than the rate for a single cycle.
Beyond the Numbers: Managing Emotional Well-Being
The emotional rollercoaster of IVF is profound. Protecting your mental health is just as important as optimising your physical health.
Set Realistic Expectations: Hope for the best, but prepare for all outcomes. Understand the statistics for your age and diagnosis.
Seek Support: Lean on your partner, join a support group (in-person or online), or consider seeing a therapist specialising in infertility.
Define Your Boundaries: Decide beforehand how many cycles you are emotionally and financially prepared for. It’s okay to take breaks.
Conclusion
Navigating the world of IVF success rates is complex, but knowledge is your greatest asset. While the statistics provide a general framework, your personal journey is unique. By understanding the factors at play—from the unchangeable, like age, to the manageable, like clinic selection and lifestyle—you can shift your focus from worry to proactive preparation. Remember, these numbers represent thousands of individual stories, and yours will have its own path. Equip yourself with information, build a strong support system, and partner with a medical team you trust.
Consult a Gynaecologist for Personalised Advice
Consult a Gynaecologist for Personalised Advice

Dr. Abhishek Daga
Obstetrician and Gynaecologist
20 Years • MBBS, MS (Obstetrics & Gynaecology)
Kolkata
Gynae Care Fertility Centre, Kolkata
(150+ Patients)

Dr. Neetu Singh
Obstetrician and Gynaecologist
19 Years • MBBS , MD (Obstetrics & Gynaecology)
Ghaziabad
Mother And Kidz Clinic, Ghaziabad
Dr. Sambana Sai Sri Neeraja
Obstetrician and Gynaecologist
6 Years • MBBS,MS (Obstetrics and gynaecology)
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Sunabha K Ghosh
Obstetrician and Gynaecologist
9 Years • MBBS, MS (Obstetrics & Gynaecology), DNB (Obstetrics & Gynaecology), MIAGE, RCOG Associate [UK]
Kolkata
Gajanan Multispeciality Clinic, Kolkata

Dr. Niti Vijay
Obstetrician and Gynaecologist
12 Years • MBBS, MD
New Delhi
THE CLINICS, New Delhi
More articles from pregnancy
Frequently Asked Questions
1. What is considered a 'good' IVF success rate?
A 'Good' rate is highly dependent on your age. For women under 35, a clinic with a live birth rate of 50% or higher per cycle is considered strong. The key is to compare a clinic's rate to the national average for your specific age bracket.
2. How many rounds of IVF does it typically take to get pregnant?
Many couples succeed in the first or second cycle. However, SART data suggests that cumulative success rates increase with each cycle, often plateauing after 3-4 cycles. The number is highly individual.
3. Does IVF work the first time?
Yes, for many people it does. The probability of IVF working the first time is highest for younger patients with no significant fertility factors. For women under 35, the national average for success on the first try is over 50%.
4. Why did my IVF fail even with good embryos?
Even high-quality embryos can fail to implant due to factors unrelated to the embryo itself, such as an unreceptive uterine lining, undiagnosed immune issues, or simply bad luck. This is often the most frustrating part of the process, and it's important to discuss a plan with your doctor for a subsequent cycle.
5. Are IVF success rates increasing?
Yes, overall success rates have steadily improved over the past two decades due to advancements in lab techniques (like blastocyst culture), embryo freezing (vitrification), and genetic screening (PGT-A).