Guide to Neurosciences Interventional Neurology/harmless Neck Massage Could Cause Stroke
Learn the real connection between neck massage and stroke risk. Understand how cervical artery dissection occurs, recognise warning signs, and explore how interventional neurology provides life-saving treatments. Practical safety guidance and prevention advice for everyday neck care.


Introduction
Neck stiffness is a common problem—and many of us instinctively stretch, massage, or even perform a quick “neck crack” to find relief. However, alarming headlines sometimes claim that a “simple neck massage could cause a stroke.” So, what’s the real risk? And how does interventional neurology, the minimally invasive branch of neuroscience focused on blood vessel disorders of the brain and spine, fit into this discussion?
In this clear, myth-busting guide, we explore how strokes can (rarely) occur after certain neck manipulations, what symptoms to watch for, and how modern interventional neurology can save brain tissue when every minute counts. You’ll learn the difference between gentle massage and high-velocity neck manipulation, who might be at greater risk for cervical artery dissection, how the condition is diagnosed, and the latest treatments—from medication to mechanical thrombectomy.
If you enjoy massage and stretching, there’s no need to panic. Serious complications are uncommon. But being informed about the warning signs and making safer choices can help protect you or someone you care about. Let’s explore the science, safety, and practical decisions that matter most.
Interventional Neurology: Where Neurosciences Meet Stroke Care
Interventional neurology (also known as endovascular neurosurgery or interventional neuroradiology) treats blood vessel problems of the brain and spine from within the arteries, using imaging and micro-catheters rather than open surgery.
Consult Top Neurologists for Personalised Advice
Key Procedures in Interventional Stroke Care
- Mechanical thrombectomy: Physical removal of a clot using a stent-retriever or suction catheter, usually within six hours, but sometimes up to 24 hours in carefully selected cases.
- Intra-arterial medication: Targeted delivery of clot-busting drugs directly to the blockage.
- Aneurysm treatment: Coil embolisation or flow-diversion stents to treat or prevent bleeding.
- Arterial stenting: Used in certain cases of vessel narrowing or dissection complications.
Why This Matters
If a rare cervical artery dissection leads to stroke, interventional neurologists play a vital role in both diagnosis (via angiography) and treatment (thrombolysis or thrombectomy). Coordinated stroke networks ensure rapid intervention—because “time is brain.”
A unique insight: Modern imaging can now identify patients with viable brain tissue, allowing thrombectomy to benefit some people even if they wake up with symptoms.
Neck Massage and Stroke Risk: Sorting Fact from Fear
What the Evidence Shows
Routine, gentle massage is extremely unlikely to cause a stroke. The concern mainly relates to rapid, high-velocity neck
manipulations, which have, in rare cases, been linked to cervical artery dissection, leading to stroke.
Large studies show that people who experience a vertebrobasilar stroke often visit a chiropractor or GP for neck pain
beforehand—suggesting the dissection itself may have caused the pain, prompting the visit, rather than the manipulation
being the cause.
Nevertheless, professional guidelines recommend caution and avoiding high-velocity manoeuvres in those with warning signs.
Key Distinctions
- Gentle soft-tissue massage ≠ high-velocity rotational thrusts.
- Avoid deep pressure over the front or sides of the neck (where major arteries lie).
- Pain that is new, severe, or unusual should be checked before any manipulation.
Unique insight: Many people with dissection recall a distinctive, sudden neck pain before neurological symptoms—pain can be a warning, not an effect.
Cervical Artery Dissection Explained: The Mechanism Behind Rare Stroke After Neck Manipulation
What Is Cervical Artery Dissection (CAD)?
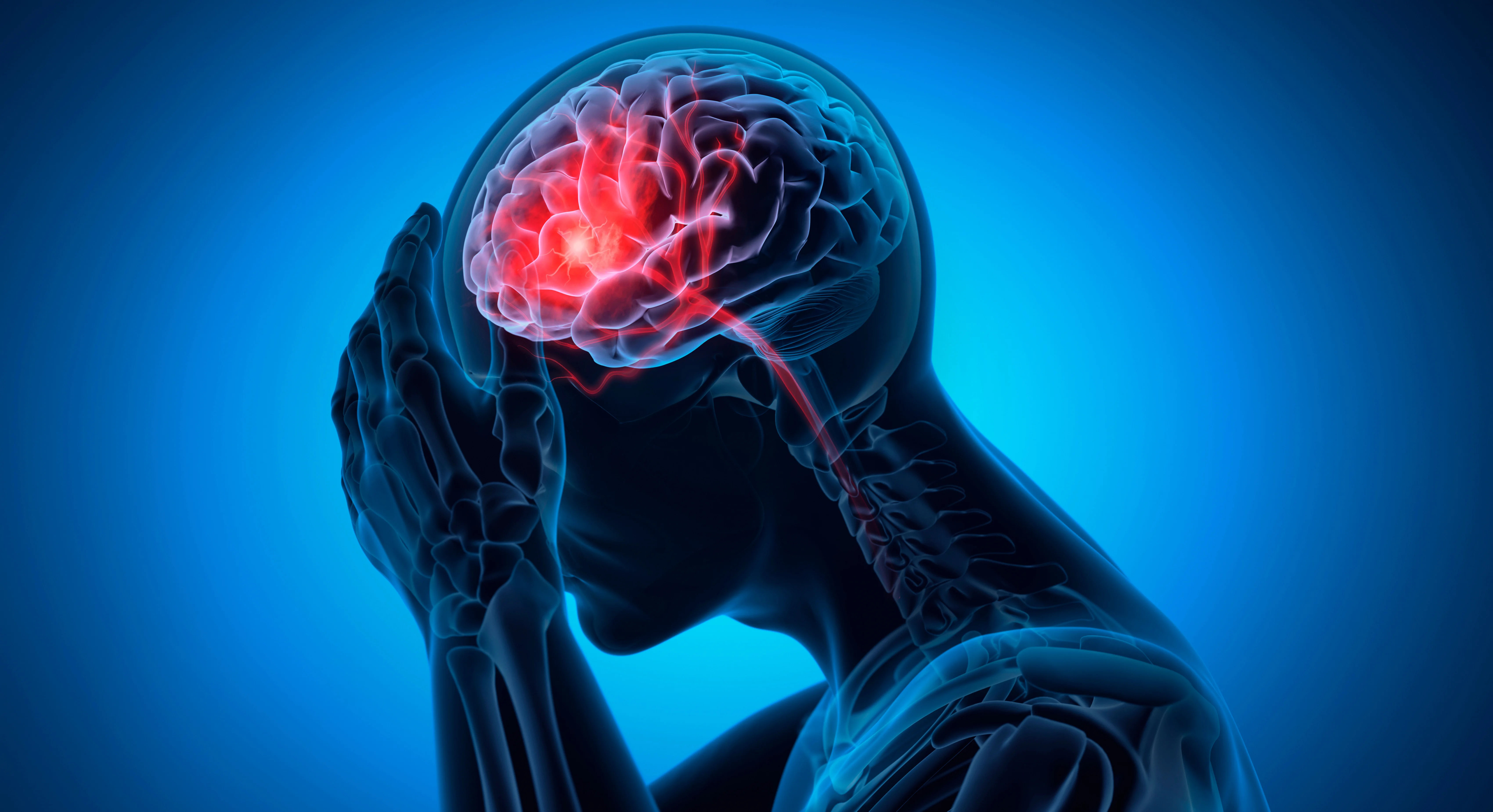
CAD occurs when a small tear develops in the inner wall (intima) of a neck artery—most often the internal carotid or
vertebral artery. Blood enters the wall, creating a “false channel” (intramural haematoma) that can narrow the vessel or
form clots, which may travel to the brain and cause a transient ischaemic attack (TIA) or a stroke.
Carotid vs Vertebral Artery Dissection
- Carotid artery: Typically causes facial or eye pain, Horner’s syndrome (droopy eyelid, small pupil), and strokes
affecting the front part of the brain. - Vertebral artery: More often causes sudden one-sided neck pain and posterior-circulation symptoms—dizziness, double vision, slurred speech, or imbalance.
Who’s at Risk?
- Connective tissue disorders (e.g. Ehlers-Danlos syndrome) and fibromuscular dysplasia.
- Migraine, high blood pressure, infection, or smoking.
- Sudden neck movements, sports injuries, or manipulation—but sometimes no clear cause at all.
How a Dissection Causes Stroke
- A tear in the artery wall allows blood to enter.
- The false lumen narrows the vessel or forms a flap.
- A clot forms and travels to the brain.
Unique insight: CAD is one of the main causes of stroke in healthy adults under 50. “Neck pain plus neurological signs” should always prompt urgent assessment.
Recognising Red Flags and Acting Fast
H3: Warning Signs for Dissection or Stroke
- Sudden, severe, one-sided neck pain or headache.
- Dizziness, double vision, imbalance, speech difficulty, or facial droop.
- Droopy eyelid with a small pupil (Horner’s syndrome).
- Severe nausea or vomiting alongside neurological symptoms.
H3: Remember FAST
- Face: Droop or uneven smile.
- Arms: Weakness or drift.
- Speech: Slurred or strange.
- Time: Call emergency services immediately.
When to Seek Help
- Any FAST signs or “first/worst” neck pain with neurological changes → Emergency.
- Mild stiffness improving with rest → monitor, but seek advice if persistent for more than two weeks.
Unique insight: Posterior-circulation strokes may cause dizziness and imbalance rather than facial droop or arm weakness. Treat sudden, severe dizziness as a potential stroke until proven otherwise.
Diagnosis and Tests: How Doctors Confirm Dissection or Stroke
Imaging and Evaluation
- CT angiography (CTA): Fast, accurate, and widely available.
- MR angiography (MRA): No radiation and excellent vessel detail.
- MRI brain: Detects early stroke changes.
- Doppler ultrasound: Useful for carotids but limited for vertebral arteries.
Laboratory tests check cholesterol, blood sugar, clotting profile, and kidney function.
For preventive screenings, Apollo24|7 offers home collection for lipid profile and HbA1c tests.
What to Expect in the Hospital
- If stroke is suspected, imaging and treatment decisions happen simultaneously.
- Confirmed dissections without major stroke usually start on antiplatelet or anticoagulant medication, followed by repeat imaging.
Unique insight: Some dissections can appear normal on early scans; repeat imaging is vital if symptoms continue.
Treatment Options: Medication and Interventional Neurology Procedures
Medication
- Antiplatelets (aspirin) or anticoagulants (heparin, warfarin, or DOACs) for three to six months help prevent clots and allow healing.
- Choice of treatment depends on anatomy, stroke severity, and bleeding risk.
Acute Stroke Treatments
- Thrombolysis (tPA or tenecteplase): Clot-busting drugs given within the eligible window.
- Mechanical thrombectomy: Interventional neurologists can remove large clots, restoring blood flow—even up to 24 hours later in selected cases.
When Stenting Is Considered
- Persistent narrowing, pseudoaneurysm, or recurrent emboli despite medication may require endovascular stenting.
Unique insight: Most dissections heal naturally within months, and many patients make a full recovery with medication alone.
Prevention and Safe Neck Care: Practical Tips and Choosing Practitioners
Safer Self-Care
- Avoid high-velocity “cracking.”
- Use gentle stretches, posture correction, and upper-back mobility exercises.
- Manage blood pressure and avoid smoking.
Choosing the Right Practitioner
- Check qualifications and experience.
- Share your medical history, including connective tissue disorders or migraines.
- Request low-force techniques and decline high-velocity neck manipulations.
Informed Consent and Screening
A responsible practitioner will:
- Screen for red flags.
- Pause treatment if neurological symptoms arise.
- Recommend urgent evaluation when necessary.
If symptoms persist or you’re uncertain, book a consultation with Apollo24|7 for a professional assessment or referral.
Unique insight: Much neck discomfort stems from tightness in the upper back or chest muscles. Improving posture often
eases neck tension without manipulation.
Conclusion
Neck tension is part of modern life, and most gentle self-care—stretching, heat, and soft-tissue massage—is safe and
effective. The rare cases of stroke after neck manipulation are mainly linked to high-velocity techniques that can cause cervical artery dissection, not ordinary massage.
Understanding your risks, recognising warning signs, and acting fast are crucial. If you or someone you know experiences sudden severe neck pain or neurological symptoms such as dizziness, imbalance, or slurred speech, seek emergency medical help. Interventional neurology provides life-saving options such as mechanical thrombectomy that can restore blood flow and prevent brain damage.
The good news is that most dissections heal with medication and time. Avoid forceful “cracking,” prioritise good posture, and manage blood pressure and other risk factors. If neck symptoms persist or you’re worried, consult a doctor online or in person through Apollo24|7 for expert advice and care.
Consult Top Neurologists for Personalised Advice
Consult Top Neurologists for Personalised Advice

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Avinash Gupta
Neurologist
12 Years • MBBS, DNB - Neurology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Aditendraditya Singh Bhati
Neurosurgeon
21 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Skull Base Endoscopy (Italy), Fellow Extended Skull Base ( Weill Cornell, USA), Fellow ZAP-X Radiosurgery. Member of American Association of Neurological Surgeons
Delhi
Apollo Hospitals Indraprastha, Delhi
(125+ Patients)

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
Consult Top Neurologists for Personalised Advice

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Avinash Gupta
Neurologist
12 Years • MBBS, DNB - Neurology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Aditendraditya Singh Bhati
Neurosurgeon
21 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Skull Base Endoscopy (Italy), Fellow Extended Skull Base ( Weill Cornell, USA), Fellow ZAP-X Radiosurgery. Member of American Association of Neurological Surgeons
Delhi
Apollo Hospitals Indraprastha, Delhi
(125+ Patients)

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
More articles from Stroke
Frequently Asked Questions
1) Can a neck massage cause a stroke?
A gentle massage is highly unlikely to cause a stroke. Rare cases have been linked to high-velocity neck manipulations that may cause artery dissection. Request low-force techniques and avoid thrusting movements.
2) What are the early signs of vertebral artery dissection?
Suddenly, one-sided neck pain or a new severe headache, often accompanied by dizziness, imbalance, or double vision. Seek immediate emergency medical attention.
3) How is cervical artery dissection diagnosed?
With CT angiography or MR angiography, sometimes alongside a brain MRI. Doppler ultrasound can aid in the diagnosis of carotid dissections.
4) What treatment is used—blood thinners or aspirin?
Both anticoagulants and antiplatelets may be prescribed for three to six months; your doctor will choose the most suitable option based on your situation.
5) Is mechanical thrombectomy possible if stroke symptoms began many hours ago?
Yes. In selected patients with large-vessel blockage and viable brain tissue, thrombectomy can be effective up to 24 hours after symptoms begin.
.webp)
.webp)