Guide to Neurosciences Interventional Neurology Are You Stroke Smart Calculate Your Stroke Smart Score
Know about the interventional neurology, what is brain stroke, types, causes, pro endure, what to expect during the journey and future of interventional neurology.

Written by Dr. M L Ezhilarasan
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026

Introduction
Every minute matters during a stroke. Advances in neurosciences—especially interventional neurology—have transformed stroke from a feared, untreatable emergency into a race we can often win. This guide helps you become “stroke smart”: you’ll learn how to recognise symptoms fast, understand what interventional neurology can do in the first hours, and calculate your personal Stroke Smart Score so you can lower risk starting today. We drew on top-ranking resources and the latest evidence from major stroke organisations to make this simple, practical, and actionable for the general public seeking reliable healthcare advice. If you or a loved one shows signs of stroke, call emergency services immediately. For prevention, risk checks, or follow-up care, you can consult a doctor online with Apollo24|7.
Consult Top Neurology for Personalised Advice
Neurosciences and Interventional Neurology Explained
Interventional neurology, also called neurointerventional surgery or interventional neuroradiology, is a subspecialty within neurosciences that treats conditions of the brain, head and neck, and spine using minimally invasive, image-guided procedures. Instead of opening the skull, interventional neurologists and neurointerventional surgeons typically use tiny catheters inserted through a small puncture in the wrist or groin to navigate blood vessels and treat problems from inside the body.
How is this different from neurology and neurosurgery? A neurologist diagnoses and manages neurological disorders primarily with medications and non-surgical strategies. A neurosurgeon performs open surgeries, such as removing tumours or repairing complex skull and spine problems. Interventional neurology sits in between: it uses endovascular (inside-the-vessel) tools to treat strokes, aneurysms, arteriovenous malformations (AVMs), carotid artery disease, and certain types of brain or spine bleeding, often in collaboration with neurologists and neurosurgeons.
Common conditions treated include:
1. Acute ischemic stroke due to large vessel occlusion (LVO), where a clot blocks a major artery to the brain.
2. Brain aneurysms, treated with coil embolisation or flow diverters to prevent rupture.
3. AVMs or fistulas, treated with targeted embolisation.
4. Carotid artery stenosis, treated with stenting in selected patients.
5. Intracranial atherosclerosis, selected embolisations for chronic subdural hematoma, and others.
Why it matters: In stroke care, interventional neurology is a game-changer. For many patients, clot retrieval (mechanical thrombectomy) dramatically increases the chance of walking independently after a severe stroke compared to clot-busting medication alone.. This is the “interventional neurology/are you stroke smart” connection: recognising stroke fast gets you to a team that can often reverse damage if you arrive within the right time window.
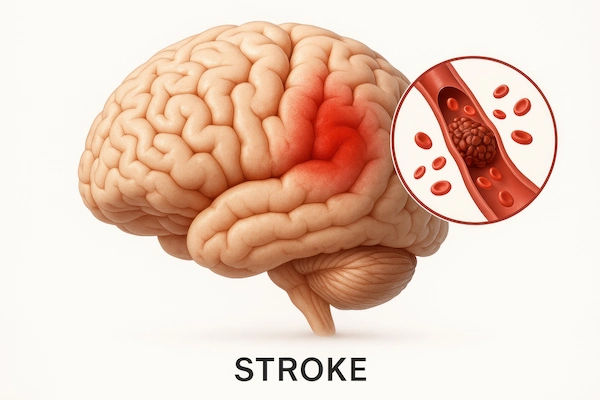
Stroke: Types, Causes, and Why “Time Is Brain”
Most strokes are ischemic, meaning a clot blocks blood flow to part of the brain. The rest are hemorrhagic, caused by bleeding into the brain from a ruptured vessel or aneurysm. A transient ischemic attack (TIA) is a short-lived “mini-stroke” with stroke-like symptoms that resolve within 24 hours—often within minutes. Treat TIAs as emergencies: they warn of a high short-term risk of a full stroke.
Causes and risks: High blood pressure is the number one modifiable risk for stroke. Others include diabetes, high cholesterol, smoking, atrial fibrillation (AFib), carotid artery disease, obesity, inactivity, and certain conditions like sickle cell disease. Family history, age, and sex also play roles; women have unique risks related to pregnancy, hormonal therapies, and migraines with aura [6].
Why time is brain: Without oxygen, brain cells begin to die within minutes. A widely cited analysis estimates that an untreated stroke destroys approximately 1.9 million neurons each minute [1]. That’s why the mantra is “recognise and run”—get to the nearest stroke-ready hospital immediately. In the first 4.5 hours, clot-dissolving medication (IV thrombolysis) can improve outcomes for many ischemic strokes. For severe ischemic strokes from large clots (LVO), mechanical thrombectomy can salvage threatened brain tissue up to 6 hours—and, in carefully selected patients, up to 24 hours from last time known well [3,4,5]. Hemorrhagic strokes require rapid blood pressure control, reversal of blood thinners when appropriate, and sometimes neurointerventional techniques or surgery.
Are You Stroke Smart? Recognise Symptoms FAST (and BE-FAST)
You become “stroke smart” by recognising symptoms fast and calling emergency services immediately.
1. FAST is the simplest memory aid recommended widely:
2. Face: Is one side drooping?
3. Arm: Is one arm weak or drifting down?
4. Speech: Is speech slurred or strange?
5. Time: If you see any of these, it’s time to call emergency services now. Do not wait. Do not drive yourself.
BE-FAST adds two symptoms many people miss:
1. Balance: Sudden loss of balance or coordination.
2. Eyes: Sudden vision changes—double vision or loss of vision in one or both eyes.
Other warning signs include sudden confusion, severe headache with no known cause (especially concerning for bleeding), sudden numbness or weakness (particularly on one side), dizziness, and trouble understanding or walking. If you’re unsure, act. It’s safer to be evaluated and discharged than to lose precious time. Remember: symptoms that come and go (TIA) still demand urgent assessment to prevent a larger stroke.
Calculate Your Stroke Smart Score
Use this two-part score to see both your stroke risk and your readiness to respond. It’s for education only and does not replace medical evaluation or guideline-based calculators.
Part A—Personal Risk Score (0–24 points)
1. Score yourself based on the items below:
2. Age: 55–64 (1), 65–74 (2), 75+ (3)
3. Blood pressure: Diagnosed hypertension or on meds (3); borderline high without meds (1); normal (0)
4. Diabetes or HbA1c ≥6.5%: Yes (3); Prediabetes/HbA1c 5.7–6.4% (1); No (0)
5. Smoking: Current (3); Quit within 5 years (1); Never/quit >5 years (0)
6. Atrial fibrillation/flutter: Yes (4); No/Unsure (0) Note: If unsure, ask about screening.
7. Cholesterol: LDL ≥160 or on statin for high LDL (2); Borderline (1); Optimal (0)
8. Physical inactivity: <150 minutes/week moderate activity (1); ≥150 minutes/week (0)
9. Obesity: BMI ≥30 (1); <30 (0)
10. Sleep apnea diagnosed or suspected (snoring, daytime sleepiness): Yes (1); No (0)
11. Prior TIA or stroke: Yes (5); No (0)
Part B—Action & Preparedness Score (0–10 points)
1. Know FAST/BE-FAST cold: Yes (2); Partly (1); No (0)
2. Emergency plan saved (ICE contact, nearest stroke centre, transport plan): Yes (2); Partly (1); No (0)
3. Medication list accessible (on phone or wallet): Yes (1); No (0)
4. Blood pressure checked at least monthly at home or clinic: Yes (2); Sometimes (1); No (0)
5. Regular check-ups for diabetes/cholesterol/AFib as applicable: Yes (2); Sometimes (1); No (0)
6. Home risks minimised (no driving self in emergencies, family informed): Yes (1); No (0)
Your total Stroke Smart Score = Risk (0–24) + Action (0–10) = 0–34
Interpretation:
1. 0–8: Low current risk/readiness concerns. Keep up healthy habits, refresh emergency plan.
2. 9–16: Moderate. Address modifiable risks and tighten your action plan in the next 30 days.
3. 17–24: High. Work with your clinician to aggressively manage risks; complete your emergency plan this week.
4. 25–34: Very high. Seek a personalised prevention strategy now; ensure family knows the plan; consider screening for AFib and sleep apnea.
What to do next:
1. Share your results with your doctor. If you haven’t had recent checks for BP, HbA1c, and lipids, consider booking tests. Apollo24|7 offers home collection for tests like HbA1c and lipid profiles, which can make this easy.
2. If you have symptoms suggestive of atrial fibrillation (palpitations, irregular pulse) or your smartwatch alerts to irregular rhythm, ask about an ECG or ambulatory monitoring.
3. Update your action plan: rehearse what to do, who to call, and where to go.
How Interventional Neurology Treats Stroke Today
Two time-critical treatments can restore blood flow in many ischemic strokes:
1. IV thrombolysis (clot-busting medication)
2. What it is: A medication (alteplase; increasingly tenecteplase in some centres) given into a vein to dissolve the clot. It’s most effective when started as early as possible, within 4.5 hours for many patients.
3. Tenecteplase vs alteplase: Some studies suggest tenecteplase (a single bolus injection) may be as effective or better than alteplase in certain scenarios, with practical advantages for speed of delivery. Protocols vary by country and hospital.
4. Not for everyone: It’s only for ischemic stroke and has inclusion/exclusion criteria (such as certain bleeding risks) determined by the stroke team.
Mechanical thrombectomy (clot retrieval)
1. What it is: A neurointerventional procedure that threads a catheter through an artery to the brain to pull out or aspirate a large clot causing a severe stroke (LVO). It dramatically improves the odds of independence when performed quickly in eligible patients.
2. Treatment window: Strong evidence supports thrombectomy up to 6 hours from onset, and with advanced imaging selection, up to 16–24 hours in selected patients (DAWN and DEFUSE 3). This is where interventional neurology excels.
3. Imaging selection: CT perfusion or MRI can identify salvageable brain tissue (“penumbra”) to guide late-window decisions.
Beyond acute stroke, interventional neurology treats:
1. Aneurysms with coils or flow diverters to prevent rupture.
2. Carotid artery disease with stenting in carefully selected patients (an alternative to surgical endarterectomy).
3. AVMs and dural arteriovenous fistulas with targeted embolisation.
Who benefits most from thrombectomy?
Patients with large vessel occlusions (e.g., internal carotid, proximal middle cerebral artery) and severe deficits benefit most, especially when reperfusion is achieved quickly [2–5]. Your stroke team decides eligibility based on clinical severity, imaging, timing, and comorbidities.
What to Expect: Before, During, and After a Neurointerventional Procedure
Before
Rapid imaging: Most centres perform a non-contrast CT to rule out bleeding, CT angiography to spot a large clot, and often CT perfusion to assess salvageable brain tissue.
Consent and preparation: If thrombectomy is indicated, the team prepares the neurointerventional suite while stabilising blood pressure and oxygen and coordinating anaesthesia (often moderate sedation, sometimes general anaesthesia).
During
Access: A small puncture in the wrist (radial) or groin (femoral) allows a thin catheter to be guided under X-ray to the brain.
Clot removal: Devices such as stent retrievers or large-bore aspiration catheters remove the clot. The goal is successful reperfusion (often graded as TICI 2b/3).
Time: Many procedures last 30–90 minutes, depending on anatomy and clot complexity.
After
ICU-level monitoring for the first 24 hours is common.
Early rehab starts as soon as the patient is stable; this “first 48 hours” is vital for long-term recovery.
Secondary prevention: blood pressure control, antiplatelets or anticoagulation (e.g., for AFib), cholesterol-lowering therapy, diabetes optimisation, smoking cessation, and lifestyle interventions.
Preventing Stroke: Your Everyday Playbook
1. Blood pressure: Aim for individualised targets per your clinician; generally, less than 130/80 mmHg is beneficial for many at risk. Home monitoring is powerful—check at the same time daily. Apollo24|7 offers home devices and consults to adjust medication when needed.
2. Diabetes: Keep HbA1c in your target range; ask about continuous glucose monitoring if appropriate. Home collection for HbA1c through Apollo24|7 can simplify tracking.
3. Atrial fibrillation: If you have AFib, anticoagulation is often key to preventing stroke. Do not stop blood thinners without medical advice.
4. Cholesterol: Many high-risk patients benefit from statins; some need additional agents. A lipid profile helps guide decisions.
5. Lifestyle pillars
6. Nutrition: Embrace a Mediterranean-style pattern—vegetables, fruits, whole grains, legumes, nuts, fish; limit processed foods and added sugars.
7. Activity: Target at least 150 minutes/week of moderate activity plus 2 days of strength training. Even 10-minute bouts count.
8. Sleep and apnea: Treat snoring and daytime sleepiness seriously—screening and treatment for obstructive sleep apnea can reduce cardiovascular risk.
9. Tobacco and alcohol: Quit smoking (ask about medications and counselling). If you drink, keep it moderate.
When to Seek Care and How Apollo24|7 Can Help
1. Emergencies: If you suspect stroke, call emergency services immediately. Do not drive yourself.
2. Non-emergency prevention and follow-up: If you have stroke risk factors, symptoms that concern you, or a family history of stroke, consult a doctor online with Apollo24|7 for risk assessment, medication review, or referrals. If symptoms persist beyond two weeks or you have difficulty controlling blood pressure, book a physical visit to a doctor with Apollo24|7.
3. Tests made easy: Apollo24|7 offers convenient home collection for tests like HbA1c, fasting lipid profile, and thyroid or vitamin D as needed—useful for prevention check-ins.
4. Choosing a hospital: Prefer a primary or comprehensive stroke centre with 24/7 neuroimaging, thrombolysis capability, and access to mechanical thrombectomy. Ask about door-to-needle and door-to-groin times, and if they participate in quality programs (e.g., stroke certifications).
The Future of Interventional Neurology
1. AI imaging: Automated CT/MRI perfusion analysis speeds decisions in the ambulance or emergency department, supporting late-window thrombectomy triage.
2. Mobile stroke units: Ambulances equipped with CT scanners and telemedicine can deliver thrombolysis pre-hospital in some cities, shrinking treatment times.
3. Next-generation drugs: Tenecteplase is gaining traction; research explores better clot-dissolvers and neuroprotectants.
4. Devices and techniques: Faster catheters, aspiration pumps, and tailored anaesthesia strategies continue to improve outcomes.
5. Integrated systems of care: Pre-notification by EMS, “hot stroke” protocols, and post-acute rehab paths create smoother journeys from door to recovery.
Conclusion
Becoming stroke smart means two things: knowing the signs and knowing your personal risk. When symptoms strike, every minute counts—call emergency services and head to a stroke-ready hospital where interventional neurology teams can deliver clot-busting drugs and, when needed, remove large clots to restore blood flow. Between emergencies, prevention is powerful. Calculate your Stroke Smart Score, fix what you can (blood pressure, diabetes, AFib, cholesterol, smoking), and refresh your action plan with family. If you need guidance, consult a doctor online with Apollo24|7 for a personalized prevention strategy, and consider convenient home collection for important tests like HbA1c and lipid profiles. Neurosciences and interventional neurology are advancing rapidly; your best outcomes come from quick action, smart prevention, and a prepared plan you practice today—before you ever need it.
Consult Top Neurology for Personalised Advice
Consult Top Neurology for Personalised Advice

Dr. Aditendraditya Singh Bhati
Neurosurgeon
21 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Skull Base Endoscopy (Italy), Fellow Extended Skull Base ( Weill Cornell, USA), Fellow ZAP-X Radiosurgery. Member of American Association of Neurological Surgeons
Delhi
Apollo Hospitals Indraprastha, Delhi
(125+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Anusha D
Neurologist
16 Years • MBBS, MD, DM (Neuro), DNB (Neuro)
Chennai
Apollo Speciality Hospitals OMR, Chennai
(125+ Patients)
Consult Top Neurology for Personalised Advice

Dr. Aditendraditya Singh Bhati
Neurosurgeon
21 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Skull Base Endoscopy (Italy), Fellow Extended Skull Base ( Weill Cornell, USA), Fellow ZAP-X Radiosurgery. Member of American Association of Neurological Surgeons
Delhi
Apollo Hospitals Indraprastha, Delhi
(125+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Anusha D
Neurologist
16 Years • MBBS, MD, DM (Neuro), DNB (Neuro)
Chennai
Apollo Speciality Hospitals OMR, Chennai
(125+ Patients)
More articles from Stroke
Frequently Asked Questions
1) What’s the difference between a TIA and a stroke?
TIA causes stroke-like symptoms that resolve within 24 hours, often minutes. It’s a warning sign of high short-term risk. Seek immediate care; do not ignore a “mini-stroke.”
2) How long after stroke can treatment work?
IV thrombolysis works best within 4.5 hours for many ischemic strokes. Mechanical thrombectomy benefits many patients up to 6 hours and, with imaging selection, up to 16–24 hours after last known well. Call emergency services immediately.
3) Is tenecteplase better than alteplase?
Evidence suggests tenecteplase is at least as effective in some settings and easier to give (single bolus), but protocols differ by hospital and region.. Your stroke team will choose the best option.
4) How can I lower my stroke risk at home?
Control blood pressure, manage diabetes, treat AFib, optimize cholesterol, stop smoking, stay active, and sleep well. Use home BP checks and consider Apollo24|7 home collection for HbA1c and lipid panels to track progress.
5) How do I choose a hospital for stroke?
Look for a primary or comprehensive stroke center with 24/7 imaging, thrombolysis, and access to mechanical thrombectomy. EMS can often route you directly to the best-equipped center.