Understanding Bone Marrow Transplant for Sickle Cell Disease
Learn how bone marrow transplant works as a treatment for sickle cell disease, including its procedure, benefits, and potential risks.

Written by Dr. Siri Nallapu
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026

Introduction
For decades, managing sickle cell disease meant a lifelong regimen of medications, blood transfusions, and managing painful crises. But what if there was a treatment that aimed not just to manage, but to cure? Bone marrow transplant (BMT), also known as a stem cell transplant, represents this groundbreaking possibility. It's a complex and intense procedure, but for eligible patients, it can be a life-changing intervention that halts the progression of the disease. This guide will walk you through everything you need to know about bone marrow transplant as a sickle cell treatment, from who is a candidate and how the process works, to the significant risks and the profound hope it offers.
What is Sickle Cell Disease? A Quick Recap
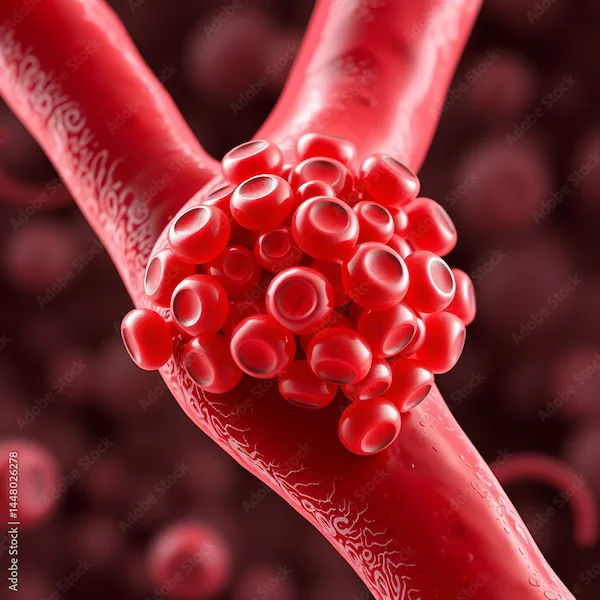
Sickle cell disease (SCD) is a group of inherited red blood cell disorders. People with SCD have atypical haemoglobin molecules, called haemoglobin S, which can cause red blood cells to become rigid, sticky, and shaped like a crescent or sickle. These sickled cells die early, causing a constant shortage of red blood cells (anaemia), and they can get stuck in small blood vessels, blocking blood flow. This blockage leads to excruciating pain, known as a pain crisis, and can cause serious complications including organ damage, strokes, and an increased risk of infection.
Why Consider a Bone Marrow Transplant?
For some patients with sickle cell disease, a bone marrow transplant offers the possibility of long-term relief and improved quality of life.
The Limitations of Standard Sickle Cell Treatments
Standard care for sickle cell disease, including hydroxyurea and regular blood transfusions, has dramatically improved life expectancy and quality of life. However, these are lifelong treatments. They manage the symptoms but do not address the root cause: the genetic mutation in the blood-forming stem cells within the bone marrow. Patients often still experience breakthrough crises, organ damage accrues over time, and treatments like transfusions carry their own risks, such as iron overload.
How a Transplant Offers a Potential Cure
A bone marrow transplant aims to replace the source of the problem. The goal is to substitute the patient's faulty blood-forming stem cells with healthy ones from a donor. These new donor cells can then produce healthy red blood cells that do not sickle, effectively curing the anaemia and preventing the complications of the disease. It is currently the only established curative treatment for sickle cell anaemia.
Consult a Haematologist for the best advice
Are You a Candidate for a Bone Marrow Transplant?
Not everyone with sickle cell disease is eligible for a bone marrow transplant, making proper evaluation essential.
The Ideal Candidate Profile
Not every person with sickle cell disease is a candidate for a BMT. The procedure is rigorous and has significant risks. Ideal candidates are often younger patients (typically under 16-18, though adult transplants are increasing) who have severe complications such as strokes, recurrent acute chest syndrome, or debilitating pain crises that are not controlled with standard treatment.
The Critical Role of the Donor: Matched Sibling Donors (MSD)
The gold standard for a donor is a healthy, fully matched sibling. Human Leukocyte Antigen (HLA) typing is used to determine if a sibling's tissue type is a compatible match. Transplants from matched sibling donors have the highest success rates, often exceeding 90%, and the lowest risk of a major complication called graft-versus-host disease (GVHD).
Expanding the Donor Pool: Haploidentical and Matched Unrelated Donors
For the 75% of patients who lack a matched sibling donor, hope is not lost. Advances in medicine have made haploidentical transplant for SCD a viable option. This uses a "half-matched" donor, such as a parent or child. While the risk of GVHD is higher, modern techniques for manipulating the donor cells and suppressing the immune system have made these transplants increasingly successful. Registries for matched unrelated donors are also an option, though finding a match can be more challenging.
The Transplant Journey: Step-by-Step
Knowing what to expect at each stage of the bone marrow transplant process can help patients and families feel more prepared.
Phase 1: Pre-Transplant Evaluation and Conditioning
This intensive phase involves a complete health workup to ensure the patient is physically strong enough for the procedure. The "conditioning" regimen involves high-dose chemotherapy, and sometimes radiation, to accomplish two things: 1) destroy the patient's diseased bone marrow, and 2) suppress their immune system to prevent it from rejecting the new donor cells.
Phase 2: The Transplant Day: An Infusion of Hope
The transplant itself is surprisingly simple and resembles a blood transfusion. The collected healthy stem cells from the donor are infused into the patient's bloodstream through a central venous catheter. The cells naturally find their way to the bone marrow cavities and begin the process of engraftment.
Phase 3: Engraftment and the Hospital Stay
The next few weeks are critical. The patient's blood cell counts will drop to very low levels, leaving them extremely vulnerable to infections and bleeding. They will need to stay in the hospital in a protective environment, receiving supportive care including antibiotics, blood transfusions, and medications. Engraftment is the milestone when the new donor cells start to grow and make healthy blood cells.
Phase 4: Recovery and Life After Transplant
Even after leaving the hospital, recovery is a slow process that can take months to a year. Close monitoring is essential to manage side effects, prevent infections, and watch for signs of GVHD. Immunosuppressant drugs are given for a period to allow the new immune system to integrate properly. Successful long-term recovery after stem cell transplant means a life free from sickle cell symptoms, though lifelong follow-up is necessary.
Weighing the Promise Against the Risks
While bone marrow transplants offer hope for curing sickle cell disease, they also come with significant risks that must be carefully considered.
Common Short-Term Side Effects and Complications
The conditioning chemotherapy causes severe side effects including nausea, vomiting, mouth sores, hair loss, and profound fatigue. The period of low blood counts carries a high risk of serious infections and bleeding.
Understanding Graft-Versus-Host Disease (GVHD)
This is a primary risk where the donor's immune cells recognise the patient's body as foreign and attack it. Graft versus host disease symptoms can range from a mild skin rash to severe, life-threatening damage to the liver, gut, and other organs. Managing GVHD is a major focus of post-transplant care.
Long-Term Considerations for Survivors
Some conditioning regimens can cause infertility. There is also a small risk of developing new cancers later in life. Certain chemotherapy drugs can affect organ function, requiring ongoing check-ups. If you are considering a transplant, consult a haematologist online with Apollo24|7 for further evaluation and to discuss your eligibility.
Beyond Traditional Transplant: The Rise of Gene Therapy
A new frontier is emerging: gene therapy. Unlike a traditional BMT, which uses donor cells, gene therapy is an autologous transplant. The patient's own stem cells are collected, genetically modified in a lab to correct the sickle cell mutation, and then reinfused. This eliminates the need for a donor and the risk of GVHD. While still largely in clinical trials, it represents the next wave of curative treatment for sickle cell anaemia.
Making the Decision: Questions to Ask Your Healthcare Team
Deciding to pursue a BMT is profound. Come prepared with questions:
- What is my predicted success rate based on my age, health, and donor type?
- What are the specific short-term and long-term risks for me?
- What does the recovery process truly look like?
- What are the alternatives, including clinical trials for gene therapy?
- What support services are available for my family and me?
Conclusion
The journey toward a bone marrow transplant for sickle cell disease is one of immense courage and hope. It is a path paved with both incredible potential for a cure and significant challenges. Understanding the rigorous process, the strict eligibility criteria, and the serious risks is the first step for any patient and family considering this option. While not the right choice for everyone, for those who are eligible and choose to proceed, it can mean a transformation from a life defined by hospital visits and pain to one of health and possibility. The landscape of sickle cell treatment is evolving rapidly, with gene therapy on the horizon, offering even more hope for the future. If you or a loved one is exploring this path, begin by having a detailed, honest conversation with a specialised healthcare provider to understand if this new beginning is within reach.
Consult a Haematologist for the best advice
Consult a Haematologist for the best advice

Dr. Thorana Prakash M
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Dr Sumanth R
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Ramalinga Reddy
General Physician
5 Years • MBBS MD General medicine
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Abilash Jain
General Physician/ Internal Medicine Specialist
12 Years • MBBS,DNB(FM),MNAMS,FIAMS,CCGMG(GERIATRICS),DGM (GERIATRICS),PGCD(DIABETES,BOSTON UNIVERSITY),FID(DIABETICS UK)CCEPC(PALLIATIVE CARE),CCCC(CRITICAL CARE)
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)
Consult a Haematologist for the best advice

Dr. Thorana Prakash M
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Dr Sumanth R
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Ramalinga Reddy
General Physician
5 Years • MBBS MD General medicine
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Abilash Jain
General Physician/ Internal Medicine Specialist
12 Years • MBBS,DNB(FM),MNAMS,FIAMS,CCGMG(GERIATRICS),DGM (GERIATRICS),PGCD(DIABETES,BOSTON UNIVERSITY),FID(DIABETICS UK)CCEPC(PALLIATIVE CARE),CCCC(CRITICAL CARE)
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)
More articles from Sickle Cell Anemia disease
Frequently Asked Questions
What is the success rate of a bone marrow transplant for sickle cell?
Success rates are highest for children with a matched sibling donor, often exceeding 90-95%. For haploidentical or unrelated donor transplants, success rates are still very good but slightly lower, typically in the 80-90% range, and depend heavily on the patient's age and overall health.
What is the cost of a bone marrow transplant for sickle cell disease?
The cost of bone marrow transplant for sickle cell is very high, often running into tens of thousands of dollars. However, many insurance plans, including Medicaid, cover the procedure when it is deemed medically necessary. Financial counselors at treatment centres can help navigate coverage and assistance programs.
Is a bone marrow transplant painful?
The transplant infusion itself is not painful. However, the side effects from the high-dose chemotherapy given beforehand, including mouth sores, nausea, and fatigue, can be very uncomfortable. The management of pain and other symptoms is a top priority for the medical team throughout the process.
Can adults with sickle cell get a bone marrow transplant?
Yes, adult bone marrow transplant is increasingly common. While historically offered mostly to children, advances in reduced-intensity conditioning regimens have made transplants safer and more accessible for adults up to their 40s and 50s, depending on their organ function and overall health.
What is the difference between a bone marrow transplant and gene therapy for sickle cell?
A traditional BMT uses stem cells from a healthy donor, which carries a risk of GVHD. Gene therapy uses the patient’s own stem cells, which are genetically modified to produce healthy haemoglobin before being reinfused, eliminating the need for a donor and the risk of GVHD. Gene therapy is still considered experimental, while BMT is an established treatment.