What Leads To Signs Of Sickle Cell Disease And Types
Learn about Sickle Cell Disease, including its causes, different types, and common symptoms. Understand this genetic blood disorder to help with early recognition and better management.


Introduction
Sickle cell disease (SCD) is more than just a blood disorder; it's a lifelong genetic condition that affects millions of people worldwide. But what exactly causes the hallmark symptoms of this disease, and why does it manifest so differently from person to person? This article demystifies the complex world of sickle cell disease, breaking down the science behind what leads to its challenging signs and symptoms. We'll explore the genetic roots, the specific triggers that can cause a painful "crisis," and the different types of SCD that exist. Whether you're newly diagnosed, supporting a loved one, or simply seeking to understand this condition, this guide will provide a clear, comprehensive overview of the causes and manifestations of sickle cell disease, empowering you with knowledge and insight.
What is Sickle Cell Disease? The Basic Breakdown
At its core, sickle cell disease is a group of inherited red blood cell disorders. The central problem lies with haemoglobin, the crucial protein inside red blood cells that carries oxygen from your lungs to the rest of your body.
The Role of Haemoglobin in Red Blood Cells
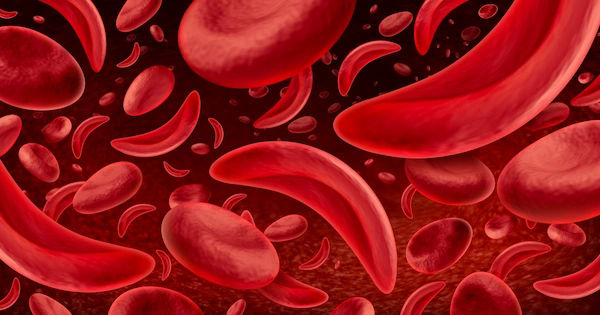
Normally, red blood cells are flexible and disc-shaped, allowing them to glide easily through even the smallest blood vessels. This flexibility is thanks to normal haemoglobin (Haemoglobin A). In sickle cell disease, a genetic mutation produces an abnormal form of haemoglobin called Haemoglobin S (HbS).
The Genetic Mutation Behind Sickle Cell
When red blood cells containing HbS release their oxygen, the abnormal haemoglobin molecules stick together and form long, rigid chains or fibers. This process causes the typically round red blood cell to contort into a stiff, sickle (or crescent) shape. These sickled cells are the root of all the problems in SCD. They are not flexible and can get stuck in small blood vessels, blocking blood flow and oxygen to tissues and organs. This blockage is the primary event that leads to the painful and damaging symptoms of the disease.
Consult a Haematologist for the best advice
The Root Cause: How Sickle Cell Disease is Inherited
SCD is not contagious; you cannot catch it like a cold. It is an inherited condition, passed down from parents to children through genes in a specific pattern called autosomal recessive inheritance.
Autosomal Recessive Inheritance Explained
A person must inherit two abnormal haemoglobin genes, one from each parent, to have sickle cell disease. If a person inherits just one abnormal gene and one normal gene, they have what is known as sickle cell trait.
Sickle Cell Trait vs. Sickle Cell Disease
This is a critical distinction. People with sickle cell trait are generally healthy carriers. They do not have the disease and usually have no symptoms, as their body produces enough normal haemoglobin to prevent sickling under most circumstances. However, they can pass the abnormal gene on to their children. If two parents with the trait have a child, there is a 25% chance with each pregnancy that the child will have sickle cell disease.
Triggers: What Causes a Sickle Cell Crisis?
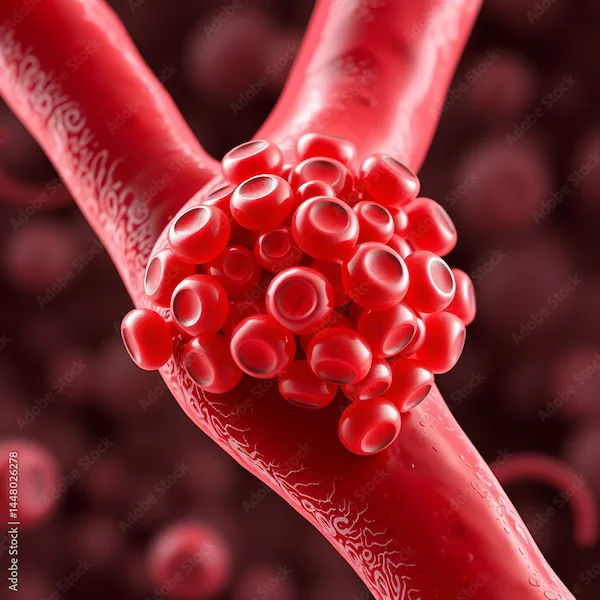
A "sickle cell crisis" or pain crisis (medically termed a vaso-occlusive crisis) is a sudden episode of severe pain that is the most common complication of SCD. While sickling can happen spontaneously, it is often triggered by specific situations.
Common Physical and Environmental Triggers
Anything that increases the body's demand for oxygen or leads to dehydration can accelerate the sickling process. Common sickle cell crisis triggers include:
- Illness: Even minor infections, colds, or the flu.
- Dehydration: Not drinking enough fluids, especially in hot weather or during physical exertion.
- Extreme Temperatures: Both very cold and very hot weather can stress the body.
- High Altitude: Where oxygen levels are lower.
- Physical Overexertion: Intense exercise without proper hydration.
The Role of Dehydration and Stress
Dehydration is a major culprit because it makes the blood more concentrated and viscous, encouraging red blood cells to sickle and clump together more easily. Emotional and physical stress can also release hormones that may contribute to the process. Understanding and avoiding these sickle cell anaemia triggers is a key part of managing the condition.
The Different Types of Sickle Cell Disease
Not all SCD is the same. The specific types of sickle cell disease depend on the genes a person inherits. The severity of the condition can vary significantly between types.
HbSS (Sickle Cell Anaemia)
This is the most common and often most severe form. It occurs when a person inherits two sickle cell genes ("S" from each parent). This is what most people think of when they hear the term sickle cell anaemia.
HbSC Disease
This is the second most common type. A person inherits one sickle cell gene ("S") and one gene for an abnormal haemoglobin called "C". Symptoms of HbSC disease are often similar to HbSS but may be milder in some individuals, though serious complications can still occur.
HbS Beta Thalassemia
This form occurs when a person inherits one sickle cell gene ("S") and one gene for beta thalassemia, another haemoglobin disorder. There are two forms: "zero" (HbS beta⁰-thalassemia), which is more severe, and "plus" (HbS beta⁺-thalassemia), which is often milder.
Rare and Less Common Types
Several other rare variants exist, such as HbSD, HbSE, and HbSO, where the second abnormal gene is something other than S, C, or beta thalassemia. The severity of these depends on the specific haemoglobin variant.
Recognizing the Signs: Symptoms of Sickle Cell Disease
Symptoms of SCD usually begin in infancy, around 5-6 months of age, and vary from person to person. They are all directly or indirectly related to anaemia and blocked blood flow.
Anaemia-Related Symptoms (Fatigue, Shortness of Breath)
Because sickled red blood cells die early (in 10-20 days instead of 120), there is a constant shortage of red blood cells, leading to chronic sickle cell anaemia. This causes:
- Fatigue and irritability
- Dizziness or lightheadedness
- Shortness of breath
- Pale skin and jaundice (yellowing of the skin or eyes)
Vaso-Occlusive Crisis (Pain Episodes)
This is the hallmark sign of sickle cell disease: episodes of severe, sudden pain that can occur anywhere in the body but are common in the chest, back, arms, legs, and abdomen. The pain occurs when sickled cells block blood flow to a region. These crises can last from hours to weeks and may require hospitalisation.
Swelling of Hands and Feet (Dactylitis)
Swelling in the hands and feet, often accompanied by pain, is often one of the first symptoms of sickle cell in infants and young children. It is caused by sickled cells blocking blood flow in the tiny bones of the hands and feet.
Frequent Infections and Vision Problems
Sickled cells can damage the spleen, an organ that helps fight infection, making individuals with SCD more susceptible to serious infections. Vision problems can arise if blood vessels in the retina become blocked.
Potential Complications of Chronic Sickling
Over time, the repeated cycles of sickling and blocked blood flow can damage tissues and organs, leading to serious complications such as stroke, acute chest syndrome (a life-threatening lung complication), organ damage (to the liver, kidneys, and heart), leg ulcers, and gallstones.
Diagnosis and When to See a Doctor
SCD is diagnosed through a simple blood test, which is now part of routine newborn screening in many countries. This early detection is crucial for beginning preventive treatments, like penicillin, to guard against infections.
If you or your child experiences symptoms of a sickle cell crisis, such as unexplained severe pain, fever, sudden weakness, or trouble breathing, it is a medical emergency. You should seek immediate care. For ongoing management and specialist support, consulting a hematologist is essential. You can consult a specialist doctor online with Apollo24|7 for an initial evaluation and guidance on managing the condition.
Get Your Health Assessed
Management and Living with Sickle Cell Disease
While there is no universal cure for all, treatments have advanced significantly. Management focuses on preventing crises, relieving symptoms, and preventing complications. This includes:
- Medications: Hydroxyurea to reduce the frequency of crises, pain relievers, and antibiotics.
- Vaccinations: Staying up-to-date to prevent infections.
- Blood Transfusions: To treat severe anaemia or prevent stroke.
- Stem Cell Transplant: The only potential cure for some eligible patients.
- Lifestyle: Staying hydrated, avoiding triggers, and eating a healthy diet.
Regular monitoring, including blood tests, is key. Apollo24|7 offers a convenient home collection for tests like CBC (Complete Blood Count) or bilirubin levels, making it easier to keep track of your health from home.
Conclusion
Understanding what leads to the signs of sickle cell disease is the first step toward effective management and empowerment. From its genetic origins to the environmental triggers that can cause a painful crisis, this condition is complex but manageable with the right knowledge and care. Advances in treatment have dramatically improved the quality of life and life expectancy for those living with SCD. By recognizing the symptoms early, avoiding known triggers, and maintaining a strong partnership with healthcare providers, individuals with sickle cell disease can lead full, active lives. If you suspect you or a family member may be at risk, especially if planning a family, seeking genetic counseling is a proactive and highly recommended step.
Consult a Haematologist for the best advice
Consult a Haematologist for the best advice

Dr Abilash Jain
General Physician/ Internal Medicine Specialist
12 Years • MBBS,DNB(FM),MNAMS,FIAMS,CCGMG(GERIATRICS),DGM (GERIATRICS),PGCD(DIABETES,BOSTON UNIVERSITY),FID(DIABETICS UK)CCEPC(PALLIATIVE CARE),CCCC(CRITICAL CARE)
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam

Dr.sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
Dr. Sanchayan Mandal Oncology Clinic, Kolkata

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)
Dr. Velu Nair
Haematologist
36 Years • MBBS, MD (Med.), FRCP, FACP, FAMS, FICP, FIACM, FUICC, FISHTM
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad
(25+ Patients)

Dr. Ramalinga Reddy
General Physician
5 Years • MBBS MD General medicine
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Consult a Haematologist for the best advice

Dr Abilash Jain
General Physician/ Internal Medicine Specialist
12 Years • MBBS,DNB(FM),MNAMS,FIAMS,CCGMG(GERIATRICS),DGM (GERIATRICS),PGCD(DIABETES,BOSTON UNIVERSITY),FID(DIABETICS UK)CCEPC(PALLIATIVE CARE),CCCC(CRITICAL CARE)
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam

Dr.sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
Dr. Sanchayan Mandal Oncology Clinic, Kolkata

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)
Dr. Velu Nair
Haematologist
36 Years • MBBS, MD (Med.), FRCP, FACP, FAMS, FICP, FIACM, FUICC, FISHTM
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad
(25+ Patients)

Dr. Ramalinga Reddy
General Physician
5 Years • MBBS MD General medicine
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
More articles from Sickle Cell Anemia disease
Frequently Asked Questions
1. Can sickle cell trait turn into sickle cell disease?
No, sickle cell trait cannot turn into sickle cell disease. They are distinct conditions. Trait means you carry one gene and are generally healthy. Disease requires two genes.
2. What is the life expectancy for someone with sickle cell anaemia today?
Thanks to advancements in treatment and comprehensive care, life expectancy has increased dramatically. Many people with SCD now live well into their 40s, 50s, and beyond.
3. Are there any specific signs of sickle cell in babies?
Yes, a key early sign in infants (around 5-6 months) is dactylitis, painful swelling of the hands and feet. Jaundice and fussiness due to anaemia are also common indicators.
4. Is sickle cell disease only found in certain ethnicities?
While it is most common in people of African, Mediterranean, Middle Eastern, and Indian ancestry, the gene mutation has occurred in populations worldwide. Newborn screening helps identify it in all infants.
5. What is the best way to prevent a pain crisis?
The best prevention is a combination of proactive measures: drinking plenty of fluids daily, washing hands to avoid infections, staying warm in cold weather, and taking prescribed medications like hydroxyurea consistently.